‘Silent’ Brain Infarcts Common, Tied to Cognitive Decline in A-fib
The findings suggest that oral anticoagulation alone may be insufficient for patients with A-fib, one researcher says.
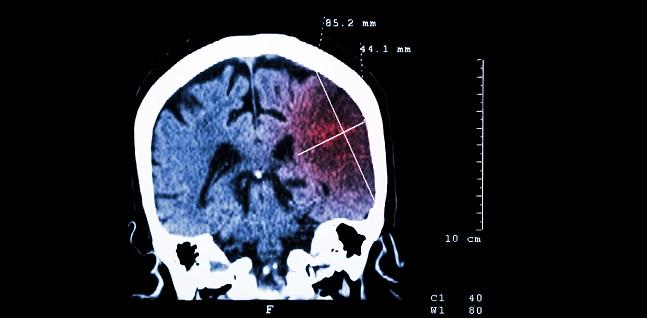
In an A-fib cohort with high use of oral anticoagulation, new brain infarcts—most clinically silent—are commonly detected on MRI. And their presence is associated with small declines in cognitive function over a relatively short time period.
David Conen, MD (McMaster University and Population Health Research Institute, Hamilton, Canada), reported the results at the Heart Rhythm Society (HRS) 2020 Scientific Sessions, held online as a “virtual” meeting last week.
“Although many AF patients benefit from oral anticoagulation, oral anticoagulation alone may not be sufficient to prevent brain damage in all patients with atrial fibrillation,” he concluded during his presentation.
At a press briefing, he argued for a more-comprehensive strategy to treat patients with A-fib. “Don’t get me wrong, I think anticoagulation is crucial, and it’s a very important intervention for many patients with atrial fibrillation,” Conen asserted. “But we also have to treat their blood pressure, their diabetes, their cholesterol. We have to make them stop smoking. And all these factors play an important role.”
Swiss-AF Cohort
In a prior cross-sectional study, Conen’s group observed a high burden of brain lesions on MRI in patients with A-fib, with most being clinically silent. Even those not related to overt strokes or TIAs, however, were associated with lower cognitive scores, “raising the possibility that silent brain damage causes an increased risk of cognitive dysfunction in patients with atrial fibrillation,” Conen said, adding that prospective data are needed.
He and his colleagues turned to the Swiss-AF cohort study, focusing on 1,227 older patients with A-fib who had brain MRIs at baseline and 2 years later. Assessments with validated cognitive tests were performed yearly.
The mean age of the patients was 71; only 26% were women. About half (47%) had paroxysmal A-fib, and 19% had a history of congestive heart failure. Median CHA2DS2-VASc score was 3. Oral anticoagulant use was high, with 90% of patients taking one at baseline and 84% taking one at the 2-year follow-up; it was about a 50/50 split between direct oral anticoagulants (DOACs) and vitamin K antagonists (VKAs), Conen said.
During the 2 years of the study, clinical stroke/TIA occurred in 2.3% of patients, whereas incident large noncortical or cortical infarcts and small noncortical infarcts were detected by MRI in 5.5% of patients. Of the 68 patients with new infarcts on brain MRI, 85.3% had a clinically silent event and 75.0% had a silent event while taking oral anticoagulation.
Cognitive decline tended to be greater in patients with versus without newly detected brain infarcts across five cognitive tests, with the differences reaching statistical significance for three of them.
Asked about the clinical significance of the difference, however, Conen acknowledged at the press briefing that the absolute differences were small “and probably clinically not really appreciable.” He pointed out that cognitive scores improved slightly in the patients without new infarcts, probably because of learning effects, and declined slightly in the patients with infarcts.
“But you also have to remember that this is only a 2-year follow-up and cognitive decline and dementia takes years and decades to develop,” Conen said, adding that he and his co-investigators were surprised to see any statistical differences over such a short span. Larger effects would be expected as these patients are followed over a longer period of time, he said.
Remaining Questions
Providing commentary after Conen’s presentation, HRS President Christine Albert, MD (Cedars-Sinai Medical Center, Los Angeles, CA), said that with this study, “we learned that silent infarcts could be a possible cause, at least in part, for the cognitive decline and dementia associated with AF.”
But there is still much to be learned, she said, pointing to the need to understand possible therapeutic options—like ablation and rate-control medications—to address this, as well as potential differences between DOACs and VKAs. Moreover, Albert said, what impact do various risk factors have on this relationship?
Isabelle Van Gelder, MD, PhD (University Medical Center Groningen, the Netherlands), in an additional commentary, said the study provides interesting data, but she also pointed to some unknowns revolving around time in therapeutic range on warfarin and adherence to the DOACs; the occurrence of other events like heart failure hospitalizations, MIs, cancer, and infections; use of other medications; and how well other comorbidities were treated.
Moreover, Van Gelder said, “their association with cognitive decline, in my view, is not very robust.”
Nonetheless, she concluded, these are “important new data. We await their further analyses.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Conen D. Incidence of silent brain infarcts in anticoagulated patients with atrial fibrillation. Presented on: May 8, 2020. HRS 2020.
Disclosures
- The Swiss-AF cohort study is supported by grants from the Swiss National Science Foundation.
- Conen reports receiving honoraria or speaking/consulting fees from Servier Canada.


Comments