OPTIMIZE: 2-Year DES Data Affirm Need for Meaningful MI Definitions
Meaningful rather than “chemical” MI definitions should be an “urgent clinical priority,” one investigator says.

Two-year results for an ultra-low-profile, fixed-wire, sirolimus-eluting coronary stent show no signs of the high target-vessel MI rates that resulted in the OPTIMIZE trial’s failure to demonstrate noninferiority for the novel stent against a standard DES at 1 year. More importantly, the results dramatically highlight the importance of standardized, clinically relevant study definitions among trialists, according to OPTIMIZE investigators.
“We need a definition of myocardial infarction that is associated with subsequent adverse outcomes, because chemical MIs that are diagnosed by a troponin elevation clearly are not associated with an increased risk of adverse events when measured in the periprocedural setting,” said Sunil Rao, MD (Duke Clinical Research Institute, Durham, NC), when presenting the 2-year results of OPTIMIZE in a “Key Abstract” session online last week as part of a sneak peek at TCT 2021. “The OPTIMIZE trial was the canary in the coal mine that called attention to this point, and I think it's a really urgent clinical priority for those of us who do clinical research.”
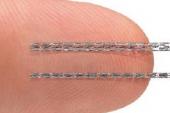
OPTIMIZE pitted the Svelte DES and Slender integrated delivery system (Svelte Medical Systems), which is designed to make direct stenting more feasible, against contemporary everolimus-eluting stents (Xience; Abbott/Promus; Boston Scientific) in 1,639 patients. At 1 year, the novel DES failed to meet a prespecified noninferiority composite endpoint of target lesion failure.
Target-vessel MIs—90% of them periprocedural—were found to be the main driver of TLF, with patients who were assessed solely with high-sensitivity troponin accounting for 80% of all target-vessel MIs. When the results were presented at TCT 2020, the OPTIMIZE investigators suggested that if they had used either the Society for Cardiovascular Angiography and Interventions (SCAI) criteria or Universal Definition of target-vessel MI, it likely would have removed the “noise” caused by minor troponin elevations and the noninferiority endpoint would have been met.
As Rao showed in his new presentation, the 2-year results found no significant difference between stent groups in rates of target-vessel MI using the following criteria: biomarker elevation within 48 hours of PCI with CK-MB or troponin > 3 times upper reference limit (URL) or total CK ≥ 2 times the URL; new pathological Q waves; or autopsy evidence of acute MI.
Under those criteria, the rates of 1-year target-vessel MI were 8.22% with the control DES and 9.43% with the ultra-low-profile DES (P = 0.42), while the 2-year rates were 8.81% and 10.23%, respectively (P = 0.48).
Elephants and Workhorses
Moderator Ziad Ali, MD (St. Francis Hospital & Heart Center, Roslyn, NY), struggled with the “elephant in the room” that periprocedural MI presents to clinical trialists.
“If we remove periprocedural MI, our event rates are going to drop so low that it's going to be statistically even more difficult to show a difference,” he said. “If we do include them, we run into a problem like this where the device actually worked—it had the lowest target lesion revascularization of any . . . drug-eluting stent, but it missed its primary endpoint.”
Rao responded that “just because high-sensitivity troponin is important for spontaneous MI, it may not necessarily be applicable to device trials or stent trials where we're trying to look for periprocedural MIs that are, in fact, associated with adverse clinical outcomes.”
Compared with controls, the ultrathin DES also showed no differences in rates of clinically indicated target lesion revascularization, cardiac death, or TLF at 2 years, and the findings were confirmed in Kaplan-Meier analyses, Rao noted.
Definitions aside, discussant Michael Haude, MD, PhD (Rheinland Klinikum Neuss, Germany), said he remains uncertain how often direct stenting, one of the primary purposes of the new stent, is possible in routine practice. Furthermore, Haude said a fixed-wire stent needs to be as steerable as the gold-standard DES if it is going to become “our workhorse standard in the cath lab.”
Rao responded that the stent is “incredibly deliverable,” even through a 6-Fr diagnostic catheter if necessary. “I think there are a couple of settings where this stent may be very advantageous,” he added. “Obviously, if you need to work very quickly in a STEMI setting, for example, where lesions are relatively soft, you can get away with direct stenting.”
However, Rao said Haude’s point about steerability is a good one.
“You do give up your guidewire position, because once you deliver the stent you withdraw the entire system, and if you need to dilate you may have to go back down a separate wire. Whether it has a role in more complex lesions, I think remains to be seen as we get more experience with this in clinical practice,” he acknowledged.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Rao SV. Two-year results of the OPTIMIZE IDE trial: A randomized evaluation of sirolimus-eluting coronary stents with fixed-wire and rapid-exchange delivery systems and a novel bioresorbable drug carrier. Presented at: TCT 2021. October 20, 2021.
Disclosures
- OPTIMIZE was funded by Svelte Medical.
- Rao reports no relevant conflicts of interest.



Comments