Residual TR After Treating Mitral ViV Disease Linked to Worse Outcomes
Investigators saw more deaths in patients with severe TR after repeat mitral valve procedures; what to do about it is unclear.

LONDON, England—A new analysis is emphasizing the prognostic significance of residual tricuspid regurgitation (TR) following mitral valve-in-valve procedures, with investigators showing that those with residual severe TR are at a significantly increased risk of death at 3 years.
The results, say investigators, highlight the negative impact of severe TR in patients who are treated for mitral regurgitation (MR) more broadly, and potentially identifies a high-risk group that requires monitoring or early intervention.
Combined mitral and tricuspid disease represents a clinical dilemma in the era of transcatheter devices, lead investigator Kashish Goel, MD (Vanderbilt University Medical Center, Nashville, TN), told TCTMD, noting that while it is the most common combination in multivalvular disease, there is limited data regarding treatment and outcomes in this space. Unlike surgery, where both valves are treated at the same time, transcatheter fixes are not routinely done simultaneously.
“What happens if you completely treat the mitral regurgitation?” said Goel. “Now, [our] data is in patients who have already had mitral valve surgery so they’re already higher risk than the overall population, but I think we can indirectly apply this to patients who undergo transcatheter mitral valve replacement. When you eliminate mitral valve disease, mitral stenosis, or mitral regurgitation, what will happen to the TR?”
Mayra Guerrero, MD (Mayo Clinic, Rochester, MN), who wasn’t involved in the study, said that, in general, if MR is not adequately eliminated in a patient with multivalvular disease, there will be more TR. Put another way, there’s a greater chance of reducing preexisting TR if there is an adequate reduction in MR.
“There are many important points here,” she said, including messages for native valve disease. When deciding between mitral transcatheter edge-to-edge repair (TEER) versus transcatheter mitral valve replacement (TMVR) in patients with both MR and TR, “it’s one more factor to take into consideration—select the procedure that will give you the best reduction in mitral regurgitation,” said Guerrero.
Residual TR After Treating MR
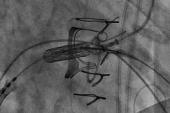
The new study, which was presented this week at PCR London Valves 2024, focused on patients who had undergone transseptal mitral valve-in-valve replacement procedures in the STS/ACC TVT registry between 2015 and 2024. In total, 2,107 had less than mild TR at the time of their mitral valve-in-valve procedure, 1,792 had moderate TR, and 1,039 had severe or greater TR.
In a propensity-matched analysis, the 3-year risk of all-cause mortality in those with severe or greater TR at baseline was 39.4%, which was significantly greater than the 31.3% observed in those with moderate baseline TR and 27.7% in those with mild or less TR (P = 0.005 and P = 0.003, respectively).
It’s one more factor to take into consideration—select the procedure that will give you the best reduction in mitral regurgitation. Mayra Guerrero
Next, investigators assessed TR 30 days after the mitral valve-in-valve procedure. For those with severe TR at baseline, 68.1% had at least a one-grade improvement in TR severity. In a multivariate model, patients with atrial fibrillation/flutter and those with impaired left ventricular ejection fraction (< 35%) at baseline were less likely to have an improvement in TR following the mitral valve procedure.
Investigators then looked at all-cause mortality in propensity-matched patients based on 30-day residual TR. For those with severe or greater TR, all-cause mortality was 43.2% at 3 years compared with 30.7% in those with moderate or less residual TR (HR 0.69; 95% CI 0.48-0.98).
“The worse the TR after fixing their mitral valve, those patients had the highest mortality,” said Goel.
Finally, the group examined the risk of death at 3 years based on improvements or persistence of TR at 30 days post-mitral ViV intervention. Those with severe TR at baseline who had no improvement in the month following the mitral valve-in-valve procedure, as well as those who progressed to severe TR, had the highest risk of death: 46.5% and 38.6%, respectively. Comparatively, those who, early on, improved from severe to mild/moderate TR or who had sustained mild/moderate TR, had the lowest risks of death at 3 years: 26.6% and 23.1%.
What Should be Done With Patients?
While cautioning against extrapolating beyond their data, Goel pointed out that transcatheter studies of patients with severe TR, such as TRISCEND II and TRILUMINATE, have shown that replacing or fixing the valve improves functional status and patient symptoms but does not reduce the risk of death, at least out to 1 year.
“Our study gives us a little bit of insight into TR mortality,” he said, noting that the survival curves for severe TR started to separate from mild/moderate TR after 12 months. “In this very specific group, the risk started increasing after 1 year.” For now, though, the finding should be considered hypothesis-generating only, said Goel.
“This data does not tell us that fixing TR will improve mortality,” he stressed. “This tells us that patients who have continued severe TR will have higher mortality at 3 years. We have no data that a transcatheter fix of TR will help.”
In terms of clinical takeaways, Goel stressed that patients who have residual severe TR should be followed closely. If the patient has atrial fibrillation or low LVEF at baseline, that’s a clue they may not have any improvement in TR after the mitral valve procedure. If symptoms are present, or don’t get better after dealing with MR, the tricuspid valve should then be addressed, he said.
Guerrero said that she’ll see MR patients 30 days after a procedure where she’ll evaluate symptoms and echocardiographic data, but then the next visit is not until 1 year later.
“Does this mean that the 30-day visit is a window of opportunity to detect that one-third of patients [with residual severe TR] who will not get better?” she suggested during the panel discussion.
In response, panelist Azeem Latib, MD (Montefiore Einstein Center for Heart & Vascular Care, Bronx, NY), observed that these patients will often feel better at 30 days because their MR is gone. Like Goel, Latib said that what can’t be answered from these data is whether the residual severe TR should be treated given the evidence of higher mortality at 3 years.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Goel K. Tricuspid regurgitation and 3-year mortality after transcatheter treatment of mitral valve disease. Presented at: PCR London Valves 2024. November 24, 2025. London, England.




Comments