No Long-term CV Impact With Mild COVID-19, Two New Studies Reassure
A study of UK healthcare workers and another in college athletes reject the role of CV imaging after mild or asymptomatic disease.

Mild cases of COVID-19 that do not require hospitalization are unlikely to have any lasting cardiovascular effect on otherwise healthy individuals, a study of British healthcare workers suggests. Published the same week, the latest in a series of analyses looking at college athletes who recovered from mild COVID also found no evidence of cardiac damage on imaging.

At 6 months, mild infections “left no measurable cardiovascular impact on LV structure, function, scar burden, aortic stiffness, or serum biomarkers,” write the UK researchers, led by George Joy, MBBS (Barts Heart Centre, London, England). The study, which compared healthcare professionals who did not test positive for COVID-19 (75 subjects) with those who did (74 subjects), was presented last weekend at the EuroCMR meeting and simultaneously published in JACC: Cardiovascular Imaging.
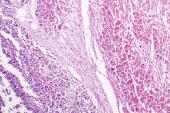
Questions about screening for cardiac abnormalities after COVID-19 have been raised by several studies, including one in mostly younger, nonhospitalized patients, which caused concern last year by showing that 78% had abnormal CMR findings. Similarly, studies in college athletes who had COVID-19 suggested the potential for subclinical myocarditis and damage or other forms of myocardial and pericardial injury. However, a larger study of professional athletes found an incidence of myocarditis of just 0.6%, while another study of over 3,000 college athletes found a 0.5% to 3.0% prevalence of definite, probable, or possible SARS-CoV-2 cardiac involvement and a low risk of adverse cardiac events over short-term follow-up.
In an accompanying editorial, Colin Berry, PhD, and Kenneth Mangion, PhD (University of Glasgow, Scotland), say the findings from Joy et al provide “welcome, reassuring information” that persistent evidence of cardiovascular complications is uncommon in healthy individuals who have had mild COVID-19 infection. They agree with Joy and colleagues that the findings “do not support cardiovascular screening in individuals with mild or asymptomatic infection with COVID-19.”
Contacted by TCTMD, Valentina Puntmann, MD, PhD (University Hospital Frankfurt, Germany), who authored the CMR study showing a 78% rate of abnormal findings, emphasized that the British healthcare workers were part of a small and highly selected group.
“[The study] does not cover the many patients with long COVID syndrome, whether mild or severe—many of whom are [National Health Service] workers—who suffer from fatigue, shortness of breath and palpitations and other frequently unspecific cardiac symptoms,” she said in an email. “It might risk misinterpretation that the symptoms may be dismissible. Also, a study in 75 selected patients provides an indication that needs to be reproduced by lived experience and, obviously, confirmed by long-term data.”
At a mean age of 37 years, the healthcare workers also are significantly younger than the typical at-risk community-dwelling population, Berry and Mangion point out, which also limits generalizability of the findings.
Similarly Low Rates of CV Abnormalities
Joy and colleagues recruited the 149 healthcare workers from the larger COVIDsortium project, an ongoing prospective study of over 700 healthcare workers from three London hospitals. The 74 seropositive individuals had mild symptoms that included fever, dry cough, loss of smell, and loss or distortion of taste. More than half of those who tested positive were asymptomatic.
A study in 75 selected patients provides an indication that needs to be reproduced by lived experience and, obviously, confirmed by long-term data. Valentina Puntmann
Participants had weekly documentation of symptoms, polymerase chain reaction testing, and serology assessment over 4 months. At 6 months they underwent cardiovascular phenotyping, which included cardiac MRI and biomarker testing. At that time, 11% of the total cohort had some symptoms: sore throat (3%); fatigue (3%); runny nose (3%); shortness of breath (2%); and productive cough, chills, diarrhea, or loss of smell or taste (1%), with no difference between seropositive and seronegative individuals.
There were no statistically significant differences between the infected and noninfected healthcare workers for any of the prespecified primary endpoints: LVEF, indexed end-diastolic volume, late gadolinium enhancement, septal T1, and septal T2. Neither were there any differences between group for any of the prespecified secondary endpoints: LV mass indexed, left atrial area indexed, global longitudinal shortening, septal extracellular volume fraction mapping, and aortic distensibility.
Mild abnormalities that were found across both groups included aortic root dilatation, left atrial dilatation, reduced LV function, and T1 and T2 elevation. Myocarditis-like scar was present in 4% of patients in both the COVID-19 seropositive and seronegative groups, with none having evidence of pericardial thickening.
Unanswered Questions Remain
Puntmann noted that while the study does introduce a number of innovative methodological concepts, “the clinical value of many of them still needs to be determined.” She also pointed out that on average the participants had normal or supernormal results, which differs from previous studies, even those in athletes.
Joy and colleagues further note that the study “does not prove that apparently mild SARS-CoV-2 never causes chronic myocarditis,” adding that “the study design would not distinguish between individuals who had sustained completely healed myocarditis and pericarditis and those in whom the heart had never been affected.”
But the study does add to a growing body of information that is, on the whole, more reassuring than the reports of last year. Also out this week, a study published as a research letter in Circulation showed that among 137 college athletes who had mostly mild COVID-19 infections, just five cardiac abnormalities were detected on initial imaging tests; all were ruled out as abnormal on CMR.
“No athlete experienced new symptoms or problems after return to training and competition. On the basis of the outcomes and follow-up in our cohort, it is reasonable to defer cardiovascular screening in asymptomatic athletes or those with milder COVID-19 as outlined in current recommendations,” write Benjamin S. Hendrickson, MD (Le Bonheur Children’s Hospital, Heart Institute, Memphis, TN), and colleagues.
Still, a number of gaps remain in understanding the prevalence of cardiovascular and multisystem involvement in recovered patients, say Berry and Mangion in their editorial. Ongoing studies such as CISCO-19 and UK COVID HEART are expected to yield more information, they add, noting that it also would be useful to target patients who had COVID-19 and who have had prior cardiac imaging that could be used for comparison.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Joy G, Artico J, Kurdi H, et al. Prospective case-control study of cardiovascular abnormalities 6 months following mild COVID-19 in healthcare workers. J Am Coll Cardiol Img. 2021;Epub ahead of print.
Berry C, Mangion K. Cardiovascular complications are very uncommon in healthcare workers with mild or asymptomatic COVID-19 infection. J Am Coll Cardiol Img. 2021;Epub ahead of print.
Hendrickson BS, Stephens RE, Chang JV, et al. Cardiovascular evaluation after COVID-19 in 137 collegiate athletes: results of an algorithm-guided screening. Circulation. 2021;143:1926-1928.
Disclosures
- The COVIDsortium was funded by donations from individuals, charitable trusts, and corporations including Goldman Sachs, Citadel and Citadel Securities, The Guy Foundation, GW Pharmaceuticals, Kusuma Trust, and Jagclif Charitable Trust, and enabled by Barts Charity with support from UCLH Charity.
- Joy, Mangion, Puntmann, and Hendrickson report no relevant conflicts of interest.
- Berry reports that his institution holds research and consultancy agreements with Abbott Vascular, AstraZeneca, Coroventis, GSK, HeartFlow, Menarini, Neovasc, Novartis, and Siemens.




Comments