Transcatheter Tricuspid, Mitral Repair Appear Safe to Combine: Registry Data
Compared with TMVR alone, the dual approach was linked to better survival. But many unknowns remain.
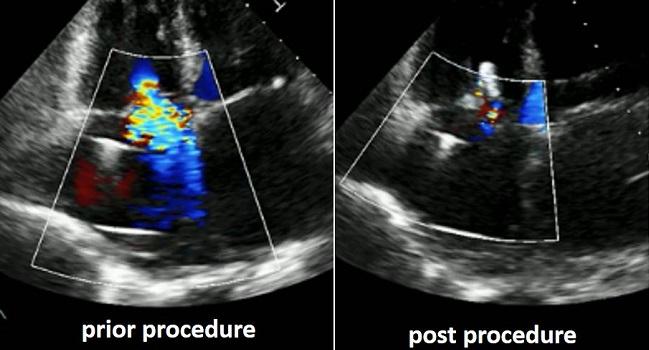
In high-risk patients undergoing MitraClip implantation for the treatment of severe mitral regurgitation (MR), it’s safe and even beneficial to also address severe tricuspid regurgitation (TR), suggests a retrospective look at data from the TriValve and TRAMI registries.
Performing tricuspid repair on top of transcatheter mitral valve repair (TMVR) was linked to significantly lower mortality risk at 1 year, even after adjustment for potential confounders.
“MR and TR often coexist. Although concomitant treatment of both valves is indicated during mitral surgery, it is unclear whether both valves should be treated simultaneously using a percutaneous approach,” Michael Mehr, MD (Ludwig-Maximilians-Universität, Munich, Germany), and colleagues note in their paper published online recently in JACC: Cardiovascular Interventions.
Ran Kornowski, MD (Rabin Medical Center, Petach Tikva, Israel), in an accompanying editorial, agrees that the best solution isn’t yet known.
Dual transcatheter mitral/tricuspid repair “is a new intervention, the technique is quite complicated and not yet refined, and its overall prognostic value as a ‘stand-alone’ procedure is yet to be determined. Thus, the indication for [tricuspid intervention] in the context of TMVR is still ambiguous, as is the timing of performing the tricuspid edge-to-edge repair,” he explains. For example, it might make more sense to first treat the MR then wait 1 to 3 months, in order to see whether the TR resolves.
That said, “this pioneering work holds great promise and potential clinical value” by providing a peek at the best strategy and a basis for future research, Kornowski says.
Speaking with TCTMD, Mehr also cautioned against drawing too many conclusions just yet, calling the current findings “hypothesis-generating” but interesting enough to pursue further. “These are very sick patients, and we have to do anything we can to improve prognosis and their symptoms,” he observed.
TRAMI and TriValve Together
The investigators compared 106 patients in the German TRAMI registry who underwent isolated TMVR with 122 patients in the international TriValve registry who also underwent concurrent tricuspid repair in compassionate and/or off-label use of MitraClip (Abbott). All had both severe MR and severe TR.
Mean age of the overall cohort was 77, and 44.3% of participants were women. All had significant dyspnea at baseline (93.9% were NYHA functional class III or IV), and there were no differences between the two groups with regard to pulmonary hypertension or chronic pulmonary disease.
Combined tricuspid/mitral patients were less likely to have LVEF < 30% compared with the TMVR group (P < 0.001), had lower estimated glomerular filtration rates (40 vs 46 mL/min; P = 0.021), and had a smaller median left ventricular end-diastolic diameter (54 vs 59 mm; P = 0.007). They were more likely to present with A-fib (68.7% vs 55.7%; P = 0.029) and be in NYHA functional class IV (32.8% vs 18.9%; P = 0.013).
The two groups saw similar procedural success and comparable reductions in MR. In-hospital rates of major adverse cardiac and cerebrovascular events also were equivalent, with the tricuspid/mitral group having a trend toward shorter median hospital stay (5 vs 7 days; P = 0.051).
At 30 days, mortality rates were similar in the two groups. By 1 year, however, patients who received a combo procedure were significantly less likely to have died than those who underwent TMVR (16.4% vs 34.0% = 0.035). Multivariate analysis showed that mortality was nearly halved with concurrent treatment versus TMVR alone (HR 0.52; P = 0.02). Slightly more than two-thirds of patients in each group were in NYHA functional class II or less at 1-year follow-up.
New Directions
The improvement with the combined approach makes sense, she told TCTMD. If two valves are severely leaking but only one is repaired, the heart would be expected not to perform as well as if both had been fixed. Most importantly, though, the paper “at least is telling us that [this strategy] is safe,” Guerrero said. “However, we should not encourage teams to start implementing this strategy routinely for all patients. The best approach is to consider enrolling in clinical trials to help obtain the scientific data needed to better understand which is the best treatment.”
Availability of transcatheter—rather than surgical—mitral valve repair is key to new possibilities in the management of tricuspid regurgitation, Mehr et al assert.
“Patients in both registries had both severe TR and dilated annuli and would therefore have undergone tricuspid repair if they underwent mitral surgery according to current guidelines. However, contrary to surgery, after a previous percutaneous mitral intervention, redo percutaneous procedure to treat TR does not carry an increased risk for complications; notably, the pericardial adherences that complicate redo cardiac surgery are not encountered with percutaneous procedures,” the investigators point out. Like Kornowski, they note that a staged procedure “might avoid unnecessary tricuspid procedures in cases in which spontaneous TR reduction occurs after MR treatment.”
Prognosis for these very sick patients is poor, Mehr emphasized to TCTMD. This raises questions about whether a combined or staged procedure would serve them best. “The other thing that is not known is: how long should we wait? There is not much data on the development of TR after repairing the mitral valve. The only thing that is known is that the degree of TR in TMVR is a very clear predictor of mortality. And so, the goal should be to reduce TR” without too much of a delay, advised Mehr.
Kornowski outlines several limitations to the current study, including inherent differences in the patient cohorts and the absence of certain echocardiographic details. Despite these reservations, Mehr and colleagues “should be commended on providing original and fair data from two cohorts of edge-to-edge valvular treatment,” he comments. “The strength of this study lies in its novelty, the relatively large number of patients in each group, and in the unselected nature of the cohort of patients with MR and TR pathology.”
Mehr said there is still a lot to learn before attempting a prospective, randomized trial. Moreover, he added, apart from MitraClip there are other techniques and dedicated devices emerging for the treatment of TR; each would need to be explored individually when combined with TMVR.
Photo Credit: Michael Mehr
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Mehr M, Karam N, Taramasso M, et al. Combined tricuspid and mitral versus isolated mitral valve repair for severe mitral and tricuspid regurgitation: an analysis from the TriValve and TRAMI registries. J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Kornowski R. Managing combined mitral and tricuspid regurgitation: should we clip the percutaneous clip procedures? J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Disclosures
- Statistical analysis for this paper was supported by an unrestricted grant from Abbott Medical. The TRAMI registry received support from Abbott Vascular. The TriValve registry was not supported by external funding.
- Mehr, Kornowski, and Guerrero report no relevant conflicts of interest.


Comments