Acute MI More Common After TAVI vs SAVR, Real-World Data Suggest
The rate was “very low” at 180 days, says Josep Rodés-Cabau, but operators should increasingly be prepared for these cases.

(UPDATED) Acute MI, while rare at a rate of less than 2%, is more common in the 6 months after transcatheter versus surgical aortic valve replacement, US data indicate. What’s more, a sizeable portion of patients experiencing this adverse event fail to receive an invasive strategy, putting them at higher risk of dying in the hospital.
This stands in contrast to the results of pivotal RCTs, which showed similar acute MI risks among low-, intermediate-, and high-risk patients irrespective of whether they had TAVI or SAVR, Toshiaki Isogai, MD (Cleveland Clinic, OH), and colleagues note in Catheterization and Cardiovascular Interventions. Moreover, they say, the numbers of acute MIs in these trials are too small to draw conclusions about which patients are most at risk and their prognosis thereafter.
Isogai told TCTMD it came as a “surprise that a substantial percentage of patients in both post-AVR groups (particularly after TAVR) did not receive an invasive strategy, despite seemingly better outcomes with [that approach].” The researchers call for a “prospective multicenter study that collects detailed information on clinical course and treatment decision” in order to better understand the phenomenon.
Other observational analyses have shown that TAVI patients fare worse than the general population when they experience acute coronary syndromes or undergo primary PCI for STEMI. Josep Rodés-Cabau, MD, PhD (Quebec Heart and Lung Institute, Laval University, Canada), who led both of these studies, told TCTMD that the new report is relevant to today’s practice despite being based on procedures performed between 2012 and 2017.
For him, these data confirm “the coronary issues after the TAVR procedure,” Rodés-Cabau said. “The originality of this article is that it compares it to the SAVR cohort.” The acute MI rate after TAVI, though “a bit higher compared with SAVR,” is still “very low,” had added.
With the shift toward lower-risk patients following the PARTNER 3 and Evolut Low-Risk trials, “it’s true the clinical profile has changed,” he said, “but the devices that we were using in 2017 are quite similar to those that we are using nowadays, [with] some differences, minor differences.”
Additionally, Isogai observed, while patients at lower surgical risk may have a different risk of acute MI, “the majority of AVR recipients continue to be elderly patients at intermediate or higher surgical risk.” As such, he said in an email, “we believe our findings reflect the current status of AMI risk following TAVR or SAVR.
Nationwide Readmission Database: 2012-2017
Isogai and colleagues, with senior author Samir R. Kapadia, MD (Cleveland Clinic), used the Nationwide Readmission Database to identify 140,285 patients in the United States who were followed for at least 180 days after their aortic valve replacement between 2012 and 2017. Among them, 2,659 were admitted to the hospital for acute MI during follow-up, at an incidence of 1.59% post-TAVI and 0.72% post-SAVR (P< 0.001). TAVI patients with prior CABG were slightly more likely to have an acute MI than were those lacking a CABG history. In the SAVR group, patients had a higher risk of acute MI if they underwent concomitant CABG than if they did not.
Patients in the TAVI group who had an acute MI tended to be older and to have more comorbidities, and were more apt to have NSTEMI (86.6% vs 78.0%; P < 0.001). Overall, they also were less likely to be treated with an invasive strategy involving angiography and/or revascularization compared with the post-SAVR patients (25.6% vs 38.3%; P < 0.001). PCI specifically also was less common post-TAVI (14.0% vs 19.8%; P < 0.001), though in the STEMI group about 40% of patients, no matter their AVR type, received PCI.
Propensity-score matching was performed to balance patient characteristics, after which in-hospital mortality was similar but high for both TAVI and SAVR (14.7% vs 16.1%; P= 0.531). For patients with STEMI, in-hospital mortality reached 38.8% and 29.2%, respectively (P = 0.153).
On multivariable analysis, patients with STEMI, prior PCI, and dyslipidemia were more likely to receive an invasive strategy for their acute MI. Use of an invasive strategy was linked to lower mortality both after TAVI (OR 0.40; 95% CI 0.24-0.66) and after SAVR (OR 0.60; 95% CI 0.41-0.88).
The researchers offer some ideas as to why these observational results diverge from those of RCTs, showing more acute MI for TAVI. “In the pivotal randomized trials, patients with CAD were carefully selected following revascularization or with clear strategies for management, whereas this analysis reflects real-world experience where many patients with CAD may not have undergone prior revascularization, particularly in the TAVR group,” they write, adding that more research should be done to tease out predictors of acute MI after aortic valve replacement.
Rodés-Cabau also drew attention to the lack of invasive treatment, with fewer than half of STEMI patients undergoing PCI. This decision may be valid, he acknowledged. “Many of these patients are really frail, etc.” It stands to reason, however, that “if you have decided to do a TAVR procedure, it seems that if a patient has an MI within a month following this procedure, you should do everything,” Rodés-Cabau said, stressing the need for careful evaluation when AVR patients return with an acute MI. “I think that there is room definitely for improvement, and for more research projects in this particular field.”
One thing to take into account is that these acute MI patients may present to hospitals with no TAVI experience, where physicians may be less familiar with the unique aspects of post-TAVI PCI, Rodés-Cabau observed.
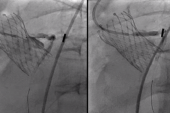
Educational programs are needed to ensure operators have the right skills, “because these patients will be more and more frequent. And we have to deal with these potential difficulties or challenges related to the fact that the patient has a valve prostheses that many times covers or extends beyond the coronary ostia,” he noted. These features in general don’t present a big problem, said Rodés-Cabau, but can do so for clinicians not accustomed to seeing them.
Isogai pointed out that optimal management of CAD among AVR recipients, especially when it comes to TAVI, is still under discussion. Randomized controlled trials including COMPLETE TAVR, CT-CA, FORTUNA, TCW, FAITAVI, ACTIVATION, and NOTION-3 will add to the knowledge base, he predicted, as will observational studies tracing how coronary status before AVR is linked to acute MI after the procedure.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Isogai T, Saad AM, Ahuja KR, et al. Incidence, treatment, and outcomes of acute myocardial infarction following transcatheter or surgical aortic valve replacement. Catheter Cardiovasc Interv. 2021;Epub ahead of print.
Disclosures
- Isogai and Kapadia report no relevant conflicts of interest.
- Rodés-Cabau has received institutional research grants from Edwards Lifesciences, Medtronic, and Boston Scientific; and holds the Research Chair “Fondation Famille Jacques Larivière” for the Development of Structural Heart Disease Interventions.




Comments