Tirofiban Provides Better Platelet Inhibition Than Cangrelor in STEMI Patients
Glycoprotein IIb/IIIa inhibitors are used less frequently in STEMI, but researchers say they may cut risk of ischemic complications.
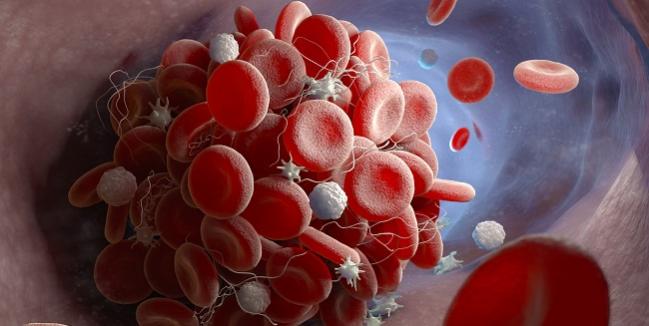
A small study testing the pharmacodynamic effects of several antiplatelet agents suggests that tirofiban (Aggrastat; Medicure), a glycoprotein IIb/IIIa inhibitor, may provide “more potent and consistent” inhibition of platelet aggregation compared with cangrelor (Kengreal; Chiesi) in patients with STEMI undergoing PCI.
Thirty minutes after the initiation of treatment, there was nearly a threefold difference between tirofiban and cangrelor in terms of inhibiting the aggregation of platelets in response to 20 µmol/L adenosine diphosphate (ADP). Both cangrelor and tirofiban were superior to chewed prasugrel for the inhibition of platelet aggregation. Chewed prasugrel did not inhibit platelet aggregation any better than the standard integral administration of prasugrel.
Marco Valgimigli, MD, PhD (Bern University Hospital, Switzerland), who presented the study at the PCR e-Course 2020, said that integral pill administration of oral P2Y12 inhibitors, such as prasugrel or ticagrelor, provides suboptimal early inhibition of platelet aggregation in STEMI patients undergoing primary PCI. Some smaller, single-center studies have suggested that chewing or crushing P2Y12 inhibitors might increase early drug availability and improve platelet inhibition.
The parenteral agents, on the other hand, have been shown to provide rapid and sustained inhibition of platelet aggregation compared with P2Y12 inhibition, but there are no comparative data on platelet aggregation inhibition with cangrelor and tirofiban in primary PCI patients, and no data on how well these agents might perform against chewed prasugrel.
Inhibition of Platelet Aggregation
In FABOLUS-FASTER, which was published simultaneously in Circulation, the researchers randomized 122 patients to cangrelor, tirofiban, or prasugrel. Cangrelor and tirofiban were administered as a bolus and 2-hour infusion followed by 60 mg of prasugrel, while prasugrel was given as a 60-mg loading dose with these patients then randomized again to receive either chewed prasugrel or integral tablet administration after loading.
With tirofiban, the percentage of inhibition of platelet aggregation after stimulation of platelet-rich plasma with ADP was 95.0% compared with 34.1% for patients treated with cangrelor (P < 0.001). As such, cangrelor failed to meet the criteria for noninferiority compared with tirofiban. With chewed prasugrel, the inhibition of platelet aggregation was 10.5%, which also failed to meet the criteria for noninferiority compared with cangrelor or tirofiban. With prasugrel alone, the patients who chewed the drug had a higher active metabolite concentration compared with standard administration, but there was no difference in the inhibition of platelet aggregation.
“It is notable to emphasize that tirofiban was associated with superior inhibition of platelet aggregation throughout the entire duration of the study, up to 4 to 6 hours,” said Valgimigli. “Cangrelor was associated with higher inhibition of platelet aggregation at 15 or 30 minutes, as well as 1 hour, compared with prasugrel. However, the inhibition of platelet aggregation did not differ any more at 2 hours, and subsequently, namely at 3 or 4 to 6 hours, prasugrel, either chewed or integral, was associated with higher inhibition of platelet aggregation compared with the cangrelor group.”
In their paper, Valgimigli and colleagues, led by Giuseppe Gargiulo, MD, PhD (Bern University Hospital), say that given the potent inhibition of platelet aggregation, tirofiban “may be more effective than cangrelor in reducing the risks of acute ischemic complications.” However, they stress that this hypothesis needs to be tested further, particularly in a study powered for clinical endpoints. They note that use of glycoprotein IIb/IIIa inhibitors in STEMI has declined out of concern for bleeding, but the clinical data on their use are mainly based on a prolonged post-bolus drug infusion and femoral access at the time of PCI.
Some Welcome Data
For Christoph Naber, MD, PhD (Contilia Heart and Vascular Center/Elisabeth Krankenhaus, Essen, Germany), the discussant following the presentation, the present study provides some welcome data on the antiplatelet inhibition effects of modern therapeutic regimens in ACS. “This study showed that there are differences between the different [drugs] and we can measure them,” he said. However, one of the study’s limitations is whether the platelet inhibition in response to ADP in vitro translates into real in vivo effects.
“We know that platelets are activated by multiple mechanisms and the ADP pathway is just one of them,” he said.
Naber added that one interesting aspect of the study is that the largest difference in the inhibition of platelet aggregation was observed with the glycoprotein IIb/IIIa inhibitor tirofiban, which is primarily used as a bailout option when complications arise during PCI, compared with the other agents. In fact, the observed differences between cangrelor and prasugrel were relatively small, and whether the observed differences are enough to warrant switching to cangrelor is uncertain, he noted.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Gargiulo G, Esposito G, Avvedimento M, et al. Cangrelor, tirofiban, and chewed or standard prasugrel regimens in patients with ST-segment elevation myocardial infarction: primary results of the FABOLUS FASTER trial. Circulation. 2020;Epub ahead of print.
Disclosures
- Valgimigli reports grant support from Medicure; grant and personal fees from Abbott, Alvimedica, Amgen, Bayer, Bristol-Myers Squibb, Coreflow, Daiichi-Sankyo, Vifor, Idorsia, Terumo, iVascular, and AstraZeneca.


Comments