Women Have Higher Risk of TAVR-Related Pericardial Complications
The study helps identify at-risk patient populations, which is important as TAVR moves into lower-risk cohorts, an expert says.
Women and patients with a history of coagulopathy have a heightened risk of significant pericardial complications during TAVR, new data show.
For procedures performed in the United States between 2012 and 2014, the likelihood of developing cardiac tamponade, pericardiocentesis, or pericardial window was 2.29-fold greater in women and 1.60-fold greater in patients with coagulopathy, according to lead author Gbolahan Ogunbayo, MD (University of Kentucky Medical Center, Lexington), and colleagues.
On the flip side, patients who had previously undergone CABG or who already had a cardiac implantable electronic device (CEID) in place were less likely to develop significant pericardial complications during TAVR, the investigators report in a research letter published online April 23, 2019, ahead of print in the American Journal of Cardiology.
“For practical purposes, those patients that we know have the higher risk become an important cohort of patients that we need to take extra care on,” Ogunbayo told TCTMD. “Especially when we’re deploying these valves and when we try and put in our temporary pacemakers, [we know] just to be a little bit more cautious.”
He pointed out that patients who developed pericardial complications had a substantially greater risk of dying in the hospital—24.7% vs 3.3% (OR 4.91; 95% CI 2.56-9.43). “This makes it even more imperative to be more mindful of this complication in the at-risk groups we identified,” he said.
Commenting for TCTMD, Chandan Devireddy, MD (Emory University, Atlanta, GA), said, “It is good to know of more vulnerable populations that might be at risk of pericardial complications. It can identify certain types of patients moving forward [for whom] we should have a heightened sense of awareness, especially as we venture into a new low-risk era where we should really aim to drop the risk of pericardial complications far lower than 1%.”
Groups Most at Risk
Ogunbayo said that even though pericardial complications—such as large pericardial effusion and cardiac tamponade—are known problems that can occur with TAVR, there has not been much known about who is most at risk.
To find out, he and his colleagues turned to the National Inpatient Sample, examining data on 34,820 patients who underwent TAVR and no other procedures that could have caused pericardial complications between 2012 and 2014.
Overall, significant pericardial complications were recorded in 1.3% of patients, ranging from 1.2% to 1.5% in the 3 years studied. That’s comparable to what has been reported previously, Ogunbayo said.
Devireddy noted that the rate is probably below 1% in the current era—when intermediate- and low-risk patients are undergoing TAVR—and that the rate observed here likely reflects the higher-risk patients that were being treated during the study period.
Multivariable regression analysis revealed that female sex and a history of coagulopathy were positively associated with those complications, whereas a history of CABG or the presence of a CEID were negatively associated.
Both Ogunbayo and Devireddy pointed to the thinner, more vulnerable myocardial walls found in women as a likely explanation for the association between female sex and a greater risk of complications.
Devireddy also noted that underweight or malnourished patients were overrepresented among the patients with significant pericardial complications. So, he said, for patients who are severely underweight, particularly older women, “I think we’d have to have a much higher suspicion to really be as delicate as possible in instrumenting these patients.”
As for why a history of CABG or CEID implantation would be tied to a lower risk, Ogunbayo suggested pericardial inflammation and the development of fibrosis after both procedures could be a possible explanation. But, he said, that should be investigated in future studies, especially as it relates to device implants.
It’s also possible, Devireddy said, that a preexisting CEID is changing how operators approach a case. If a device is already there, “we may not be as aggressive in our placement of these temporary pacer wires because you know that if you lose backup pacing you’ve got something else there to kind of back you up,” he said, adding, however, that that is purely hypothesis-generating.
Ogunbayo said his group has plans to investigate these issues further using data from the Society of Thoracic Surgeons/American College of Cardiology TVT Registry, which will provide more granular information, particularly regarding comparisons between the different types of TAVR valves.
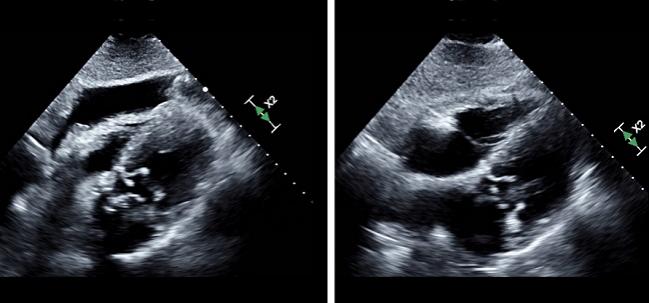
Photo Credit: Bennet George, MD, and Naoki Misumida, MD.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Ogunbayo GO, Misumida N, Goodwin E, et al. Characteristics, outcomes and predictors of significant pericardial complications in patients undergoing transcatheter aortic valve implantation (TAVI). Am J Cardiol. 2019;Epub ahead of print.
Disclosures
- Ogunbayo reports no relevant conflicts of interest.
- Devireddy reports that his institution receives research funding from Medtronic and Edwards Lifesciences and that he serves on data safety monitoring boards for Medtronic.


Comments