Large Medicare Analysis Reopens Debate Over Multivessel Revascularization
Some surgeons at STS argue the data, showing stark mortality reductions with CABG, should spark a rethink of the guidelines.
SAN DIEGO, CA—Among Medicare patients with ACS undergoing CABG or PCI for multivessel CAD, surgery appears to be associated with lower mortality and fewer complications, according to a large contemporary observational data set.
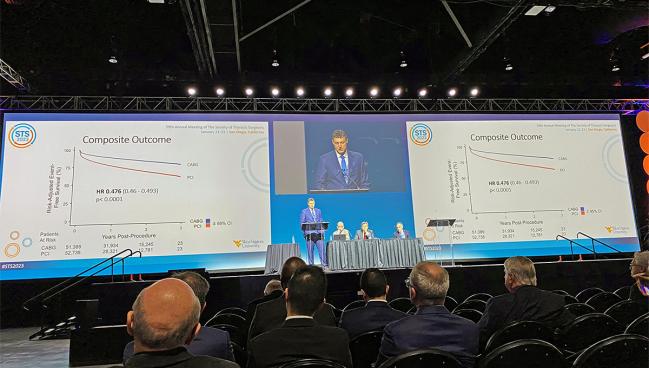
The findings will no doubt add fuel to an ongoing debate over the 2021 revascularization guidelines from the American Heart Association, American College of Cardiology, and Society for Cardiovascular Angiography and Interventions, a document that downgraded surgery to a 2b recommendation for patients with stable multivessel disease. As such, the new analysis should have “policy and practice implications,” said J. Hunter Mehaffey, MD (West Virginia University, Morgantown), who presented the J. Maxwell Chamberlain Memorial Paper in Adult Cardiac Surgery on Saturday during the Society of Thoracic Surgeons (STS) annual meeting.
Cardiothoracic surgeons were “shocked” when the guidelines downgraded CABG to a class 2b from a class 1 recommendation for patients with stable three-vessel coronary artery disease, Mehaffey said, a move that led the STS as well as the American Association for Thoracic Surgery to not endorse them. Subsequent news coverage of the guidelines has caused confusion for patients and referring physicians alike, Mehaffey argued.
“We have to focus on the data,” he told TCTMD. “The majority of providers are not reading the fine print. They are not focused on the details and the nuances of the guidelines, and when we provide a confusing message to patients, . . . I think it's detrimental to the overall healthcare of patients. I think that it's our responsibility as physicians to ensure that patients are getting the best therapy for their disease.”
Discussing the study following Mehaffey’s presentation, Joseph Sabik, III, MD (University Hospitals Cleveland Medical Center, OH), highlighted the fact that it was focused on ACS patients, whereas the downgrade in the guideline was specific to stable CAD patients with multivessel disease. As such, Sabik asked, would these data be “beneficial in assisting in a reevaluation of the 2021 revascularization guidelines.”
In response, Mehaffey predicted that “literalization of the definition of ‘stable’ may result in further guideline creep” and said for this reason the study “is an important contribution . . . to take back the narrative about bypass surgery to ensure patients are getting the optimal treatment.”
Audience member Faisal Bakaeen, MD (Cleveland Clinic, OH), appeared to agree, calling the results both important and timely. This study of real-world data “really builds on what we already know,” Bakaeen said, citing not only older trials like SYNTAX but the newer FAME 3. “The data is clearly on our side.”
But David Cohen, MD (St. Francis Hospital, Roslyn, NY), commenting on the findings for TCTMD, countered that Medicare claims data are an inherently flawed way to compare CABG and PCI. “The selection that goes into these two treatments is enormous. There are anatomic features that would favor one over another, but most importantly there are clinical features,” he said. “We know that a frail patient, a patient with very severe components of different comorbidities, is simply not going to get surgery.”
Even with the risk adjustment that the researchers performed, he said, “it is virtually impossible with the granularity of claims data to do a good job of risk adjusting it.”
This is confirmed by their results, Cohen argued. Because the survival curves separate very early in favor of surgery, “that tells you that there are unmeasured factors that are driving these differences. It's not the procedures.”
Wilson Szeto, MD (University of Pennsylvania, Philadelphia), who co-moderated the STS session, told TCTMD he would like to see physicians more consistently discuss surgery as an option for patients with multivessel disease but acknowledged that knowledge gaps remain. “The narrative and the story will continue,” he predicted. “This data shows that there's still a lot for us to learn and that coronary artery bypass grafting is still a very effective, durable treatment for patients in a longitudinal fashion.”
Better Longitudinal Outcomes With CABG
For the study, Mehaffey and colleagues included all Medicare beneficiaries with ACS undergoing isolated CABG (n = 51,389) or PCI (n = 52,738) for multivessel disease between 2018 and 2020. CABG patients tended to be younger and have more comorbidities.
After adjustment, PCI was associated with significantly lower risks of stroke, renal failure, acute kidney injury, and blood transfusion but a higher risk of death compared with CABG during the index hospitalization. At 30 days, however, all of these endpoints favored CABG.
For the primary outcome of risk-adjusted survival over 3 years, CABG came out ahead of PCI with an almost 60% reduction (adjusted HR 0.45; 95% CI 0.44-0.46). The same was seen with the composite primary outcome of death, repeat revascularization, and readmission for MI (HR 0.48; 95% CI 0.46-0.49).
When the researchers looked at 3-year risk adjusted longitudinal outcomes, CABG was favored over PCI for the composite endpoint as well as for death, all-cause readmission, coronary reintervention, and cost-specific readmission for MI, bleeding, and heart failure. There was no advantage seen for either intervention in terms of reducing readmissions for stroke.
Outcomes were similar in subgroup analyses looking at patients 75 years and younger, older than 75 years, and those with diabetes, heart failure, or NSTEMI.
“These contemporary, real-world data highlight the clear benefits of CABG over PCI in multivessel coronary artery disease,” Mehaffey concluded.
“Across the board, no patient is excited to have open heart surgery, and everyone is looking for an excuse to be able to avoid open heart surgery,” he told TCTMD. “Really it's our job to interpret the data and educate the patients, because the decisions they're making about the treatment they receive now not only affects their quality of life and their outcomes in 30 days and 6 months, but whether or not they're alive or dead at 3 years, 5 years, and 20 years.”
‘Take Back the Narrative’
Sabik noted that while the researchers have “demonstrated the superiority of coronary surgery over percutaneous coronary intervention in hospitalized Medicare patients with acute coronary syndrome, . . . it is fair to note the benefits of coronary surgery came at the cost of more hospital morbidity, greater length of stay, and higher hospital costs.”
Cohen had other concerns, pointing out that previous randomized trials have shown, at most, a 20% relative increase in mortality with PCI over CABG, whereas this study suggests a 100% relative increase. “The effect here is so much larger than what has been observed in well-done randomized trials that we know that there is an enormous amount of what we call unmeasured confounding that is driving these patient differences, not treatment differences,” he commented.
Because of all of these issues, Cohen concluded that “this study is hugely problematic. . . . Therefore, I don't think this adds anything meaningful to our understanding of the differences between the two procedures. It simply is a confirmation that the patients are different.”
Sabik pointed out that guideline writers typically only include randomized trial evidence to support their recommendations. “Observational studies such as yours are often ignored or given very little weight,” he said to Mehaffey, asking why this study should be treated differently.
Mehaffey pointed to the limitations of clinical trials, including “smaller sample sizes, selection and exclusion criteria which limit generalizability, treatment crossover, and longer duration to wait for the results.” He argued that his study is worthy of being considered by those developing clinical guidelines, as it “serves an example of how high-fidelity longitudinal databases provide real-world contemporary data on over 100,000 patients and can guide clinical decisions as well as policy-making.”
Cohen disagreed. “Using flawed studies to support something that you believe inherently is not the right way to convince patients of it,” he said. “It just is misleading.”
STS Past President W. Randolph Chitwood Jr, MD (East Carolina Heart Institute, Greenville, NC), closed out the session by saying that his own CABG surgery, performed using bilateral mammary arteries 30 years ago, is still going strong with “good ventricular function, no infarct, no angina, no stents. [I’ve been] cathed twice, perfect mammaries. I think that says it all.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Mehaffey JH. Contemporary coronary artery bypass grafting versus multivessel percutaneous coronary intervention in 100,000 matched Medicare beneficiaries. Presented at: STS 2023. January 22, 2023. San Diego, CA.
Disclosures
- Mehaffey and Bakaeen report no relevant conflicts of interest.
- Sabik reports serving on the advisory board and as a speaker for Medtronic.
- Szeto reports conflicts of interest with Medtronic, Aqudeon, Artivion, Edwards Life Science, Microinterventional Device, and Terumo Aortic.
- Cohen reports being employed by the Cardiovascular Research Foundation and receiving research grants and consulting support from Abbott, Boston Scientific, and Medtronic.




Comments