QFR More Consistent Than FFR in Nonculprit Lesions After STEMI
QFR, derived from angiography, might be used to predict which stenoses are likely to matter beyond the acute phase.
PARIS, France—In patients with STEMI and multivessel disease, quantitative flow ratio (QFR) may provide better information than fractional flow reserve (FFR) on how nonculprit lesions will affect physiology after the acute phase.
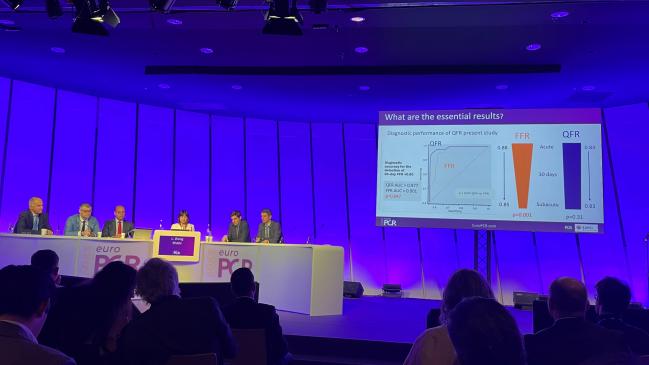
The results, from a post hoc analysis of the REDUCE-MVI study, were released during last week’s EuroPCR 2023 and simultaneously published as a research letter in JACC: Cardiovascular Interventions.
Much attention has been paid over the last decade to the question of how best to manage nonculprit lesions in the STEMI setting, said Lin Wang, MD, (Hospital Clínico San Carlos, Madrid, Spain), who presented the study in a hotline session.
Physiological assessment is appealing as a way to figure out which of these lesions will hold future relevance, she said. Yet “use of FFR to decide revascularization of nonculprit lesions in STEMI patients remains controversial” after studies like the 2021 FLOWER-MI trial, she told EuroPCR attendees.
QFR, an FFR-like index derived from quantitative coronary angiography using computational fluid dynamics, “is a novel approach for functional evaluation of coronary stenosis and has shown good agreement with pressure wire-determined FFR patients in stable coronary artery disease,” Wang noted.
Based on what they saw here, “FFR values in nonculprit lesions vary significantly from acute to subacute STEMI phases,” Wang concluded. “This phenomenon was not observed for QFR.” Their study suggests “QFR might become the physiologic index of choice for clinician decision-making” in STEMI patients with multivessel disease, she added. “The findings also may help in interpreting the results of previous trials and formulating new ones.”
Present and Future
It’s unknown whether QFR measured at the time of primary PCI could, compared with FFR, more reliably predict the functional significance of nonculprit lesions at a later date. But this notion is plausible, since QFR is calculated using models based on stable CAD, Wang and colleagues say.
To explore this possibility, the researchers looked at 70 patients (out of the 110 original REDUCE-MVI participants) for whom QFR could be calculated and FFR invasively measured at baseline and 30 days. All were experiencing their first STEMI and had at least one intermediate nonculprit lesion. Mean age was 61.8 years, and 15.7% were female.
Most often STEMIs were due to an occlusion of the right coronary artery (42.9%), with the nonculprit lesions evenly distributed, at 34.3% each, between the left anterior descending and the left circumflex arteries.
Between baseline and 30 days, QFR values in nonculprit lesions held steady, whereas the FFR values decreased.
Physiologic Assessment of Nonculprit Lesions in STEMI
|
|
Baseline |
30 Days |
P Value |
|
FFR |
0.88 ± 0.08 |
0.85 ± 0.10 |
0.001 |
|
QFR |
0.84 ± 0.09 |
0.83 ± 0.10 |
0.310 |
Baseline QFR values were more tightly correlated than baseline FFR values to the subsequent 30-day FFR measurements. In terms of diagnostic accuracy for the detection of 30-day FFR < 0.80, QFR was more sensitive: it offered an area under the receiver-operating curve (AUC) value of 0.977, while FFR had an AUC of 0.901 (P= 0.047).
Overall, “baseline QFR yielded significantly higher specificity, higher negative and positive predictive values, and higher overall diagnostic accuracy compared with baseline FFR,” the investigators note in their paper.
But Why?
Wang, in a press briefing, told TCTMD that one reason why FFR results are inconsistent is because, in the time between “acute STEMI and subacute STEMI, the hemodynamic conditions have changed.” Another possibility relates to microvascular dysfunction.
EuroPCR Chair William Wijns, MD (Lambe Institute for Translational Medicine and CÚRAM, Galway, Ireland), elaborated by saying that some data show microvascular dysfunction can be present in the nonculprit stenosis in the acute phase.
“And of course the FFR is dependent on the level of increase of flow when you’re giving adenosine or another hyperemic drug,” he continued. If these areas of the microcirculation are full of leukocytes or thrombus, the reaction “to that injection of adenosine might be blunted acutely,” such that the true degree of stenosis is underestimated, Wijns explained. With QFR, flow is calculated from the angiogram rather than measured within the body, “and that’s why maybe it is more stable, more reliable.”
This is yet another strength of QFR, Wijns stressed. The information is already there, available and waiting to be analyzed, within the angiography already being performed. “If you have the right software, you can extract the information, in every patient, in every cath lab, around the world. . . . The only thing you need is two angiograms [of] good quality,” he said.
Physiology Evolves
FFR pioneer Nico Pijls, MD, PhD (Catharina Hospital Eindhoven, the Netherlands), after Wang’s presentation, stepped up to the mic in the auditorium to make the case that it makes sense FFR values wouldn’t be static.
“In normal physiology after acute myocardial infarction, in the first months there is always some recovery of the microvasculature. And that means that if you measure FFR in the acute phase and [again] a month later, it should decrease a little bit because there is some increase of flow. For the same reason [coronary flow reserve] will increase,” said Pijls. The lack of change with QFR represents a “fundamental shortcoming” of the technology, he suggested. “I think that what you prove is the opposite of what you are intending to prove.”
Javier Escaned, MD, PhD (Hospital Clínico San Carlos, Madrid, Spain), senior author for the new study, provided a counterargument. “I think there is a fundamental misunderstanding of the presentation,” he said as he stood beside Pijls in the aisle.
As of now, said Escaned, the “gold standard” for gauging the functional relevance of a nonculprit stenosis is FFR value at 30 days, a concept with which Pijls agreed.
What their data show, Escaned noted, is that QFR at day 0 is better than FFR at day 0 at predicting that 30-day FFR value. “That is the point. So if you make a decision by the time of primary PCI based on FFR, you will be making [more] mistakes compared with if you make decisions based on QFR,” he commented.
Session moderator Davide Capodanno, MD, PhD (University of Catania, Italy), with a smile, predicted: “I guess we will see letters and letters to the editors of JACC: [Cardiovascular] Interventions, with good pleasure.”
Haitham Amin, MBBS (MKCC, Awali, Bahrain), another discussant on the panel, agreed that mechanistically the study’s results make sense. QFR, he said, may be another tool that operators can use—with the angiography already at hand—to assess nonculprit lesions during primary PCI and make an educated guess about what’s to come. If the QFR raises a red flag about potential stenosis at this time, “I think it behooves us to reassess it later on,” said Amin.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Wang L, Travieso A, van der Hoeven N, et al. Improved nonculprit stenosis assessment in patients with ST-segment elevation myocardial infarction using quantitative flow ratio. J Am Coll Cardiol Intv. 2023;Epub ahead of print.
Disclosures
- AstraZeneca supported the investigator-initiated REDUCE-MVI study with an unrestricted grant. The study was also financed by the Netherlands Ministry of Economic Affairs by means of the PPP Allowance made available by the Top Sector Life Sciences & Health to stimulate public-private partnerships.
- Wang reports no relevant conflicts of interest.
- Travieso has received unrestricted research grants from Philips.
- Escaned is on the advisory board and/or has received speaker fees from Abbott, Boston Scientific, Medis Medical Imaging, and Philips, and has reported joint ownership in the angio-IMR patent.




Comments