Uproar Continues Over UK NICE Guidelines Restricting EVAR for AAA
Although the recommendations have yet to be published, the draft document and its writing committee are under fire.
The full guidelines have yet to be released, but as a session here at the 46th Annual VEITHsymposium made abundantly clear, the outcry shows no signs of dying down.
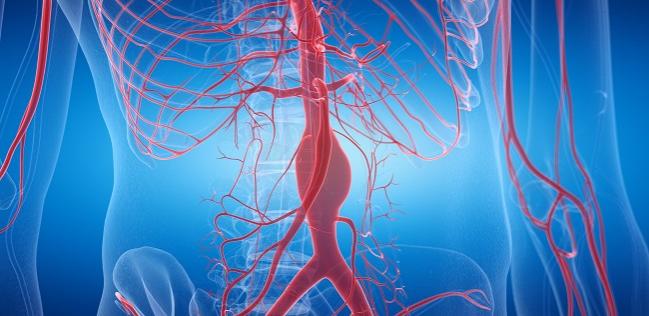
"It's actively withdrawing EVAR, despite the safety and efficacy we have in the literature,” said Dittmar Böckler, MD (University of Heidelberg, Germany). He added that in its current state, the guideline document "contradicts good clinical practice" and is "unacceptable" in recommending surgery only or no intervention for patients with unruptured aneurysms.
During his presentation, Michael P. Jenkins, MBBS (Imperial College London, England), noted that there was unprecedented feedback during the open comment period after the draft was released last year. "Publication deadlines have come and gone, the committee was actually discharged in July, and we still don't have a publication date," he added.
“They basically set up a biased panel of people who are anti-endo and anti-EVAR and pro-open surgery,” session moderator and VEITHsymposium chair Frank J. Veith, MD (Cleveland Clinic, OH, and New York University, New York, NY), told TCTMD. “It’s bad for patient care. I think they ought to have the courage to reexamine the data and back away from this absurd guideline.”
Grading the Data
Nicholas J. Cheshire, MD (Imperial College London), took exception to the way the NICE committee graded the quality of evidence from the four pivotal RCTs of EVAR for AAA (DREAM, OVER, EVAR-1, and ACE), saying that they used "fancy statistical manipulation" to grade two of the trials as providing "very-low-quality evidence.” The EVAR-1 trial, which suggested that the early mortality benefit of EVAR over surgery may be lost over the long term, was graded as having the highest-quality evidence. What that essentially means, said Cheshire, is that "no matter how you cut it,” the excess EVAR deaths were guaranteed to be more meaningful to the NICE committee than excess surgical deaths.
It’s bad for patient care. I think they ought to have the courage to reexamine the data and back away from this absurd guideline. Frank J. Veith
UK NICE writing committee chair Andrew W. Bradbury, MD (Heart of England NHS Foundation Trust, Birmingham, England), who attended the VEITHsymposium session, said he asked permission from the NICE committee to present some new analyses that have been performed in response to the feedback referenced by Jenkins, but was told they are embargoed until the final guideline is published sometime in 2020.
Instead, Bradbury showed cost-effectiveness data that the NICE committee factored into its decision, which included the most recently available RCT and non-RCT clinical and economic data. In a sensitivity analysis, EVAR was more expensive 100% of the time, Bradbury said, with only 0.1% of EVAR procedures meeting the threshold for cost-effectiveness despite early health gains associated with better perioperative survival and quality of life.
"Even if you double or triple your willingness-to-pay threshold, you are not going to get cost-effective outcomes,” he added.
But Cheshire disagreed, telling Bradbury, "You've got some of the right data, but it's a wholly inappropriate interpretation.”
Among the most troubling aspects of the looming guideline, said Böckler, is that patient choice is not being factored into treatment choice. Additionally, he pointed out that "if you are not routinely performing elective EVAR in your hospital, would you be able to deliver an emergency EVAR service for rupture as recommended? The answer is no."
Impact on Decision-Making and Options
Frans L. Moll, MD, PhD (University Medical Center Utrecht, the Netherlands), agreed with Veith that the NICE committee, which was composed of individuals with no connection to industry, was biased in their decision-making.
"It's a bias, and it's wrong to presume that people who have no consultancy [with industry] would be more neutral than colleagues who have a consultancy,” he said. Moll also criticized the NICE committee for not giving proper consideration to evidence from well-done prospective, observational studies, choosing instead to make their decision based primarily on randomized trials they knew were underpowered.
At the end of the session, Veith asked the audience what they would choose for themselves if they had an AAA. Approximately one-third said open surgery and two-thirds said EVAR.
“I hardly ever see any patients who when you talk to them about it, want an open repair,” observed session co-moderator Ali F. AbuRahma, MD (West Virginia University, Charleston), who added that he wondered how UK physicians will manage their patients if they are forced to follow the guidelines and withhold EVAR.
Hopefully the agony will be over early in the new year, and when you see that new analysis, you can decide for yourself whether it stacks up for you and your country and your practice. Andrew W. Bradbury
Bradbury, a vascular surgeon, noted that he believes additional health and economic analyses that have been done since the draft was released will help clinicians better understand why UK NICE came to their decision.
“Hopefully the agony will be over early in the new year, and when you see that new analysis, you can decide for yourself whether it stacks up for you and your country and your practice,” he said.
To TCTMD, Veith said this issue will continue to be debated despite the fact that there is no signal that the committee plans to change their mind and limit the restrictions on EVAR in their final document. He added that he hopes the feedback from around the world will show the UK NICE guideline writers how out of step they are being in their decision-making and how their recommendations could potentially influence those of other countries.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Böckler D. Why the NICE AAA Guidelines reached the wrong conclusions – that EVAR benefits were not worth the costs. Presented at: VEITHsymposium 2019. November 19, 2019. New York, NY.
Cheshire NJ. Why the early survival benefit for EVAR versus open repair outweighs the late survival benefit for open repair versus EVAR. Presented at: VEITHsymposium 2019. November 19, 2019. New York, NY.
Bradbury A. Highlights of the UK NICE guidelines for treating elective and ruptured AAA. Presented at: VEITHsymposium 2019. November 19, 2019. New York, NY.
Jenkins MP. The NICE AAA guidelines are misleading and unfairly biased against EVAR. Presented at: VEITHsymposium 2019. November 19, 2019. New York, NY.
Disclosures
- Bradbury, Jenkins, Cheshire, and Böckler report no relevant conflicts of interest.


Comments