Study Bolsters Link Between Silent MI and Ischemic Stroke
Unrecognized MI might help explain a subset of embolic strokes of undetermined source (ESUS).

Older people who’ve had an MI without any clinical symptoms appear to be at risk for subsequent ischemic strokes, according to an analysis of the Cardiovascular Health Study.
Over roughly a decade of follow-up, people who had a silent MI were a relative 47% more likely to have an ischemic stroke after accounting for demographics and vascular risk factors (HR 1.47; 95% CI 1.01-2.16), Alexander Merkler, MD (NewYork-Presbyterian and Weill Cornell Medicine, New York, NY), reported as part of the virtual International Stroke Conference 2021, which begins later this week.
When the results were broken down by stroke subtype, the relationship remained significant for nonlacunar strokes (HR 2.18; 95% CI 1.24-3.83) but not for lacunar or other/unknown strokes.
“This is helpful information, because if you have a stroke we can identify that maybe it’s from having evidence of heart injury from a heart attack,” Merkler told TCTMD. “And this can guide therapy to not only prevent a second stroke, but also may help in future studies looking at what to do in patients who have a silent heart attack and whether they need to have different therapies to prevent them from having a stroke in the first place.”
American Stroke Association spokesperson Christine Holmstedt, DO (Medical University of South Carolina, Charleston), told TCTMD the findings might help explain what’s causing a portion of cryptogenic strokes, or embolic strokes of undetermined source (ESUS), which account for 20% to 30% of all strokes. “If this is a potential etiology, it could help us to prevent future strokes in these patients,” she said.
The Heart-Brain Connection
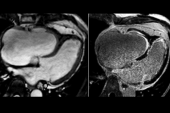
MI accompanied by symptoms is an established risk factor for cardiac embolism and stroke. But MIs aren’t always clinically apparent, and so-called silent or unrecognized infarcts, which have been shown to be about as common as overt MIs, are associated with increased risks of subsequent MI, congestive heart failure, and death.
Prior research has suggested that silent MI may be a risk factor for stroke, too, so Merkler and his colleagues further explored this possibility using the Cardiovascular Health Study, a longitudinal study that enrolled Americans 65 and older in 1989 and 1990. Participants underwent annual ECGs. The current analysis included 4,224 people who did not have prevalent stroke or ECG evidence of MI at baseline.
During a median 9.8 years of follow-up, 10% of participants had a clinically apparent MI, 8.6% had a silent MI, and 8.9% had an ischemic stroke. Of the strokes, 15.1% were lacunar, 36.8% were nonlacunar, and 48.0% were other/unknown.
Consistent with previous studies, overt MI was associated with greater ischemic stroke risks over both the short term (HR 80; 95% CI 53-119) and long term (HR 1.60; 95% CI 1.04-2.44).
For overt and silent MIs, the strongest relationships were seen with nonlacunar strokes, which are more-closely related to cardiac embolism than are lacunar strokes. The proposed mechanism to explain the finding, Merkler said, is that a silent MI damages the heart, increasing LV dysfunction and the formation of thrombi, which can dislodge and eventually cause blockages in the brain. Lacunar strokes, on the other hand, are typically due to plaque buildup in the small arteries of the brain.
“I think it really supports the concept that these are strokes that came from the heart and weren’t just strokes of any etiology,” Holmstedt commented.
Mulling Intensified Therapy
If additional studies confirm the link between silent MI and subsequent ischemic strokes, it might justify changes to clinical management, Merkler said. “These patients may be better served by escalating therapy.”
Standard treatment for ESUS right now is aspirin. However, if it turns out cardiac embolism stemming from silent MI is the culprit, then consideration might be given to starting anticoagulation to prevent future events, he said. Randomized trials to determine the best antithrombotic approach are needed, he noted.
Holmstedt pointed out that researchers are actively exploring potential cardiac causes of ischemic stroke. The ongoing ARCADIA trial, for instance, is randomizing patients with cryptogenic stroke and left atrial cardiopathy to aspirin or apixaban (Eliquis; Bristol-Myers Squibb) to prevent recurrent strokes.
Silent MI “could potentially be another etiology of stroke that we haven’t identified yet and if it is then we could eventually look at aiming our efforts at potentially utilizing different blood thinners for those patients to reduce their risk of embolic stroke,” Holmstedt said.
From primary prevention perspective, it would be premature to advise widespread screening with ECG to look for silent MI as a way to head off even a first related stroke, Merkler and Holmstedt agreed.
“At this point, it’s not ready for clinical practice to say that if you have had a silent MI, you’re definitely at risk for stroke, but that would be the next phase of investigation to really confirm the findings,” Holmstedt said.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Merkler AE. Silent myocardial infarction and subsequent ischemic stroke in the Cardiovascular Health Study. Presented at: ISC 2021.
Disclosures
- Merkler reports receiving an American Heart Association career development award and performing medicolegal consulting on neurological diseases.
- Holmstedt reports no relevant conflicts of interest.




Comments