PA Pressure Monitoring Useful Even in Presymptomatic CHF Patients
In GUIDE-HF patients with elevated biomarkers, but no recent hospitalizations, hemodynamic monitoring still signaled events.
Wireless pulmonary artery pressure monitoring with CardioMEMS (Abbott) may be an option in chronic heart failure (HF) patients who have elevated natriuretic peptides and presymptomatic congestion but have not had a recent hospitalization, according to an analysis of the GUIDE-HF study.
The implantable censor is approved by the US Food and Drug Administration as a preventive strategy for patients with class III HF to reduce future hospitalization risk in those who have had a hospital stay for HF within the prior year. Since slightly less than half of all patients in the GUIDE-HF trial were enrolled on the basis of elevated natriuretic peptides alone, the investigators compared their outcomes, by treatment assignment, with patients in the trial with a recent hospitalization.
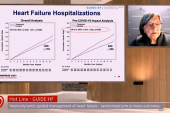
For the primary endpoint (all-cause mortality, HF hospitalization, or urgent HF visits), hemodynamic-guided management resulted in an 8% decrease in the group with prior hospitalization and a 14% decrease in the elevated natriuretic peptides group, reported Akshay S. Desai, MD (Brigham and Women’s Hospital, Boston, MA), in a late-breaking presentation at the inaugural Technology and Heart Failure Therapeutics (THT) 2022 meeting in New York. For the endpoint of HF hospitalization alone, there was a 16% decline in the prior hospitalization group and a 12% decline in the elevated natriuretic peptides group.
“Our conclusions from this analysis are that despite lower event rates in those with elevated natriuretic peptides but no recent heart failure hospitalizations, the effects of hemodynamic-guided heart failure management were similar across enrollment strata,” said Desai.
The main GUIDE-HF trial, presented and published in 2021, examined 12-month outcomes in two types of stable outpatients: those with mild or severe HF symptoms (NYHA class II or IV) and those with elevated natriuretic peptides without a recent HF hospitalization. All patients were implanted with the sensor and then randomized to pulmonary artery pressure monitoring or usual care with no access to the sensor data. No statistically significant differences were seen in the primary endpoint between those managed hemodynamically or with usual care. However, as the authors noted at the time, the study was impacted by the COVID-19 pandemic, resulting in a marked reduction in hospitalizations for HF. Recently, the GUIDE-HF investigators presented a subgroup analysis of clinical events that occurred before March 2020, which showed a statistical advantage in hemodynamically managed patients, regardless of ejection fraction status, driven by fewer HF hospitalizations. For this latest analysis focused on presymptomatic patients, Desai and colleagues analyzed outcomes by treatment enrollment for the full study duration, as well as for the pre-COVID period only.
Small Numbers, but Reason for Optimism
Compared with patients with a prior hospitalization (n = 557), those with elevated natriuretic peptides alone and no prior hospitalization (n = 442) were older, more often white, had lower body mass index, were less likely to have diabetes, were more likely to have atrial flutter/fibrillation, and had higher Kansas City Cardiomyopathy Questionnaire (KCQQ) scores and longer 6-minute walk times.
The pre-COVID analysis showed an advantage for hemodynamic-guided HF management in the overall cohort, with a reduction in events compared with usual care (HR 0.81; 95% CI 0.66-1.00). This effect was similar in those with a prior hospitalization and those with elevated natriuretic peptides only, and no treatment by enrollment stratum interaction (P for interaction 0.58). A similar pattern was seen in the full study duration. Here, the reduction in events with hemodynamic-guided care versus usual care missed statistical significance (HR 0.88; 95% CI 0.74-1.05), however, and the number of events in each group was small. In the analysis looking at the impact on HF hospitalizations only, hemodynamic-monitoring trended better than usual care, but was not statistically significant in the elevated natriuretic peptides group in either the pre-COVID or full analysis.
In his presentation, Desai said despite missing statistical significance, the study supports the notion that a hemodynamic-guided approach leads to numerically lower rates of HF hospitalizations in patients with or without a recent hospitalization.
Following the presentation, moderator Gregg Stone, MD (Icahn School of Medicine at Mount Sinai, New York, NY), noted that multivariable analysis could be an important avenue for shedding more light on the differences between the two patient populations.
“I think you have enough events to do that, and you really have to do that, because of differences in age, atrial fibrillation, et cetera,” Stone said. He also noted the importance of stratifying the results further by ejection fraction, which Desai said the GUIDE-HF researchers hope to do. However, he pointed out that “the numbers get very small once you start to look at the subgroups.”
Desai said while he agreed that multivariable analysis would better isolate the effect of hemodynamic-guided monitoring, their aim was simpler.
“I think the ideal concept . . . rather than to prove a clinical benefit in a subpopulation that wasn't prespecified, is largely just to show the consistency of benefit across those strata, even acknowledging the differences in those strata,” he explained.
Despite the small numbers, panelist Anu Lala, MD (Icahn School of Medicine at Mount Sinai), told TCTMD that the trends demonstrated in the pre-COVID and full analysis are meaningful.
“I think the rationale for using the device among those who are congested fits with this analysis,” she said. “It may not necessarily be that you have to have had a recent hospitalization or decompensation, but other markers of congestion may signify those patients who will benefit.”
While caution is needed in interpreting the results so far, Lala said hemodynamic-guided management is one of the first strategies that has been shown to improve outcomes regardless of ejection fraction and as such the potential for broadening its use is important. An additional point is that Lala said she has found that this type of management strategy can be empowering from the patient’s perspective.
“This isn’t just about doing a procedure, it's also about the lifestyle changes that can ensue,” she said. “[Hemodynamic-guided monitoring] can offer opportunities for more education and more communication that benefits our patients.”
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Desai AS. Efficacy of hemodynamic-guided heart failure management in patients enrolled with elevated natriuretic peptide levels but without a recent HF hospitalization: an analysis of the GUIDE-HF trial. Presented at: THT 2022. February 2, 2022.
Disclosures
- Desai reports grants/research support from Abbott, Alnylam, AstraZeneca, Bayer, and Novartis; and consulting fees/honoraria from Abbott, Alnylam, AstraZeneca, Avidity, Biofourmis, Bayer, Boston Scientific, Cytokinetics, DalCor Pharma, GlaxoSmithKline, Lexicon, Lupin, Merck, Novartis, Relypsa, Regeneron, Sun Pharma, and Verily.




Comments