SCAAR Registry Delves Into Left Main Revascularization Outcomes
The observational data raised red flags for many, including the fact that CABG survival curves appeared to separate so quickly.
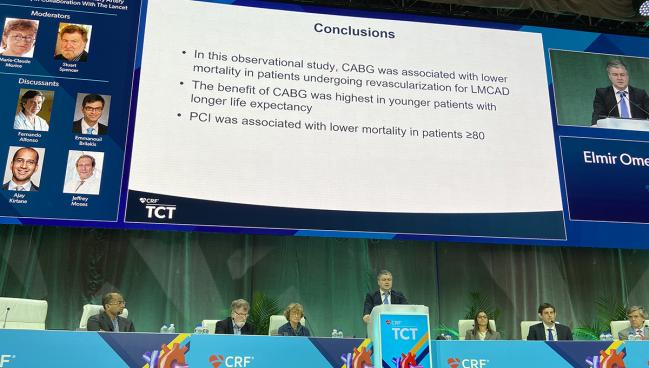
BOSTON, MA—Patients with left main CAD treated with PCI are at a significantly increased risk of death in long-term follow-up compared with patients who underwent CABG surgery, according to new observational data from the Swedish Coronary Angiography and Angioplasty Registry (SCAAR).
The results, which were presented as late-breaking science at TCT 2022, showed that PCI was associated with a 59% increased risk of death compared with surgery after 7 years of follow-up (P = 0.011), reported lead investigator Elmir Omerovic, MD, PhD (Sahlgrenska University Hospital, Gothenburg, Sweden).
Despite the inherent limitations of the observational analysis, Omerovic said, these data reinforce the idea that surgery offers a survival advantage over PCI in a real-world population of patients with left main disease. “I don’t think it’s fair to discount observational studies,” said Omerovic. “Randomized, controlled trials have hazards and limitations, too.”
He also acknowledged these results will add to the current debate over the optimal treatment strategy for left main CAD. “I will just say the ‘EXCEL Controversy,’’ said Omerovic joked. “If you are not laughing, you should probably Google it.”
For Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), these new SCAAR data aren’t particularly contentious, however. “I don’t think anybody should be surprised by the results of an observational analysis like this,” he said during the session.
“The reason I say I don’t think it’s surprising is because if you look at the differences in baseline characteristics of the patients selected for PCI, not randomized to PCI, you can appreciate the difference in the rate of [previous] bypass surgery, the rate of difference in advanced Killip class, and the rate of difference in age. We know these patients are inherently different patients than those selected for surgery. That’s the reason why we do randomized trials. In fact, if you had found PCI was associated with better outcomes, that would have been surprising to me.”
We know these patients are inherently different patients than those selected for surgery. That’s the reason why we do randomized trials. Ajay Kirtane
Cardiac surgeon Richard Whitlock, MD (McMaster University/Population Health Research Institute, Hamilton, Canada), said the increased mortality risk in SCAAR supports the 5-year data from EXCEL showing that CABG surgery was associated with an decreased risk of death when compared with PCI.
He pointed out, however, that while the SCAAR researchers performed statistical analyses, including an instrumental variable analysis, to account for confounding variables, it’s unlikely these were completely eliminated. There are “nuances” in terms of how physicians decide on the appropriate revascularization strategy for patients, and given the early benefit of surgery, some type of procedural or patient-related risk factor isn’t captured by the SCAAR database.
“The mortality benefit emerges pretty early [with CABG surgery]” in this data set, Whitlock told TCTMD. “That’s not typical. It’s really around 5 years out that the curves begin to diverge. These curves diverge early, which tells me there is still some uncaptured or residual confounding.”
Even with those drawbacks, Whitlock said the totality of the data supports a survival benefit with CABG surgery over PCI in left main CAD. In terms of routine clinical practice, Whitlock offered a hypothetical, saying that an 84-year-old with expected survival of 2-3 years is probably best served with PCI, whereas those with a projected survival of 5, 7, or 10 years “really needed to be guided towards CABG assuming they are appropriate candidates.”
Ori Ben-Yehuda, MD (Cardiovascular Research Foundation, New York), who moderated a TCT press conference where the results were presented, also emphasized the immediate separation of the mortality curves, which was surprising because CABG surgery is normally associated with an upfront risk of surgical complications while it takes time for the benefits emerge.
“It does suggest a significant selection bias,” said Ben-Yehuda.
Despite the pushback, Omerovic argued that the instrumental variable analysis can account for known and unknown variables. For example, there was wide variability across the hospitals included in the analysis, with surgery outnumbering PCI by more than two to one at some centers, while PCIs dramatically outnumbered surgeries at others. With their statistical approach, he told TCTMD, they were able to use this variability to their advantage, with the hospital’s treatment preference serving as an act of randomness not unlike randomization in clinical trials. The comparison in SCAAR included patients balanced in all characteristics, said Omerovic.
Wide Variability Across Hospitals
For the uninitiated, EXCEL was a randomized clinical trial comparing PCI with an everolimus-eluting stent (Xience, Abbott Vascular) against CABG surgery for patients with left main CAD. The 3-year results showed that PCI was noninferior to surgery for death, stroke, or MI, but it was the 5-year follow-up that really ignited a firestorm when investigators were accused of not publishing MI data that cast PCI in a less than favorable light and of downplaying the all-cause mortality benefit with CABG surgery. The researchers vehemently denied those accusations.
These new data from SCAAR include all patients with stable angina, unstable angina, or NSTEMI who underwent coronary angiography at 30 PCI-capable hospitals between 2015 and 2022. Of these patients, 10,254 had significant left main CAD, with 52.6% of these undergoing PCI and 47.4% treated with surgery. The surgical patients were younger than those treated with PCI and were less likely to have had a prior MI, PCI, or bypass surgery.
In terms of the findings, Omerovic said real-world data provide value to the research community because they can help shape clinical decisions when physicians engage in discussions with patients.
“For me, 5 or 6 extra months might not be worth it,” he said. “You inform me and respect my autonomy, but I would like to go with PCI because there is less trauma. Yet there are individuals who will value the additional 6 months and that’s what we take away from them if we don’t inform them properly.”
Like Omerovic, Roxana Mehran, MD (Icahn School of Medicine at Mount Sinai, New York), who was an investigator in the EXCEL trial, emphasized that real-world data are incredibly important, pointing out that data from SCAAR have helped the cardiology community understand some of the hazards, including the risks of stent thrombosis, associated with drug-eluting stents. Like others, though, she is concerned the study can’t completely rule out confounding.
Durable Surgical Collaterals
Cardiac surgeon Faisal Bakaeen, MD (Cleveland Clinic, OH), said SCAAR provides very useful reflections regarding the patterns and trends of coronary revascularization practices for left main disease in Sweden. The data also shows tremendous variability in the utilization of CABG versus PCI between different hospitals, with lower-volume centers more likely to perform PCI than higher-volume centers.
But Bakaeen, too, was struck by the survival curves.
“The immediate and early separation of survival curves suggests selection bias,” Bakaeen told TCTMD. “Having said that, modern-day CABG is very safe with perioperative mortality of less than 1% for elective cases. In addition to treating the lesions present at the time of revascularization, CABG provides durable surgical collaterals that provide a prophylactic field protection against future lesions upstream to the bypass. Arterial grafts, especially the left internal thoracic artery to the LAD, are known to maintain perfect patency for decades after surgery.”
Eric Cohen, MD (University of Toronto/Sunnybrook Health Sciences Centre, Canada), an interventional cardiologist, offered another perspective, noting that while statistical modeling can account for multiple variables, it can’t account for the goal of treatment.
“A patient with severe symptoms who might have highly-complex anatomy, including left main [disease], and comorbidities, you’re still more likely to undertake a treatment, and that’s more likely to be PCI rather than surgery, to achieve short-term symptom relief, which is a viable goal patients want and need,” Cohen told TCTMD. “There may be no expectation of extending survival.”
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Omerovic E, on behalf of the SCAAR investigators. Survival after PCI or CABG for left main coronary disease: a report from the Swedish Coronary Angiography and Angioplasty Registry. Presented at: TCT 2022. September 19, 2022. Boston, MA.
Disclosures
- Omerovic reports no conflicts of interest.




Comments