OCT-Based Strategy Outperforms Angiography in Calcified Lesions: CALIPSO
The results are intuitive, but whether better stent expansion will translate into better clinical outcomes is still up for grabs.
PARIS, France—Patients with calcified lesions undergoing PCI can benefit from an OCT-based strategy for lesion preparation and stent optimization, achieving greater minimum stent area (MSA) than with angiography alone, data from the CALIPSO trial demonstrate.
“We know that coronary calcifications are very frequent among atherosclerotic stenoses and are associated with poor clinical outcome, even in the short term with increased risk of stent thrombosis and in the long term with increased need for target-lesion revascularization,” said Nicolas Amabile, MD, PhD (Institut Cardiovasculaire Paris Sud, France), who presented the late-breaking clinical trial findings this morning at EuroPCR.
Various strategies that leverage intravascular imaging—either OCT or IVUS—to guide management of these lesions have been proposed, he told EuroPCR attendees. “However, the data supporting this approach are currently scarce, and none of these algorithms [have been] validated in practice so far.”
CALIPSO, said Amabile, is the first randomized controlled trial to pit an OCT-based strategy against conventional angiography in this space.
Davide Capodanno, MD, PhD (University of Catania, Italy), commenting on the results for TCTMD, said CALIPSO fits into the larger story of intravascular imaging in PCI. The hotly anticipated ILUMIEN IV, which disappointed cardiologists by showing target-lesion failure was no less frequent by 2 years with OCT versus angiography, also contained a substantial portion of patients—11.5%—with severe coronary artery calcification, for instance.
But, as reported by TCTMD, enthusiasm remains for intravascular imaging—especially in high-risk cases—despite what have thus far been encouraging but still-murky data.
With CALIPSO, Capodanno said, it’s good “to see something randomized in a particular underserved population. [Calcified lesions] are where you would expect OCT to work well.” That said, OCT is capable of detecting superficial calcium, not so much the extent of periadventitial calcium, “so it’s interesting to see if it’s at an advantage or not,” he added.
MSA is a surrogate endpoint, but based on the evidence, it seems that even small differences can have an impact, he noted. “We know that the larger the stent in the end, the better the outcomes will be.” Even apart from clinical outcomes, said Capodanno, the knowledge that a stent has been well expanded thanks to OCT guidance can be reassuring in cases where patients are on a shorter duration of dual antiplatelet therapy.
Larger Minimum Stent Area, Done Safely
Amabile and colleagues analyzed data on 134 patients with stable moderate-to-severe calcified coronary lesions who were randomized to undergo PCI under OCT (n = 65) or angiographic guidance (n = 69). Baseline characteristics were similar.
In the OCT arm, operators used a predefined algorithm for lesion preparation then based stent sizing on OCT analysis, followed by mandatory stent postdilatation, then a post-PCI OCT run, and optimization if required. “Management was mainly based on the maximal extent of calcified plaque,” such that under a threshold of 180° patients were eligible for noncompliant-balloon predilatation, Amabile explained. Between 180° and 270°, noncompliant-balloon predilatation or intravascular lithotripsy (IVL) could be used. Above that, rotational atherectomy or IVL were suggested.
In the angiography arm, all aspects of treatment, including plaque modification, were at the operator’s discretion, but again stent postdilatation was mandatory.
Upfront lesion preparation consisted of noncompliant balloon in 63% of the angiography arm versus 39% of the OCT arm, whereas rotational atherectomy was used in 25% versus 17% and IVL in 12% versus 46%, respectively.
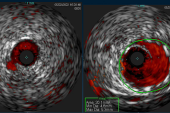
After PCI, all patients underwent a final OCT run in order to assess MSA, the primary endpoint. The median MSA was 6.5 mm2 with OCT versus 5.0 mm2 with angiography (P < 0.001), with mean MSA values of 6.9 mm2 and 5.3 mm2, respectively. Below the threshold of 4.5 mm2, stents were considered underexpanded, said Amabile. Very few of the OCT-guided cases fell under that cutoff.
“Whether this superiority in terms of imaging endpoints will translate into clinical benefit should be assessed in the future,” Amabile concluded.
Beyond this, the researchers found shorter major malapposition length in the OCT group. There were no differences in the number of stents, stent length, or maximal stent diameter.
The OCT-based strategy also appeared safe, with no difference in periprocedural complications, total X-ray dose, volume of contrast medium, or procedure duration compared with angiography. There was no difference in the periprocedural MI rate, and no additional MACE occurred in the month after PCI.
Whether this superiority in terms of imaging endpoints will translate into clinical benefit should be assessed in the future. Nicolas Amabile
Ziad Ali, MD, DPhil (St. Francis Heart Center, Roslyn, NY), the discussant for CALIPSO, pointed out that the difference in MSA is the largest he’s seen in any trial of OCT or IVUS. By comparison, the difference in ILUMIEN IV, for which he served as a principal investigator, was 0.4 mm2, he said. “This is probably the area where we could look to potentially impact clinical outcomes. . . . Do you think that is the mechanism by which we could [derive] long-term clinical benefits?”
“I hope so,” Amabile replied, adding that they are currently pursuing 1-year follow-up.
In his comments, Ali questioned whether the benefits already shown in the new trial resulted from steps taken to address calcification or from the imaging itself. “Because what we’re seeing here,” he said, “is very similar to what we see in the overall population of ILUMIEN—is the finding that the OCT allows you to size the vessel better and therefore place larger stents from the outset, or is this a calcium-specific effect?”
“It looks like there is a calcium-specific effect,” said Amabile, “especially because when we went over the data, we realized that probably the difference in terms of preparation was related to better calcium-burden evaluation by the operators in the OCT group compared to the angio.” In fact, he said, the immediate MSA after stenting in the OCT group, prior to any optimization and differences only resulting from lesion preparation, was still higher compared to what was seen with angiographic guidance.
Also interesting, Ali pointed out, is that the modes of lesion preparation differed less in severe calcification. “What that tells us is the operators are very good at being able to see 360°, or concentric calcium. We’re also very good at being able to see moderate calcification, because it’s only on one side. What we can’t see by our eye on angio is 180-270°, so that’s where we saw the biggest difference in the use of the different devices. Maybe it’s that area we need to focus on.”
Amabile agreed, noting that additional analyses of the initial angiograms showed a larger magnitude of effect in moderate compared with severe calcification.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Amabile N. OCT vs. angiography for guidance of calcified lesions PCI: the CALIPSO (Calcified Lesion Intervention Planning Steered by OCT) trial. Presented at: EuroPCR 2024. May 16, 2024. Paris, France.
Disclosures
- Amabile reports receipt of grants/research support from Abbott and receipt of honoraria or consultation fees from Abbott, B. Braun Melsungen AG, Boston Scientific, and Shockwave Medical.




Comments