Short DAPT Safe in ACS With No Ischemic Penalty: 4D-ACS
The lower rate of net adverse clinical events was driven by less bleeding in those on 1 month of prasugrel-based DAPT.
PARIS, France—A short duration of dual antiplatelet therapy (DAPT) followed by low-dose prasugrel monotherapy is safe and effective without compromising ischemic protection in ACS patients following drug-eluting stent implantation, results of the 4D-ACS trial show.
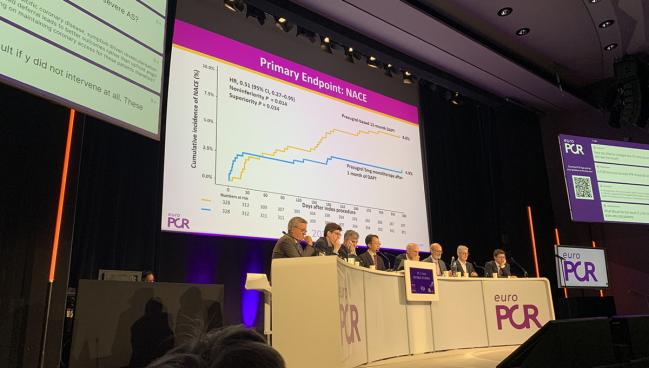
At 12 months, rates of net adverse clinical events (NACE)—a composite of death, MI, stroke, TVR, and Bleeding Academic Research Consortium (BARC) type 2-5 bleeding—were 4.9% in patients on 1 month of DAPT compared with 8.8% in those on 12 months of DAPT, meeting criteria for both noninferiority (P = 0.014) and superiority (P = 0.034).
“In the landmark analysis beyond day 30, the incidence of NACE remained lower in the 1-month group,” said lead investigator Woong Chol Kang, MD, PhD (Gachon University College of Medicine, Incheon, Republic of Korea), in his presentation here last week at EuroPCR 2025. The study was simultaneously published in EuroIntervention.
The short DAPT regimen consisted of 1 month of aspirin plus 10 mg of prasugrel followed by 5 mg of prasugrel alone, while the standard DAPT regimen was 12 months of aspirin plus prasugrel 5 mg.
Despite several studies in recent years looking at how best to handle DAPT in patients with ACS and/or high bleeding risk, no definitive strategy has been embraced. Some investigators have focused on short-term DAPT followed by P2Y12 inhibitor monotherapy (TOPIC and HOST-REDUCE-POLYTECH-ACS), while others have tried dropping aspirin entirely and using P2Y12 inhibitors alone immediately after PCI (STOPDAPT-3). In the latter case, the strategy not only did not reduce major bleeding, but also was accompanied by an increased risk of stent thrombosis compared with aspirin plus prasugrel.
Kang said the difference in NACE between treatment groups in 4D-ACS was driven primarily by a significant decrease in major bleeding in the 1-month DAPT arm: a 77% relative risk reduction in BARC type 2-5 bleeding and an 87% reduction in major bleeding.
Noting some of the other trials that have tested shortened DAPT regimens—featuring a mixed bag of doses and endpoints that included bleeding, MACE, or net clinical benefit—Gilles Montalescot, MD, PhD (Hôpital Pitié-Salpêtrière, Paris, France), said he was not surprised to see that short DAPT followed by prasugrel monotherapy led to less bleeding.
“It’s not new. This is exactly what we found in all the studies,” he said.
But Montalescot drew attention to the fact that gastrointestinal bleeding accounted for over 70% of all bleeding cases, yet proton pump inhibitors (PPIs) were left to the discretion of treating physicians and were prescribed in only 22.5% of those on short DAPT and 25.3% of those on 12 months of DAPT.
“The recommendations say we should only use PPI in [patients at] high risk for bleeding, so clearly we have a question here concerning the use of PPIs if we want long duration of the DAPT,” he added.
Panelist David Moliterno, MD (University of Kentucky, Lexington), added that it’s also important to look beyond antiplatelet therapy at other factors related to clinical care that impact patient outcomes after PCI, including the use of IVUS or OCT, aggressive pharmacotherapy management, and cardiac rehab.
4D-ACS Results
For the trial, 656 ACS patients (mean age 60 years; 18% women) from three centers in South Korea were randomized to one of two DAPT regimens after PCI with a polymer-free, biolimus-coated stent (BioFreedom Ultra; Biosensors). More than 99% were randomized within 1 day of their procedure.
At 12 months, rates of major bleeding were 0.6% in the 1-month DAPT group and 4.6% in the 12-month DAPT group (HR 0.13; 95% CI 0.03-0.58). Looking across all BARC types, rates were consistently lower throughout follow-up in patients who received short DAPT.
The most frequent type of bleeding was BARC 3b (overt bleeding with a hemoglobin drop ≥ 5 g/dL, cardiac tamponade, bleeding requiring surgical intervention, or necessitating intravenous vasoactive agents), which occurred at rates of 0.3% with short DAPT and 3% with 12-month DAPT (P = 0.027).
There were no significant differences between groups in all-cause death, CV death, MI, ischemia-driven TVR, stent thrombosis, or stroke. There also were no cases of stent thrombosis in any patient during follow-up.
No differences were seen between the groups in ischemic composite endpoints (P = 0.36), and a subgroup analysis showed the treatment effect of 1-month DAPT followed by reduced-dose prasugrel monotherapy was consistent across all ACS subtypes, including unstable angina, NSTEMI, and STEMI.
Approximately 11% of patients in the short DAPT group were at high bleeding risk, as were 13.5% in the 12-month DAPT group. Among these patients, there was a greater benefit of 1-month DAPT versus 12-month DAPT on reducing NACE (HR 0.44; 95% CI 0.21-0.89), but the interaction P value did not reach statistical significance.
Following the presentation, Thomas Cuisset, MD, PhD (CHU La Timone, Marseille, France), who wrote an accompanying editorial, urged caution in extrapolating the results of this all-Asian cohort to other patient populations and pointed out that a specific DES was used, which also limits generalizability of the trial.
Finally, Montalescot said the results of STOPDAPT-3 make it clear that a minimum of 1 month of DAPT is mandatory in ACS to avoid excess ischemic events, but beyond that it seems like any P2Y12 inhibitor is probably fine and should be individualized based on the patient.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Jang Y, Park S-D, Lee JP, et al. One-month dual antiplatelet therapy followed by prasugrel monotherapy at a reduced dose: the 4D-ACS randomized trial. EuroIntervention. 2025;Epub ahead of print.
Cuisset T, Cayla G. DAPT de-escalation post-ACS: a new rule or just a new option? Lessons from the 4D-ACS trial. EuroIntervention. 2025;Epub ahead of print.
Disclosures
- 4D-ACS was funded by Biosensors.
- Kang reports no relevant conflicts of interest.
- Cuisset reports consulting fees and honoraria from Abbott, Boston Scientific, Edwards Lifesciences, Terumo, Medtronic, Inari, BMS-Pfizer, and MicroPort.





Comments