Stroke Thrombectomy Also Benefits Kids, Observational Study Shows
“The sooner those kids come in for medical attention, the better,” an expert says about those with large-vessel occlusions.

Children are less likely than adults to have acute strokes caused by large-vessel occlusions (LVOs), but when they do, endovascular therapy to remove the blockage may be a good option, a small observational study suggests.
Patients younger than 17 years old who had untreated LVO strokes had poorer outcomes compared with those with either non-LVO infarcts or LVO strokes treated with thrombectomy, Kartik Bhatia, MBBS, PhD (Sydney Children’s Hospitals Network, Australia), reported last week at the International Stroke Conference 2022.
About three-quarters of patients with untreated LVO strokes, in fact, had moderate-to-severe disability at 3 months and most (57.7%) maintained that level of impairment several years later. Patients treated with thrombectomy, on the other hand, had outcomes comparable to those seen in patients with non-LVO strokes.
“We have now established that the outcomes in children with an untreated LVO are very poor, and this refutes previous theories that children have better collaterals and better plasticity, and, therefore, you can just leave them alone if they have an LVO,” Bhatia said, noting that children with proximal occlusions have particularly bad outcomes.
“Based on this, we highly recommend that people strongly consider thrombectomy for children when they present with an LVO and that we should make greater efforts to triage and to image children with LVO earlier,” he urged. Moreover, he said, “I think that we should strengthen our stroke treatment guidelines in children to better reflect that we now have natural history data saying that the outcome without treatment is very poor.”
Lack of Data Creates Uncertainty
Though numerous trials have proven thrombectomy to be safe and effective as a treatment for LVO strokes in adults, none of those studies enrolled children, resulting in uncertainty among clinicians when it comes to managing LVOs in a pediatric population, Bhatia said. “And this is exacerbated further by the fact that there is no natural history data available on what happens to a child with a large-vessel occlusion,” he added. Pediatric stroke guidelines provide only weak recommendations on use of mechanical thrombectomy, and it’s unlikely that any randomized trials are forthcoming to inform the issue, as such a trial would be considered unethical at this point considering the overwhelming evidence of benefit in adults, Bhatia indicated.
That means the best evidence will probably come from observational studies like this one. Bhatia and colleagues retrospectively examined all ischemic stroke admissions in patients younger than 17 years of age across four centers in the Australian state of New South Wales—three pediatric hospitals and one adult hospital that treats some older adolescents—between 2010 and 2019.
The analysis included 39 admissions for LVO strokes and 127 (involving 122 patients) for non-LVO strokes. The proportion of LVO to non-LVO strokes is similar to what’s seen in the adult population, Bhatia noted. The LVO group was further divided into patients who underwent thrombectomy (n = 13) and those who did not (n = 26).
Overall, LVO patients were older than those with non-LVO strokes (mean 8.23 vs 5.48 years; P = 0.007). Males were more common than females in both groups, consistent with what has been known about pediatric stroke.
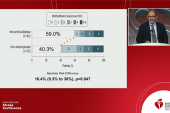
Outcomes were assessed using the pediatric modified Rankin Scale (ped-mRS) score, and at 3 months, the highest rate of favorable outcomes (ped-mRS 0-2) was seen in the non-LVO group (58%), followed by the LVO-thrombectomy group (50%), and then the untreated LVO group (27%). Most patients in that last group (73.1%) had a poor outcome (ped-mRS 3-6).
An ordinal logistic regression analysis confirmed that patients with untreated LVOs had worse outcomes compared with non-LVO patients (OR 3.65) and those treated with thrombectomy (OR 3.75), particularly when the procedure was performed for blockages in the anterior circulation (OR 7.14).
Although the proportion of patients with untreated LVOs who had a poor outcome declined to 57.7% by the end of a mean follow-up of 53 months, this group still had worse outcomes compared with non-LVO patients (OR 3.23) and those who underwent thrombectomy (OR 6.07), particularly when the blockage was in the anterior circulation (OR 8.60).
‘Time is Brain’ a Key Message for Kids
“Now that we know what the outcomes are for these children, there’ll be a much-stronger drive for pediatric neurologists to call for a thrombectomy earlier in the presentation,” Bhatia predicted, noting that in his center, “since I started there and we started promoting this procedure, we now get calls from ICU, from the emergency department, and we start activating the stroke pathway much earlier.” He envisions that over the next 5 to 10 years, networks to facilitate pediatric thrombectomy will solidify, which is expected to have a major impact on the management of children with LVO strokes.
Ashutosh Jadhav, MD (Barrow Neurological Institute, Phoenix, AZ), who was not involved in the study, agreed with Bhatia that it would be tough to do a trial of thrombectomy in children both because of the positive results seen in adults and because of the rarity of strokes in a pediatric population.
The field, then, is reliant on nonrandomized data, Jadhav commented, saying that the findings of the current study align with what has been seen in adults. He agrees with the researchers’ assessment that thrombectomy should be strongly considered in children despite the lack of high-quality evidence seen in adults.
“I think doing a trial to prove this probably is not going to be realistic,” Jadhav said. “It just means that more and more centers need to share their experience and publish it so that we can get some consensus” about the best way to manage these patients.
Aside from the lack of data, he acknowledged other concerns that could hold some physicians back from offering thrombectomy to children. These include issues involving bias in retrospective studies; smaller vessel size, which could require a change in device choice and technique; and beliefs that children are more resilient and more likely to recover from an LVO stroke without endovascular therapy than adults.
But the finding in this study that three-quarters of children who had an LVO and did not undergo thrombectomy had moderate-to-severe disability at 3 months is compelling, Jadhav said. “That’s a very important message to get out—that kids still do badly even with these types of strokes. So it’s not like their recovery is back to normal in most cases.”
The most-critical public health message when it comes to stroke in adults is “time is brain,” Jadhav said, and “this data emphasizes that in the pediatric population, we should be thinking along the same lines.”
This study indicates that children with LVO strokes can do better with thrombectomy, he added, “and the sooner those kids come in for medical attention, the better.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Bhatia K. Pediatric large vessel occlusion stroke: poor outcomes without intervention. Presented at: ISC 2022. February 11, 2022.
Disclosures
- Bhatia and Jadhav report no relevant conflicts of interest.




Comments