Paclitaxel Safety Concerns Wane as Hope Emerges for Newer PAD Devices
Katsanos says his original meta-analysis is “perhaps” outdated since a mortality signal is not being seen with newer devices.
NEW YORK, NY—Nearly 4 years since the publication of a controversial meta-analysis that set off a firestorm of questions about long-term safety of paclitaxel-coated devices in PAD treatment, the lead author of that paper now agrees with many researchers that safety appears to be less of a concern in real-world use.
But as other experts gathered at VEITH 2022 made clear, this is an ever-changing space with more devices and data yet to come.
The original meta-analysis by Konstantinos Katsanos, MD, PhD (Patras University Hospital, Rion, Greece), and colleagues was published in 2018 and pooled 28 RCTs of DES and drug-coated balloon (DCB) treatment for femoropopliteal artery disease. It showed a signal for all-cause mortality at both 2 years and 5 years in the paclitaxel-treated patients compared with those treated with uncoated devices. It was later found that important follow-up data from some of the RCTs were missing or “inadvertently omitted,” as the endovascular community, regulatory bodies, and industry scrambled to put together the pieces of the paclitaxel puzzle, yet found themselves unable to replicate the signal in real-world evidence.
Here at VEITH 2022, Katsanos presented new data indicating that reconciliation of that missing data from the pivotal trials now puts the risk of all-cause death at 1.3 times higher for claudicant paclitaxel-treated patients at 2 years compared with uncoated devices. That figure is lower than his original estimate of a 1.8 times higher risk. The number-needed-to-harm (NNH), which was 29 at 2 years in the original meta-analysis, is now at 59 in his reanalysis incorporating some of that missing data.
Speaking with TCTMD, Katsanos acknowledged that new evidence seems to have diluted the mortality signal and, more importantly, that 2018 meta-analysis is “perhaps” outdated due to the use of first-generation devices in those trials. That’s part of the reason, he said, that efforts to replicate the mortality signal he documented in real-world data over the last several years were never likely to succeed.
“The problem with reconciling the data between the randomized evidence and the real-world data is the fact that the two are coming from completely different populations,” he said. “Those recently published studies have been using mostly low-dose, new-generation devices. Perhaps the new iterations of paclitaxel-coated balloons are safer and equally effective than the older-generation devices that were mostly the ones driving the signal in the original meta-analysis.”
Much of the real-world safety data has come from the SAFE-PAD study of over 150,000 Medicare patients treated with paclitaxel DES/DCB or BMS/plain old balloon angioplasty (POBA) from 2015 through 2018. At VEITH 2022, the study’s primary investigator, Eric A. Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), presented updated 3.8-year median follow-up data (max 6.9 years) showing that the cumulative incidence of mortality was 67.1% in the paclitaxel group and 68.9% in the control group (HR 0.98; 95% CI 0.97-0.99). Controlling for whether hospitals were high- versus low-volume users of paclitaxel devices did not change the results. Further, use of falsification endpoints (acute MI, congestive HF, and pneumonia) showed minimal association with receiving paclitaxel treatment.
“We have a lot of reassuring data about safety that has occurred outside of the original pivotal trials in [the Katsanos] meta-analysis,” Secemsky told TCTMD. Indeed, SAFE-PAD adds to other long-term safety data from SWEDEPAD and VOYAGER PAD. These along with updated meta-analyses done by VIVA have “quieted” the conversation, Secemsky added, and shifted the emphasis back to the critical importance of the devices for patients with PAD who need revascularization. Four years on, the harm signal, he concluded, is “now crossing the line of null.”
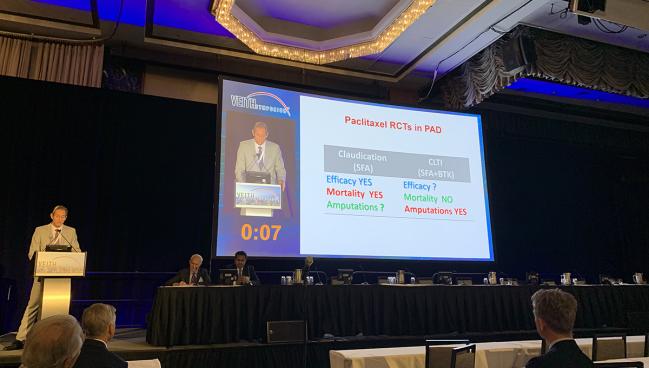
Diminished, maybe, but a mortality signal is undeniably still there, Katsanos argued. “In claudication there seems to be a mortality signal in the low-risk patients. In CLTI [critical limb-threatening ischemia], combining the data for the DCB devices alone, not DES, there seems to be an amputation signal,” he said in his presentation.
But to counter the possibility of a mortality signal in low-risk patients, SAFE-PAD included a prespecified low-risk cohort. As Secemsky showed, data from that group of patients—aged 66 to 70 years with no history of CLTI and fewer than two chronic major comorbidities—overlaps with that of the full cohort for the primary endpoint (HR 0.98; 95% CI 0.87-1.10), showing no difference.
Amputation Signal Still May Warrant Study
The question mark around amputation recalls another Katsanos meta-analysis in 2020 looking at primarily CLTI patients who received infrapopliteal paclitaxel DCBs. That paper found that paclitaxel-treated groups had lower amputation-free survival than those who received uncoated balloon, driven by greater risk of all-cause death and major amputation (HR 1.52; 95% CI 1.12-2.07).
As reported by TCTMD, among the criticisms of the meta-analysis at the time of publication was that it included single-center and unpublished data sets. Here at VEITH, Katsanos showed updated, reconciled data that boost the number of patients from 1,420 to 3,760. Paclitaxel treatment continues to be associated with greater risk of amputation compared with POBA (HR 1.66; 95% CI 1.14-2.42), with the difference driven by substantially greater risk in the CLTI population.
Perhaps the new iterations of paclitaxel-coated balloons are safer and equally effective than the old-generation devices that were mostly the ones driving the signal in the original meta-analysis. Konstantinos Katsanos
Peter A. Schneider, MD (University of California, San Francisco), also presenting at the meeting, said he does not believe there's a mortality signal caused by paclitaxel because it has not been consistent. As for the claim of amputation risk, Schneider said the meta-analysis that supports it left out 19 RCTs in which no amputations occurred and mixed claudicants with CLTI patients.
“It looks like there's a signal, but look at the data. It comes from devices, most of which aren't used [today],” said Schneider. Moreover, ”a lot of them were single-center studies.” In recent years, data from the German BARMER database have shown no support for an amputation signal, and neither have SAFE-PAD or VOYAGER PAD, Schneider noted. Still, he remains cautious.
“Although there is no amputation risk, in my opinion, that's been demonstrated so far, I do think this warrants further study,” Schneider added.
When asked by an audience member about his current practice, Katsanos said: “I'm not using paclitaxel-coated balloons at all in the peripheral vessels.”
Speaking with TCTMD, Katsanos disclosed that in keeping with his presentation’s conclusion about the lack of mortality signal with paclitaxel DES, he does use stents but only one specific device, the Eluvia stent (Boston Scientific). Of note, Eluvia DES were not included in the Katsanos meta-analysis or analyses conducted by VIVA or the FDA, and have long-term safety data from the pivotal IMPERIAL and MAJESTIC RCTs showing no mortality signal.
“I will be perfectly blunt about that,” he explained. “I am still using the Eluvia stent because it is a very low-dose polymer device with well-proven technology for the SFA.” Katsanos said his justification for its use is that the elution of drug is sustained, as opposed to an “acute burst of paclitaxel like in the first iterations of DCB and the Zilver PTX device.”
Katsanos added: “I believe in the potency of the agent. I think that the original versions of those devices were not handling the delivery of the agent the proper way. . . . I think we're going to see a lot more new, improved iterations of paclitaxel technologies in the future.”
Looking Ahead, Maybe to Sirolimus
Some in the endovascular community have already turned their attention toward newer contenders, namely sirolimus, which has proven itself in the coronary arteries and is now being tested in a head-to-head fashion against paclitaxel in the SIRONA trial, with follow-up out to 5 years.
At VEITH, an audience member asked the panel whether, if they had randomized data showing that a limus DCB was noninferior to paclitaxel, they would choose it instead. For Schneider, the question is too theoretical at this point.
“How many years away are we from a sirolimus DCB for above-the-knee, whereas we have multiple tools for above-the-knee with paclitaxel,” he commented. “The SIRONA trial will contribute to that and probably there'll be additional trials in the US. When we have that answer, then then we can alter our practices. But, right now we're looking at a 5-year horizon where it's mainly paclitaxel for SFA.”
In the session, Secemsky said he would not change his practice, elaborating later to TCTMD that it will be important to assess whether, beyond the noninferiority issues, a limus DCB option can give operators pragmatic reasons to switch. That would mean being less expensive and accessible in all healthcare systems and across all PAD patient populations as paclitaxel.
“If we're not confident that there's harm with these paclitaxel devices and there's no benefit to a different drug platform and we have noninferiority, why would I make that choice?” he added.
Katsanos also remains unpersuaded. He agreed that there is a long way to go for the sirolimus device or any other limus DCB to prove itself, not only for efficacy but for long-term safety in the peripheral arteries.
“If sirolimus comes out indeed to be noninferior to paclitaxel in terms of efficacy and is safe, as well, then I think I would probably indeed be moving down to this agent alone,” he said.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Katsanos K. Older and more recent meta-analyses still reveal an increased mortality signal in patients receiving paclitaxel coated devices compared to uncoated devices: the more recent study of DCBs in BTK arteries showed increased mortality and amputation rates after only 1 year. Presented at: VEITH 2022. November 16, 2022. New York, NY.
Secemsky E. An update of the real-world evidence evaluating paclitaxel coated device safety in treating fempop and crural artery lesions: the SAFE-PAD study. Presented at: VEITH 2022. November 16, 2022. New York, NY.
Schneider P. The paclitaxel increased mortality effect reported by Dr. Katsanos et al. seems not to be confirmed by added data: let’s put 4 years of frenetic activity into perspective. Presented at: VEITH 2022. November 16, 2022. New York, NY.
Disclosures
- Katsanos reports clinical research grants from RONTIS and Medalliance.
- Secemsky reports grants to his institution from BD, Boston Scientific, Cook, CSI, Laminate Medical, Medtronic, and Philips; and speaking/consulting fees from Abbott, BD, Bayer, Boston Scientific, Cook, CSI, Inari, Janssen, Medtronic, Shockwave, and Philips.
- Schneider reports consulting for Silk Road, Surmodics, Medtronic, Boston Scientific, Philips, LimFlow, and Cagent.





Comments