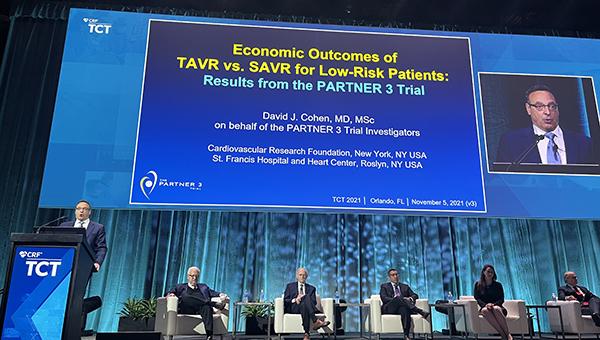
TAVI Edges Out Surgery in 2-Year Costs for Low-risk Patients: PARTNER 3
The findings confirm “we are not bankrupting the healthcare system,” says David Cohen.
In patients with severe aortic stenosis at low surgical risk, the overall cost of TAVI with the Sapien 3 valve (Edwards Lifesciences) is about $2,000 less than for surgical AVR at 2 years, thanks to lower follow-up costs with the transcatheter procedure, according to new PARTNER 3 data.
In the United States, valve price drives the initial cost difference, which was $26,600 higher for TAVI in this trial, but researchers predict increased competition from emerging new devices will bring prices down, eventually cementing the cost-effectiveness of the transcatheter procedure.
Prior data in intermediate-risk patients has shown substantial cost-effectiveness favoring TAVI over surgery. Also, the 3M TAVR study published earlier this year demonstrated $11,000 in savings with a minimalist versus standard TAVI pathway at 30 days.
“We've come a very, very long way over time,” David Cohen, MD (St. Francis Hospital and Heart Center, Roslyn, NY, and Cardiovascular Research Foundation, New York, NY), who presented the findings today in a late-breaking trial session at TCT 2021, told TCTMD. “I think in the earliest days of TAVR, we could've never expected to match surgical AVR for these low-risk patients both clinically [and] economically.”
These results matter because “we need to know that we're not bankrupting the healthcare system with all of this advanced technology and these less-invasive procedures,” he continued. “These results are very reassuring that despite the much higher cost of the valve we're actually saving the health system money at least at 2 years.”
Commenting on the study for TCTMD, Edward Chen, MD (Duke University Medical Center, Durham, NC), said the findings “are extremely important to know because as we continue to improve upon the care that we provide our patients with cardiovascular disease, particularly in the structural heart arena, I think it's important that we not only demonstrate quality in these innovative therapies and these new therapies, but also value. . . . This is important information, and I look forward to seeing how this value will trend over a time period beyond 2 years, maybe to the 5- or 10-year mark.”
Clinical events over time will likely tell the economic story out to 10 years, Cohen said. “It's unlikely I think that the costs will catch up over time especially if the valve prices come down. It's really going to be whether there are meaningful differences in durability of the valve or in survival. That's really what's going to drive things.”
Competition, Durability
For the study, Cohen and colleagues linked Medicare claims to the 1,000 low-risk patients in PARTNER 3 who underwent SAVR or TAVI with the Sapien 3 device. Valve cost can vary among hospitals, so for the purposes of the study, the researchers assumed a base device price of $32,500 for TAVI and $5,900 for SAVR.
During the index hospitalization, procedure duration was lower (mean 59 vs 208 minutes) and length of stay was shorter (mean 1.9 vs 6.5 days)—including ICU time (mean 0.8 vs 2.7 days)—for TAVI than for surgery (P < 0.001 for all). Additionally, more TAVI patients were discharged to home (95.9% vs 73.1%; P < 0.001). This translated to comparable index hospitalization costs for both TAVI and surgery ($47,196 vs $46,606; P = 0.59).
However, follow-up costs were significantly lower for TAVI from discharge to 30 days (-$3,896) and from 30 days to 6 months (-$1,506; P < 0.05 for both). From 6 to 12 months and 12 to 24 months, respectively, TAVI was $1,072 and $1,710 more expensive. As such, total 2-year follow-up costs were $2,620 less for TAVI compared with surgery ($19,638 vs $22,258; P = 0.13). This translated to a $2,030 cost difference favoring TAVI at 2 years inclusive of index hospitalization costs ($66,834 vs $68,864; P = 0.31).
“That difference wasn't statistically significant by conventional standards,” Cohen explained, noting “that doesn't really matter when we're doing these economic analyses.”
Additionally, there were early quality-of-life benefits as well as a small difference in early mortality for TAVI which led to a 0.05 benefit in quality-adjusted life-years with TAVI over surgery (1.95 vs 1.91). This benefit might not sound like much, “but it's actually twice the amount of benefit that drug eluting stents adds and it's similar to the amount of benefit that we saw in PARTNER 1,” Cohen said.
Lastly, in a bootstrap analysis replicating the trial 2,000 times, he explained that the result remained in favor of TAVR 95% of the time.
“Now that's not the end of the story, obviously,” he said. “If there are no differences in outcomes beyond 2 years, that is the story. The cost-effectiveness will hold and that's our primary assumption, that there isn't a meaningful difference in survival or quality of life beyond 2 years, but we have to wait another 8 years to find that out.”
Sensitivity analyses showed that with as small as a 4% relative survival advantage favoring SAVR “the whole story flips around and surgical AVR would be more cost-effective,” Cohen said. “But that's uncertain at the present time. We don't have any evidence that's the case. Right now, the data we have says the survival is almost identical. It's actually still a little bit in favor of TAVR, but time will tell.”
The two subgroups where TAVI would be most cost-effective included patients who were most symptomatic preprocedure—those who had class 3 or 4 heart failure or patients with Kansas City Cardiomyopathy Questionnaire scores of less than 70. “In those patients, the 2-year cost savings weren't $2,000, they were actually $6,000-7,000, so a much greater cost savings in those groups,” Cohen noted.
Additionally, if the price of the TAVI valve dropped to $25,000, say, “the cost difference at 2 years would be almost $10,000 in favor of TAVR,” he said. “So again, all of these things kind of line up to say that right now it appears that TAVR is economically dominant or at least a highly cost-effective therapy, but we need to wait for the 10-year data to really know for sure whether that is the case or whether there is some long-term difference that changes things dramatically.”
All of these things kind of line up to say that right now it appears that TAVR is economically dominant or at least a highly cost-effective therapy, but we need to wait for the 10-year data to really know for sure. David Cohen
As more TAVI valves are developed around the world, Cohen said their price will likely come down. “The drug-eluting stent story was that once there were three devices on the market, the prices started to come down and they are continuing to decrease today,” he said. “I remember when drug-eluting stents were first introduced in 2003 they cost $3,000 a stent and now they cost about $800 a stent, and so I believe that with competition and plateauing of the market that there will be reductions in the price of the valve. But I wouldn't dare to guess how quickly and to what level. It's hard to predict the future.”
Chen agreed. “I do think that competition breeds results in these types of trends in lowering cost, but also more importantly improving quality,” he said. “I would hope that would happen and it certainly appears that would be the case.”
Commenting on the study during a press conference, Luca Testa, MD, PhD (IRCCS Policlinico S. Donato, Milan, Italy), said the findings are “hard to translate from a European perspective, . . . but I must say that the picture is still incomplete because in order to have a final word we need to see [durability outcomes].”
Surgical valves have data out to 15 years or longer, “but this is not the case for TAVR,” he added. “I will say that I'm pretty reassured because what we are doing it looks very cost-effective from an economic perspective but also very reassuring in terms of long-term follow-up. Well not that long, but that's what we have.”
Of note, Cohen et al’s analysis was conducted entirely among patients in the United States, so these numbers may not necessarily hold up in other countries where relative costs are different. As Milan Milojevic, MD, PhD (Dedinje Cardiovascular Institute, Belgrade, Serbia), observed when discussing the SURTAVI results with TCTMD earlier today, TAVI may cost more than surgery in middle-income countries.
Cohen said this may very well be true. “This analysis is 100% a US analysis, and I couldn't honestly guess what the results would look like outside of the US because there are at least two factors that are different,” he said. “One is that valve prices are lower outside of the US, no question. And then the second is that a lot of the benefit is reducing the number of hospitalizations, rehab days, and hospital days, and those are cheaper outside the United States too. So the balance of those factors is not something that I can really predict. I think it is uncertain, and this analysis would need to be redone outside of the United States.”
Note: An earlier version of this story incorrectly stated that follow-up TAVI costs were significantly lower than surgery at all time points through 2 years. The story has been updated to show that the costs were only significantly lower through 6 months.
Cohen is an employee of the Cardiovascular Research Foundation, the publisher of TCTMD.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Cohen DJ. Economic outcomes of TAVR vs. SAVR for low-risk patients: results from the PARTNER 3 trial. Presented at: TCT 2021. Orlando, FL. November 5, 2021.
Disclosures
- Cohen reports grant support/research contracts from Abbott Vascular, Ancora Heart, Boston Scientific, Corvia, Edwards Lifesciences, Medtronic, Svelte, Volcano Corporation, and V-Wave Medical; and consulting fees/honoraria/speaking fees from Abbott, Boston Scientific, and Medtronic.
- Chen and Testa report no relevant conflicts of interest.




Comments