Unplanned PCI Rare After TAVI, but Operators Get Good Results
In the first 2 years, PCI was mainly for ACS, but chronic disease with symptoms or ischemia was the leading indication thereafter.
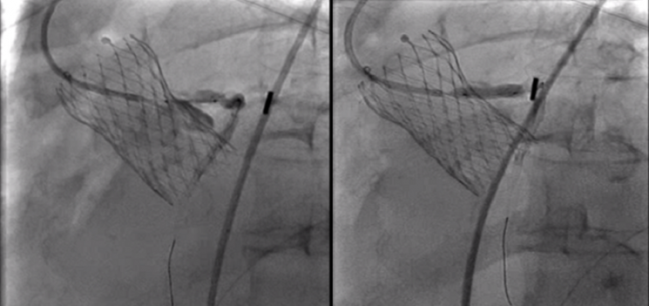
Photo Credit: Prasad A. Case Review: Complex PCI Post-TAVR Implant. Presented at: TCT 2019. September 27, 2019.
Unplanned PCI following TAVI is rare, but when necessary, interventionalists are almost always able to successfully revascularize the occluded artery, according to data from an international registry. The incidence of unplanned PCI is highest in the first week after TAVI, declining over time, and the most common reason for the procedure in the first 2 years after valve implantation is acute coronary syndrome, particularly NSTEMI, according to researchers.
Interestingly, the type of valve implanted had no impact on PCI outcomes, with operators reporting similar rates of successful revascularization in those treated with balloon-expandable and self-expanding bioprostheses. The self-expanding Evolut (Medtronic) valve, with its taller frame, is thought by some to make coronary reaccess more difficult when compared with other valve types.
“The issue of reaccess after TAVI is becoming increasingly important,” lead investigator Giulio Stefanini, MD, PhD (Humanitas Clinical and Research Center BRCCS, Milan, Italy), told TCTMD. “Once you move from the elderly to a younger patient population treated with TAVI, you need to face the issue of coronary artery disease, which might not be present at the time of TAVI but which may become clinically significant over time. These are patients who might require revascularization but it’s not coronary artery disease you were aware of prior to the procedure. It’s something that now requires clinical attention.”
Published January 18, 2021, in JACC: Cardiovascular Interventions, the observational study includes 15,325 patients who underwent TAVI between July 2008 and 2019 at one of 20 European centers participating in the REVIVAL registry. Just 0.9% of patients had an unplanned PCI after valve implantation, after a median delay of 191 days. Their mean age was 80.1 years, and the vast majority (78%) of those requiring PCI were men.
Among the 133 patients who underwent unplanned PCI, the most common indication was ACS, with 15.4% of patients presenting with unstable angina, 32.3% with NSTEMI, 9.8% with STEMI, and 2.2% with cardiac arrest. Additionally, 40.6% of patients required PCI for stable coronary artery disease, including 25.2% for angina symptoms and 15.4% with evidence of ischemia. Over time, there was a shift in the indication for PCI. In the first 2 years after TAVI, ACS was the leading indication for PCI, but chronic coronary syndromes were the reason for revascularization from then on.
“Of course, this is preliminary evidence,” said Stefanini. “This is a relatively small registry, although it’s the largest available to date. The interesting aspect is that this is rare—it’s not a frequent occurrence to have PCI after TAVI that isn’t planned upfront.”
Regarding ACS occurring in the first 30 days, Stefanini said while it’s possible these acute events requiring revascularization might be caused by the TAVI procedure, a good proportion are likely the result of coronary lesions not considered significant prior to aortic valve replacement. After the valve is replaced it might become apparent that the coronary lesion is also clinically relevant. “We should always think, from a pathophysiological standpoint, that the aortic valve stenosis is predominant in determining the majority of the patient’s symptoms,” said Stefanini. “In that setting, for example, you might not consider a 50% stenosis of proximal LAD relevant, since it’s not angiographically significant. You might not think the symptoms are caused by that [coronary] stenosis, but after TAVI, the patient continues to be symptomatic.”
Overall, 63.9% of those requiring PCI had received a self-expandable bioprosthesis, mainly CoreValve or CoreValve Evolut. For those who received a balloon-expandable device, Sapien, Sapien XT, or Sapien 3 (Edwards Lifesciences) were the valves implanted. The overall success rate for PCI was 96.6%, with no significant differences between patients who received the self-expanding and balloon-expandable valves (94.9% vs 100%; P = 0.150). Additionally, there was no difference in the number of diagnostic or guiding catheters used, total fluoroscopy time, or vascular access during PCI among patients treated with the two valve types.
“The registry suggests very good outcomes in the acute phase after TAVI, and also good clinical outcomes over time, without any major differences in terms of reaccess between self-expanding and balloon-expandable valves,” said Stefanini. “Of course, again, we’re talking about an observational study—it’s not conclusive, but it does provide some preliminary data.”
Half of TAVI Patients With CAD
In an editorial, Duk-Woo Park, MD, PhD, and Seung-Jung Park, MD, PhD (University of Ulsan College of Medicine/Asan Medical Center, Seoul, Korea), also urge caution interpreting the results, noting that there was no systematic prospective evaluation of these unplanned PCIs. Also, without a control group, it’s not possible to identify potential predictors or risk factors of rare unplanned PCI, nor is it possible to determine the exact cause or mechanism leading to unplanned revascularization after TAVI.
Ankur Kalra, MD (Cleveland Clinic, OH), who wasn’t involved in the study, said that epidemiological data suggests 50% of patients undergoing TAVI also have concomitant coronary artery disease. The present study, he said, shows that coronary access isn’t hindered by the valve implantation. “Coronary access is a hot topic as we deploy these valves in patients at low risk for mortality following surgical aortic valve replacement,” Kalra told TCTMD. “This study shows very nicely that there were no issues accessing the coronaries in upwards of 95% of the cases. No issues engaging the guiding catheter and performing PCI even with the valve in.”
With the recognition that future coronary access might be needed, interventional cardiologists are now aiming to achieve commissural alignment so that the valve struts do not block the coronary arteries, he added. Also, Kalra noted, the majority of patients requiring unplanned PCI had an ACS, suggesting there was some stable coronary disease that clinicians initially felt could be left untreated. The field, he added, is moving away from treating stable coronary lesions with PCI and the present study offers some reassurances. Back in 2019, Kalra published and presented a meta-analysis showing that revascularization of stable CAD before or at the time of TAVI did not improve clinical outcomes compared with patients who didn’t undergo PCI.
“Even if you have stable disease which you don’t think is contributing to the patient’s symptoms, either chest pain or shortness of breath, and you think it’s the valve causing the symptoms, you can just leave [the coronary lesion] alone and don’t revascularize it,” he said. “If the patient presents later with an acute coronary syndrome, and where you now have an indication to revascularize, simply having a TAVR valve doesn’t preclude them from having a procedure. From that perspective, it’s very reassuring.”
For his part, Kalra doesn’t think ACS in the first 30 days is related to the TAVI procedure. The stress of TAVI leading to plaque rupture or erosion is one hypothesis, and potentially worth studying; however, he doesn’t see a “cause and effect” between TAVI and subsequent ACS, nor is it something that can be gleaned from this observational study.
In their editorial, Park and Park point out that the prognostic effect of CAD on clinical outcomes in patients undergoing TAVI remains controversial. Right now, there are no definitive data on the most appropriate revascularization strategy or any information on its optimal timing. Instead, individualized management based on clinical and angiographic findings is usually how contemporary practice is done.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Stefanini GG, Carrato E, Pivato CA, et al. Unplanned percutaneous coronary revascularization after TAVR: a multicenter international registry. J Am Coll Cardiol Intv. 2021;14:198-207.
Park D-W, Park S-J. Unplanned coronary intervention after TAVR: timing, causes, and management. J Am Coll Cardiol Intv. 2021;14:208-210.
Disclosures
- Stefanini reports institutional research grant support from Boston Scientific and speaker/consultant fees from B. Braun, Biosensors, and Boston Scientific.
- Park and Park report no conflicts of interest.





Comments