Subcutaneous GP IIb/IIIa Inhibitor in STEMI Is Fast, Potent in Early Study
The novel injectable antiplatelet, RUC-4, will be further evaluated in the just-started phase IIb CELEBRATE study.

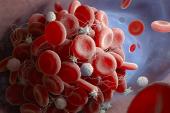
RUC-4 (CeleCor Therapeutics), an investigational glycoprotein IIb/IIIa inhibitor (GPI) administered by subcutaneous injection, provides rapid and powerful platelet inhibition in patients with STEMI, according to findings from Cel-02, a phase IIa study.
Average platelet inhibition 15 minutes after the injection increased across three doses, from 77.5% with the lowest dose to 87.5% with the middle dose and 91.7% with the highest dose (P = 0.002 for trend), Jurriën ten Berg, MD, PhD (St. Antonius Hospital, Nieuwegein, the Netherlands), reported during the virtual EuroPCR 2021.
RUC-4 was well tolerated among the 27 patients in the trial, with one injection-site reaction and two major bleeds, both related to perforation as the guidewire passed through a side branch of the radial artery.
“Single-dose, subcutaneous RUC-4 induces a fast, potent, dose-dependent response of platelet inhibition in patients with STEMI presenting for primary PCI,” ten Berg said during his presentation. “It is therefore promising for prehospital platelet inhibition in STEMI patients.”
The results support additional clinical studies, he said, telling TCTMD that the phase IIb CELEBRATE trial—which aims to enroll about 1,600 STEMI patients in Europe—has just started.
The Cel-02 findings were published simultaneously online in EuroIntervention, with lead authors Willem Bor, MD, and Kai Zheng, MD (both St. Antonius Hospital).
Unmet Need in STEMI
Rapid reperfusion is key to reducing infarct size and improving outcomes in patients with STEMI, but existing drugs for acute treatment have limitations. Oral P2Y12 inhibitors have a delayed onset of action, whereas the intravenous administration of GPIs is inconvenient in a prehospital setting. Intravenous GPIs also have a long duration of effect. Ideally, ten Berg said, there would be an agent that provides rapid platelet inhibition but doesn’t last too long so it doesn’t interact with the oral P2Y12 inhibitors, which take effect within about 2 to 4 hours, to increase bleeding.
RUC-4 is being evaluated for that role. Administered with a single subcutaneous injection, the drug was shown in two phase I studies involving healthy volunteers and patients with stable CAD to induce high-grade platelet inhibition within 15 minutes, with a return to normal platelet function within roughly 2 hours. It was well tolerated up to a dose of 0.075 mg/kg.
Cel-02 moved the research into phase II, testing three doses of RUC-4—0.075, 0.090, and 0.110 mg/kg—in STEMI patients undergoing primary PCI. The study included 27 patients (mean age 62 years; 26% women), with pharmacodynamic data available for 24. RUC-4 was given in a single subcutaneous injection before angiography, with concomitant procedural heparin administered if the activated clotting time (ACT) on arrival was below 200 seconds. Most patients were preloaded with aspirin (93%), ticagrelor (93%), and unfractionated heparin (96%). During PCI, additional heparin guided by ACT was used in 92%.
The primary endpoint was the number of patients with at least 77% inhibition of iso-TRAP-induced platelet aggregation, which is equivalent to 80% inhibition with light transmission aggregometry in response to 20 μM adenosine diphosphate, within 15 minutes. This threshold was achieved by three of eight patients (38%) at the lowest dose and seven of eight patients (88%) in each of the other dose groups.
Maximal platelet inhibition was achieved within 15 minutes. Effects wore off quickly, with a return to 50% of platelet function by about 2 hours.
There was one mild injection-site reaction, with bruising occurring in 11%. Mild access-site hematomas occurred in 22%, whereas there were two severe hematomas (7%).
It’s not clear that the two major bleeds were related to RUC-4, as small perforations can occur in any patient, although it’s possible strong platelet inhibitors can aggravate the issue, ten Berg said. “So you always have to be careful, and I always say to the fellows that if you introduce a sheath and a catheter, you have to use fluoro. You observe where the wire is going, and if it passes easily through the forearm and into the ascending aorta, you are safe, but you should never do it without visualization especially when a patient is on a strong antiplatelet drug.”
Thrombocytopenia—a major disadvantage of the IV GPIs—was not observed in any patient within 72 hours, similar to what was observed in the phase I studies. “That’s because this drug doesn’t modify the glycoprotein IIb/IIIa receptor,” ten Berg explained.
‘Quite Impressive’
Commenting for TCTMD, Pascal Vranckx, MD, PhD (Heart Centre Hasselt, Belgium), said that “modern use of [GPIs] certainly has high potential to optimize the balance between ischemic risk without the excess of bleeding complications, and that’s exactly what we are looking for here.”
Cel-02 represents an important first step in the evaluation of RUC-4 as a treatment in the acute phase of STEMI, he said, noting that “a drug that can achieve an 80% inhibition within 15 minutes, that’s quite impressive.” Even more impressive, he added, was the rapid onset of platelet inhibition followed by a fading of the effect within a few hours. “It gives you enough time to perform the procedure in a safe environment. [Then] you drop to 50%, the other drugs kick in, and you don’t pay the price of bleeding,” Vranckx said. “Of course this has to be established in bigger trials, but at least the concept is there and at least the pharmacokinetics are there. And that’s impressive.”
In emailed comments, Davide Capodanno, MD, PhD (University of Catania, Italy), program chair for EuroPCR 2021, said “the availability of a parenteral agent to bridge the gap in platelet inhibition during primary PCI may be of value, if the net benefit shows to be favorable,” noting that the action of oral antiplatelets may be delayed by slow absorption, cardiogenic shock, vomiting, or an interaction with opioids.
Taking a broader view of the field, Capodanno pointed out “there is some emerging interest in developing parenteral antiplatelet drugs to be administered to STEMI patients in the ambulance or even earlier, as self-medications.” RUC-4 is one, but there is also selatogrel, an injectable P2Y12 inhibitor being developed by Idorsia Pharmaceuticals.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Bor WL, Zheng KL, Tavenier AH, et al. Pharmacokinetics, pharmacodynamics, and tolerability of subcutaneous administration of a novel glycoprotein IIb/IIIa inhibitor, RUC-4, in patients with ST-segment elevation myocardial infarction. EuroIntervention. 2021;Epub ahead of print.
Disclosures
- The study was supported by a grant and materials provided by CeleCor Therapeutics.
- Ten Berg reports lecture or consultancy fees from AstraZeneca, Eli Lilly, Daiichi Sankyo, The Medicines Company, AccuMetrics, Boehringer Ingelheim, Bristol-Myers Squibb, Pfizer, Bayer, Ferrer, and Idorsia; and institutional research grants from ZonMw and AstraZeneca.
- Bor and Zheng report no relevant conflicts of interest.




Comments