PRAGUE-17: LAA Occlusion Noninferior to DOACs Over Longer Term
The data provide reassurance that, at least over 3 to 4 years, the intervention compares well against meds, one expert says.
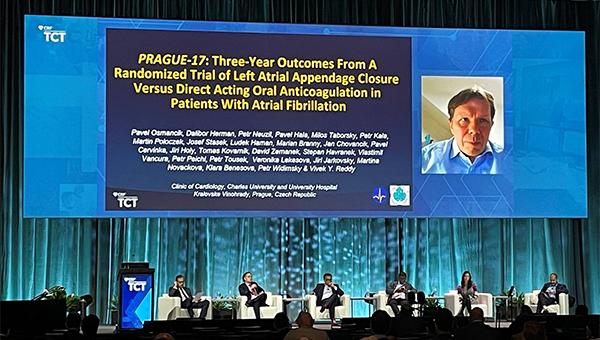
ORLANDO, FL—Left atrial appendage (LAA) closure remained noninferior to direct oral anticoagulants (DOACs) in terms of preventing major cardiovascular and neurological events, as well as clinically relevant bleeding, in patients with atrial fibrillation (AF) over longer-term follow-up in the PRAGUE-17 trial, according to results presented today at TCT 2021.
Over a median of 3.5 years of follow-up, the annualized rate of the primary endpoint—a composite of cardioembolic events, CV death, clinically relevant bleeding, and procedure/device-related complications—was 8.6% in patients who underwent LAA closure and 11.9% in those treated with DOACs, a difference that met criteria for noninferiority (margin of 5%; P = 0.006). That’s consistent with the initial results reported after a median follow-up of 20.8 months.
Most individual outcomes occurred at statistically similar rates in both arms, although the rate of nonprocedural clinically relevant bleeding was lower after LAA occlusion (annualized rate 3.4% vs 5.9%; P = 0.039), Pavel Osmancik, MD, PhD (Charles University Prague and University Hospital Kralovske Vinohrady, Czech Republic), reported.
The findings, which were published simultaneously online in the Journal of the American College of Cardiology, are consistent with the long-term results of the initial trials of LAA occlusion using the Watchman device (Boston Scientific), PROTECT-AF and PREVAIL, and also with subsequent observational studies.
“We believe appendage closure may be considered as a nonpharmacological alternative to long-term anticoagulation in high-risk patients with atrial fibrillation,” Osmancik concluded during a media briefing.
Median Follow-up of 3.5 Years
In PROTECT-AF and PREVAIL, LAA closure with the Watchman was compared with warfarin, but since then, the DOACs have largely displaced vitamin K antagonists as standard of care for stroke prevention in AF, highlighting the need to compare the procedure with the newer anticoagulants.
PRAGUE-17, conducted at 10 cardiac centers in the Czech Republic, was designed to do just that. Investigators randomized 402 patients with AF and high-risk features (mean age 73.3 years; 65.7% men) to LAA closure or DOAC therapy. In the intervention arm, most patients (61.3%) were treated with the Amplatzer Amulet device (Abbott), with the first-generation Watchman used in 35.9% and the next-generation Watchman FLX used in 2.8%. The vast majority of patients in the DOAC arm (95.5%) received apixaban (Eliquis; Bristol Myers Squibb).
In the LAA closure arm, most patients (81.8%) were discharged on dual antiplatelet therapy (DAPT). Another 13.8% received apixaban for 3 months followed by aspirin and 4.4% received apixaban for 6 weeks followed by 6 weeks of DAPT.
This new presentation extended follow-up out to a median of 3.5 years, showing that LAA occlusion remained noninferior to DOAC therapy in terms of the primary composite endpoint. There were no differences between groups for any of the endpoint’s individual components. The per-protocol and on-treatment analyses provided similar results.
Regarding nonprocedural clinically relevant bleeding, the advantage for LAA occlusion became apparent at around 6 months, with the gap widening with longer follow-up. “This again emphasizes that the benefits of LAA closure become more evident as time progresses,” Osmancik et al write in their paper. “The early postimplant period is burdened by both i) procedure/device-related complications which are typically bleeding events (six of nine complications in PRAGUE-17 were bleeding events), and ii) the temporarily more-intense antithrombotic treatment, both of which increase early bleeding.”
Some Questions Unanswered
Commenting for TCTMD, Faisal Merchant, MD (Emory University School of Medicine, Atlanta, GA), who wrote an accompanying editorial in JACC, said PRAGUE-17 provides helpful information in that it compares LAA closure with DOAC therapy rather than warfarin and does so in a population of patients who are not thought to be good candidates for chronic anticoagulation. That’s noteworthy because the initial trials of the Watchman device required patients to be good candidates for anticoagulation. PRAGUE-17 participants are more in line with the population receiving LAA occlusion today, Merchant said.
A noteworthy finding from the long-term results, he said, is that a “sizeable number” of patients in the LAA occlusion arm of the trial ended up taking oral anticoagulation. On the flip side, many patients assigned to DOAC therapy had to stop taking it at some point. Studies like this will always have a lot of crossovers, “which may make it very hard to sort out who really benefits form LAA occlusion and who’s best suited to staying on anticoagulation in the long run.” If a lot of patients have to start anticoagulation after LAA occlusion, he added, “then obviously that really questions the benefit of the procedure. And conversely, for people who we decide to treat with anticoagulation—and a fair number of them end up having bleeding problems and need to have the appendage occluded in the long run—it’d be helpful to have better markers of who’s likely to need to cross over like that.”
In his editorial, Merchant notes that the trial represents a missed opportunity when it comes to providing more information on late cases of device-related thrombus (DRT) or peridevice leak (PDL). Many of the follow-up transesophageal echocardiograms had to be canceled due to the COVID-19 pandemic.
Although there doesn’t seem to be a signal that these issues are resulting in major increases in clinical events, the trial is not definitive in that regard, both because of the relatively small number of patients and the length of follow-up, he said. “I think really teasing apart not only the incidence but also the clinical consequences is going to be important.”
Additional studies are also needed to see whether the separation of nonprocedural bleeding risk continues over longer follow-up, a key question when considering LAA occlusion, which carries up-front risks. “The hope is that over time the nonprocedural bleeding reduction is going to be enough to offset those early events. It certainly seems like things are moving in that direction, so that there’s some hopeful signal there,” Merchant said. He added, however, that the curves could start to converge if a lot of patients undergo the procedure and then require anticoagulation anyway in response to DRT, PDL, or some other issue.
Further trials of LAA occlusion versus DOAC therapy are ongoing, but while awaiting those results, PRAGUE-17 “helps provide some reassurance that as you follow people longer . . . LAA occlusion seems to stand up at least over the course of 3 to 4 years,” Merchant commented. It’s unclear, however, whether the events prevented in PRAGUE-17 are the major events feared by patients—disabling strokes and significant bleeds—or more-minor events.
More analyses will be needed to look into that, “but for right now at least, [PRAGUE-17] provides some reassurance that there’s enough data here to support LAA occlusion and that it makes sense to continue to do these bigger studies while we’re sorting out some of the subtleties of safety and efficacy,” he said.
Merchant said a vexing issue for the field is determining which patients should be treated with LAA occlusion, noting that currently many patients undergoing the procedure are older with a lot of comorbidities, which means they have many competing risks for death. In a patient like that, “it’s very unclear to me at least that doing any one specific thing to reduce their stroke risk is going to have a meaningful impact on their overall survival and quality of life.” He added that a younger, relatively healthy patient who has one specific reason for not being a good candidate for long-term anticoagulation might be better suited for the procedure.
And the choice might not just be between LAA occlusion or anticoagulation in an older patients with a heavy comorbidity burden, Merchant suggested. “I think that there’s a certain point where if you were to take three options—LAA occlusion, anticoagulation, or no therapy—it may be that no therapy starts to be as good as the other two at a certain age and comorbidity profile where doing invasive procedures or specific forms of therapy isn’t beneficial.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Osmancik P, Herman D, Neuzil P, et al. Left atrial appendage closure versus non-warfarin oral anticoagulation in patients with atrial fibrillation. J Am Coll Cardiol. 2021;Epub ahead of print.
Merchant F. Does percutaneous left atrial appendage closure stand the test of time? J Am Coll Cardiol. 2021;Epub ahead of print.
Disclosures
- PRAGUE-17 was funded by a research grant from the Ministry of Health, Czech Republic.
- Osmancik reports occasional speaking honoraria from Bayer and Abbott.
- Merchant reports no relevant conflicts of interest.





Comments