POET: Oral Antibiotics Continue to Show Good Long-term Results for Endocarditis
The study found a survival advantage that favored oral treatment, possible due to early discharge and avoidance of hospital-related harms.
NEW ORLEANS, LA—A strategy of switching to oral antibiotics after a short intravenous regimen confers long-term safety and efficacy in endocarditis patients, data from an exploratory analysis of the POET trial show. The updated information provides additional reassurance that the strategy can allow many patients to go home earlier, extending a survival advantage in the form of avoiding hospital-associated illnesses.
Presenting the results here, Henning Bundgaard, MD, DMSc (National University Hospital, Copenhagen, Denmark), said, “Oral antibiotics may safely be administered during approximately half the recommended antibiotic treatment period, and that could potentially be as outpatient treatment.” Oral therapy with early discharge home may be appropriate in more than 50% of patients with endocarditis, he added.
In the main POET trial, patients with left-sided endocarditis who were hospitalized in Denmark and had been receiving IV antibiotics were randomized at 10 days to either continue IV therapy (n = 199) or switch to a regimen of oral antibiotics (n = 201) and discharge to outpatient treatment, if possible.
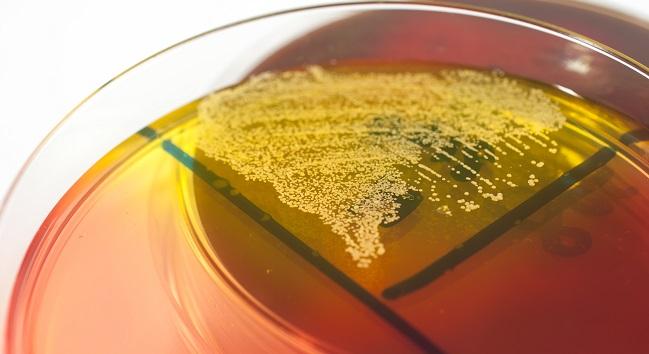
Approximately half of patients in each treatment group had aortic valve endocarditis, about one-third had mitral endocarditis, and about 10% had both mitral and aortic valve endocarditis. The most frequent pathogen involved was streptococci, followed by Staphylococcus aureus, Enterococcus faecalis, and coagulase-negative staphylococci. Most patients had an infection of the aortic valve while about one quarter had developed an infection in a previously implanted prosthetic valve.
At 6 months, all-cause mortality, unplanned cardiac surgery, clinically evident embolic events, or relapse of bacteremia with the primary pathogen (primary endpoint) had occurred in 12.1% of the IV group and in 9.0% of the oral group (OR 0.72; 95% CI 0.37-1.36).
The 3.5-year follow-up presented here at the American College of Cardiology 2019 Scientific Session, shows that the safety and efficacy of the oral strategy is maintained. The primary endpoint occurred in 38.2% of the IV group and 26.4% of the oral group (HR 0.64; 95% CI 0.45-0.91). Among the components of the primary endpoint, there were no significant differences between groups, with the exception of survival—long-term all-cause mortality in the IV group was 27.1% and 16.4% for oral therapy (P = 0.009).
The findings were simultaneously published as correspondence in the New England Journal of Medicine.
Home Sooner and Away From Hospital Hazards
Following his presentation, Bundgaard said he believed the mortality differences likely stem from the oral group being discharged from the hospital about 2 weeks earlier than the IV group.
“We all know that staying in hospital may cause physical as well as mental losses,” he said. “The patients’ capacities are reduced, and these patients are quite often elderly, have significant comorbidities, and are on multiple drugs. So, maybe they don’t ever recover from a functional loss after the prolonged hospital stay.”
This important study does not imply that oral [antibiotics] are applicable to all patients with infective endocarditis. Chris P. Gale
In an email to TCTMD, Chris P. Gale, MD (University of Leeds, England), commented that the long-term results look promising, but also cautioned that “the key here is strict adherence to the inclusion and exclusion criteria of the trial. This important study does not imply that oral [antibiotics] are applicable to all patients with infective endocarditis.”
During the discussion following Bundgaard’s presentation, David Mushatt, MD (Tulane Medical Center, New Orleans, LA), highlighted a number of caveats in extrapolating from the Danish cohort to the US population, including a different subset of infections. While a US population would be expected to have MRSA infections, the Danish population had none, for example. They also had much more strep infections and less staph infections than would be expected in US patients, he said.
Another important issue Mushatt noted was that patients in the oral-medication group were seen two to three times per week for follow-up once they were discharged home, “which would be difficult to pull off in our academic health centers.”
Finally, Mushatt also pointed to the large dose of antibiotics that was required in the oral treatment group: in some patients amoxicillin 1 g had to be taken four times per day. Mushatt observed that side effects such as diarrhea and nausea would be expected. According to Bundgaard, however, there were no side effect issues, prompting Mushatt to jokingly conclude that Danish GI systems might be hardier than those of Americans.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Bundgaard H, Ihlemann N, Gill S, et al. Long-term outcomes of partial oral treatment of endocarditis. N Engl J Med. 2019;Epub ahead of print.
Disclosures
- Bundgaard reports no relevant conflicts of interest.


Comments