VASCADE Closure Device: FDA Database Tracks Common Complications, Deaths
While the voluntarily reported MAUDE numbers can’t be used to calculate rates, they do raise awareness, Ron Waksman says.

VASCADE, developed by Cardiva Medical, which was acquired earlier this year by Haemonetics Corporation, received FDA approval in January 2013 based on the RESPECT pivotal trial. In that 420-patient study, minor event rates were 1.1% for VASCADE and 7% for manual compression; neither arm experienced any major access-site-related complications.
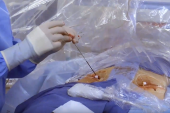
Meant for use with up to a 7-Fr inner diameter sheath, VASCADE delivers a bioabsorbable collagen-based patch to achieve hemostasis of mid-bore femoral access sites.
Senior author Ron Waksman, MD (MedStar Washington Hospital Center, Washington, DC), said this study is one of several by their group to pull numbers from the FDA’s Manufacturer and User Facility Device Experience (MAUDE) database. Other papers have focused on topics as diverse as large-bore closure devices (Abbott’s Prostar XL and Perclose ProGlide plus Essential Medical’s MANTA), rotational atherectomy, cerebral protection in TAVI, and guide extension catheters in PCI. The latest report was published in Catheterization and Cardiovascular Interventions.
To TCTMD, Waksman stressed that since MAUDE doesn’t capture the “denominator” of how many devices are in use, its reports can’t be used to calculate actual prevalence. Still, he said, it offers a glimpse at how devices are performing.
It’s not surprising to see more complications as a new product is adopted, he said. “When you do a trial for approval today, obviously you do a very careful selection of patients [and] you focus on training of the operators or investigators. You expend all that effort. Once the device is approved for marketing, usually you do have [monitoring] but the level of scrutiny about patient eligibility and training is not at the same level [as before].”
Waksman emphasized that physicians need to report their experiences to MAUDE, despite the limitations of a voluntary database. “It’s a good thing. We have to develop more awareness and know what to expect [or] not expect,” he said.
An important message is that “not all closure devices are the same,” said Waksman. They have different mechanisms of action, are geared toward certain settings, and require physicians to learn unique skills.
Around 200 Reports
Most common among the injuries were bleeding (n = 85), pseudoaneurysm (n = 29), and pulselessness of an extremity (n = 21). The bleeds included 31 documented hematomas, while 28 reports specified location as retroperitoneal. In 45 instances, the injury reports described operators using the device incorrectly, most often failing to perform fluoroscopy to verify VASCADE’s position.
The most-frequent treatments for injuries were intervention (n = 79), manual pressure (n = 35), and blood transfusion (n = 31).
There were 41 reports of device malfunction that included deployment failure, most often the collagen patch being not released or only partially released (n = 43), retraction failure (n = 30), and manufacturer error (n = 10).
“Our analysis of the MAUDE database demonstrates that in contemporary postmarketing practice, physicians should be well trained and educated to use the VASCADE closure device because improper utilization is a common cause of device failure, and complications with the VASCADE device can have profound clinical implications,” the researchers conclude. They stress that, unlike the RESPECT trial, their data set includes patients who might be at risk of higher complications: those with bleeding diathesis, extreme morbid obesity, and previous vascular grafts or surgeries at the target site.
Ultrasound Guidance Key
Amin Al-Ahmad, MD (Texas Cardiac Arrhythmia Institute, St. David's Medical Center, Austin), an investigator who’s studied VASCADE as well as the VASCADE MVP venous closure device, agreed that it’s hard to put the MAUDE reports into context. Beyond not knowing the denominator, it’s also unclear exactly how the device is being used in each instance, he noted. “Is it being used for artery or is it being used for vein? What French? And is it being used on-label or off-label?”
For him, the main use of VASCADE has been for catheter ablation procedures done by venous access. “We do a lot,” Al-Ahmad said. “Our center typically will do about 2,000 to 2,500 ablations per year, and each ablation is typically three to four access sites in the groin.” VASCADE has been their “go-to” device, he added. “We do use other vascular closure devices, but that’s been our majority.”
They’ve witnessed no serious adverse events, he reported. “We’ve seen a few failures here and there, but that’s been expected with any device,” Al-Ahmad noted, adding that in these instances, operators can typically switch to manual compression.
Key to success with VASCADE, Al-Ahmad advised, is ultrasound-guided access, which his group uses in all cases. “[We’re] extremely cautious about it, and then when we close, we confirm with ultrasound. We, in doing that, have been very, very safe,” he said, adding that patient satisfaction is up, bed rest time is shorter, and their groin complication rate is approaching zero. “I think ultrasound’s been a bigger impact than VASCADE, but the two together really make for a good combination.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Case BC, Kumar S, Medranda GA, et al. Contemporary post-marketing adverse events and modes of failure related to VASCADE vascular closure system: the utility of the MAUDE database. Catheter Cardiovasc Interv. 2021;Epub ahead of print.
Disclosures
- Case reports no relevant conflicts of interest.
- Waksman reports serving on the advisory boards of Abbott Vascular, Amgen, Boston Scientific, Cardioset, Cardiovascular Systems Inc, Medtronic, Philips, and Pi-Cardia; consulting for Abbott Vascular, Amgen, Biotronik, Boston Scientific, Cardioset, Cardiovascular Systems Inc, Medtronic, Philips, Pi-Cardia, and Transmural Systems; receiving grant support from AstraZeneca, Biotronik, Boston Scientific, and Chiesi; serving on the speakers bureaus of AstraZeneca and Chiesi; and being an investor in MedAlliance and Transmural Systems.
- Al-Ahmad reports receiving honoraria for participating in educational programs and consulting related to VASCADE.




Comments