Positive Early Data for TAVR in Low-Risk Patients With Bicuspid Valves
Small trials and registries likely offer the best evidence since industry has little appetite to fund an RCT in bicuspid disease.
NATIONAL HARBOR, MD—A small study assessing the feasibility of TAVR in low-risk patients with bicuspid aortic valve stenosis suggests the procedure can be safely performed in these younger patients, with investigators reporting there is no early risk of death or disabling stroke as well as a very low risk of major bleeding or vascular complications.
The results, reported at CRT 2020 earlier this week and published in JACC: Cardiovascular Interventions, come just as new numbers from Society of Thoracic Surgeons/American College of Cardiology TVT Registry were published in Circulation addressing outcomes among patients with bicuspid aortic stenosis treated with current-generation TAVR devices.
“TAVR in bicuspid aortic valves is considered to be a more complex procedure because these valves tend to be more calcified,” lead investigator Ron Waksman, MD (MedStar Heart & Vascular Institute, Washington, DC), told TCTMD. “Also, because there are only two leaflets, it’s harder to dilate them. Retrospective analyses that were done across different cohorts—not necessarily in the low-risk patients—did show that there is a higher pacemaker rate, and more paravalvular leak, in patients with bicuspid valves.”
Presenting the results at CRT 2020, Waksman said the surgical community still strongly believes that patients with bicuspid aortic stenosis should be treated with SAVR and there have been repeated calls for a randomized trial of TAVR versus surgery in this patient group because they were excluded from the low-risk trials. However, since the US Food and Drug Administration expanded the indication of TAVR to low-risk patients regardless of valve morphology in 2019, such a trial would be incredibly difficult, said Waksman.
“We all think it’s going to be very hard to convince patients to be randomized to surgery when TAVR is available clinically and they’re going to shop around,” Toby Rogers, MD, PhD (MedStar Heart & Vascular Institute), one of the study investigators, told TCTMD. “If they go to one hospital and they’re told we’re going to randomize you to a trial, but the hospital down the road will just do the TAVR, that’s very difficult.”
Zero Mortality at 30 Days
The multicenter Low-Risk TAVR trial, which has been previously presented and published, also included 61 patients with bicuspid aortic valve stenosis treated with transfemoral TAVR. Like their trial testing oral anticoagulation in TAVR patients, the Low-Risk TAVR investigators had planned on including up to 100 bicuspid patients in their study, but the expanded FDA indication to low-risk patients dried up enrollment.
The rate of all-cause mortality at 30 days, the study’s primary endpoint, was zero. In a contemporary cohort of 211 low-risk patients with bicuspid aortic valve stenosis who underwent isolated SAVR, the rate of all-cause mortality was 0.5%. In the TAVR-treated patients, there was one nondisabling stroke, one life-threatening/major bleeding event, and two vascular complications. The results were comparable to those seen in the main study of low-risk patients with a TAVR-treated tricuspid aortic valve, although the rate of pacemaker implantation was higher (13.1% in bicuspid vs 6.5% in tricuspid valves).
In addition to the clinical outcomes, there were significant improvements in the mean aortic valve gradient, mean aortic valve area, and NYHA functional class from baseline in the bicuspid patients.
“What we’ve shown here is that despite all the anatomical challenges, with the currently approved devices we can still get good results,” said Waksman.
Jeffrey Popma, MD (Beth Israel Deaconess Medical Center, Boston, MA), who wasn’t involved in the study, said zero mortality at 30 days is a fantastic outcome, but added that discussions with patients with bicuspid aortic valve stenosis in his office revolve around durability, especially since these people present younger than those with classic tricuspid aortic stenosis. There is a need for long-term follow-up, he said.
Waksman said their group plans to follow patients for 5 years. “I’m not sure it’s enough, but that’s the most we could do with this feasibility study,” he said.
Surgeon Michael Reardon, MD (Houston Methodist DeBakey Heart and Vascular Center, TX), one of the panelists who commented on the durability issue, pointed out that patients returning to surgery for valve replacement 8 to 10 years following an initial TAVR have two-to-three times the risk of all-cause mortality than patients undergoing the first surgical procedure. “This is not just a routine surgery in a 10-year-older guy,” said Reardon.
More Data in Sievers type 0 Bicuspid Valves
In Circulation this week, Sharif Halim, MD (Duke Clinical Research Institute, Durham, NC), and colleagues dig into the Society of Thoracic Surgeons/American College of Cardiology TVT Registry to look at procedural and clinical outcomes in 3,705 patients with bicuspid aortic stenosis treated with newer TAVR devices, such as Sapien 3 (Edwards Lifesciences) and CoreValve Evolut R (Medtronic).
Implantation success was slightly lower and postprocedure valve gradients a little higher in patients with bicuspid valves compared with patients with tricuspid aortic valves. There was also more residual moderate or greater aortic insufficiency in the bicuspid group. When the analysis was restricted to Sapien 3 and Evolut R valves, there was an improvement in implantation success and the incidence of aortic insufficiency. Overall, there were no differences in in-hospital or 1-year rates of mortality, stroke, or major bleeding between patients with bicuspid valves and those with tricuspid aortic valves.
During the press conference, while not directly speaking to the new Circulation paper, Waksman highlighted limitations of registry data for addressing at the feasibility of TAVR in bicuspid valves. With the TVT Registry, for example, physicians simply “check a box” for bicuspid valves and there’s little granularity to the data, such as information on bicuspid valve morphology. In fact, Halim et al state the lack of information on the bicuspid subtype is one of their study’s limitations.
Bicuspid valves are heterogenous, said Waksman, and imaging data are needed to properly categorize the valve types. In their analysis, for example, 14% of patients had a purely bicuspid valve with no fused raphes (Sievers type 0), while more than 82% had a Sievers type 1 bicuspid valve (one fused raphe). Just 3.5% had a Sievers type 2 valve (two fused raphes).
Given the different morphologies, Waksman said they need more data in patients with the purely bicuspid aortic valve (Sievers type 0), stating that simply because the procedure can be technically performed doesn’t mean that it should be. However, he would like to see a head-to-head comparison of TAVR versus surgery in patients with similarly classified bicuspid aortic valve subtypes. “We need to compare apples to apples,” he said. “We didn’t have the Sievers classification for the patients who underwent surgery, so we just don’t know what [sort of valve subtype] was on the surgical side.”
Cardiac surgeon Christian Shults, MD (MedStar Heart & Vascular Institute), said registry data will need to be used to tease out how to best manage patients with bicuspid aortic stenosis given that industry also has no appetite for funding a randomized trial. “There are certain subsegments of the bicuspid population who should still have surgery,” he said. “I think we’re going continue to learn about how to effectively manage those groups.”
Rogers noted that a bicuspid valve often goes “hand-in-hand” with a dilated aorta and these patients were not enrolled in the present study. “Those patients should still be going to surgery and having their aortic replaced or repaired at the same time,” he said. “We have to very careful that this data is applied to the right patients and not generalized to every bicuspid patient.”
At the American College of Cardiology 2020 Scientific Session next month, investigators are scheduled to present data from the Medtronic Transcatheter Aortic Valve Replacement (TAVR) Low Risk Bicuspid Study. Waksman said that if their results are corroborated by the Medtronic registry data, “it’s going to be even harder to get people randomized to surgery” in a future study.
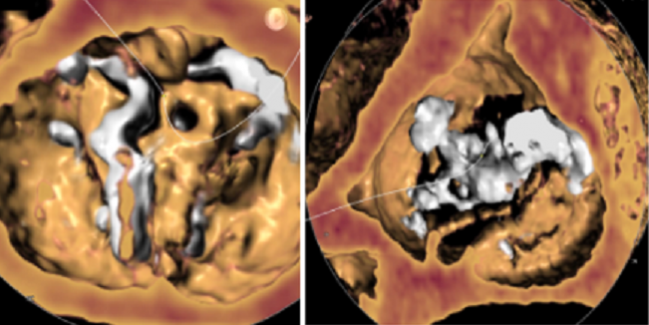
Photo Credit: Mack, M. TAVR for bicuspid aortic stenosis: what is known and what is not. Presented at: TCT 2019. Sept 27, 2019. San Francisco, CA.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Waksman R, Craig PE, Torguson R, et al. Transcatheter aortic valve replacement in low-risk patients with symptomatic severe bicuspid aortic valve stenosis. J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Halim SA, Edwards FH, Dai D, et al. Outcomes of transcatheter aortic valve replacement in patients with bicuspid aortic valve disease: a report from the society of Thoracic Surgeons/American College of Cardiology Transcatheter Valve Therapy Registry. Circulation. 2020;Epub ahead of print.
Disclosures
- Waksman reports consulting for Abbott Vascular, Biosensors International, Biotronik, Boston Scientific, Medtronic Vascular, Symetis, and Lifetech. He reports speaking fees and/or grant support from Abbott Vascular, AstraZeneca, Biosensors International, Biotronik, Boston Scientific, and. Edwards Lifesciences.
- Rogers reports consulting/proctoring for Edwards Lifesciences and Medtronic.
- Reardon reports consulting for Boston Scientific and Medtronic.
- Popma reports consulting for Direct Flow Medical.
- Shults reports no relevant conflicts of interest.


Comments