‘Aggressive’ OCT Strategy for Stent Sizing Noninferior to IVUS: iSIGHT
The message isn’t to pit the two methods against each other, says the lead investigator. “Just use intravascular imaging.”

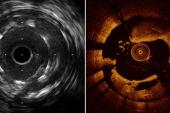
Photo Credit: Prati F. When IVUS-OCT Guidance is a Need: Highly Calcified Lesions and ACS. Presented at TCT 2019. September 26, 2019.
A three-way comparison of PCI guidance confirms that, when sizing is based on the external-elastic membrane (EEM), optical coherence tomography achieves stent expansion that’s noninferior to what’s seen with intravascular ultrasound and superior to angiography.
The iSIGHT study, published in Circulation: Cardiovascular Interventions, involved detailed algorithms for each modality in order to draw clear comparisons, lead author Daniel Chamié, MD, PhD (Dante Pazzanese Institute of Cardiology, São Paulo, Brazil), told TCTMD. It was designed in late 2014 around the same time as the ILUMIEN III trial; both employed an EEM-based strategy for OCT in order to help minimize stent undersizing, but only iSIGHT specified instructions for how to optimize PCI guidance by IVUS and angiography.
At the time, IVUS was thought to be better than OCT, said Chamié. Yet at his hospital, where they used the EEM-based strategy, “our perception as clinicians was that OCT was not inferior—maybe it’s not superior, but definitely it’s not inferior. We get the same clinical outcomes in our practice. That’s what motivated us to do iSIGHT.”
The notion that the EEM approach to OCT improves stent sizing is no longer novel today, following the results from ILUMIEN III and OPINION in the ensuing years, Chamié acknowledged. What’s specific to iSIGHT, he added, is that its approach to stent sizing is “more aggressive” yet still safe, and perhaps especially useful in more-complex cases.
Ziad Ali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), who led ILUMIEN III, also highlighted how OCT’s reputation has shifted as techniques evolved.
“When OCT was first introduced, the method of treatment was a lumen-guided stent sizing,” he commented to TCTMD. “So obviously, if you do [this] for OCT but you do membrane-guided [sizing] for IVUS, you’re comparing apples and oranges and the IVUS always ends up to be bigger. And there’s no question that for arteries, bigger is better—the more lanes you have on a highway, the less likely you are to get traffic jams.”
EEM-based OCT is now “operator standard,” said Ali. Data from iSIGHT add “further weight to the concept that there’s improved stent expansion” with EEM-based OCT, with the possibility that better expansion underlies improved clinical outcomes.
Chamié said that the message is not to pit IVUS and OCT against each other. “Just use intravascular imaging,” he emphasized. The choice comes down to operator preference, ability, training, and level of comfort with one versus the other. What’s more, as noted by Ali, iSIGHT demonstrates that the addition of imaging doesn’t have to substantially increase contrast volume or procedural time for PCI.
The iSIGHT Trial
iSIGHT enrolled 151 patients (156 lesions), randomizing them to undergo PCI guided by OCT, IVUS, or angiography. For both types of intravascular imaging, an EEM-based strategy was used.
Chamié elaborated on what makes the iSIGHT approach unique. To quantify stent diameter by OCT, the ILUMIEN III protocol measured the proximal and distal reference mean EEM then used the smaller of these two values and rounded down to the nearest 0.25 mm. By contrast, for both IVUS and OCT, in iSIGHT “when the EEM was visible in ≥ 180° of the vessel circumference, the reference was sized to the mean EEM diameter. Otherwise, the largest lumen diameter was used,” the paper notes, advising that “lipid-rich plaques should be avoided in the landing zones to minimize the risks of edge dissection or periprocedural MI.”
iSIGHT’s primary endpoint was noninferiority of stent expansion (defined as minimum stent area divided by the average lumen area of the distal and proximal references) measured by post-PCI OCT versus IVUS.
OCT proved noninferior to IVUS, with a mean stent expansion of 98.01% versus 91.69% (P for noninferiority < 0.001). Compared with angiographic guidance, which had a mean stent expansion of 90.53%, OCT was significantly better (P = 0.041). IVUS and angiography performed comparably. The prevalence of lesions with stent expansion ≥ 90% was higher with OCT guidance (74.5%) than with angiography (50.9%) or IVUS (49.0%).
All three methods were equally safe, with no differences in stent edge dissection or periprocedural complications among the groups. By a median of 2.5 years, MACE rates, too, were similar.
How to Encourage Intravascular Imaging?
Ali drew attention to the mean contrast volumes seen in iSIGHT, which came in at 94 mL for OCT, 82 mL for IVUS, and 72 mL for angiography. “Operators were able to use OCT to perform PCI with a really small amount of contrast. Their mean contrast use for the entire procedure was less than 100 mL and in ILUMIEN III it was 222,” he said, attributing this to the fact that ILUMIEN III mandated multiple OCT runs. “But this is an impressive number, so I’m very happy with that.”
Moreover, mean procedure times were approximately 59 minutes with OCT, 58 minutes with IVUS, and 51 minutes with angiography, he pointed out. “[This] shows that you can do imaging-guided PCI with about 8 minutes of additional time and that’s really impressive and profound—that’s a big deal. One of the main reasons that people don’t like to use these things is because they say it takes to long.”
Chamié said their center is attuned, regardless of whether intravascular imaging is being done, to making sure that contrast is used efficiently. “We only take OCT shots in key moments of the procedure when we were already about to take an angio, . . . so the amount that I’m going to add [just for] OCT is much less,” he explained. After stenting, postdilatation, and good angiographic results, Chamié then adds one contrast injection for the OCT, with the catheter well-engaged and coaxial to the vessel. They also do manual injections rather than powered, he said. “You can really control more the amount of contrast you’re giving” and, with experience, know when it’s possible to stop injecting.
Looking ahead, what Chamié would like to see is a large, prospective RCT wherein the angiographic protocol is as optimized as that of OCT and the population includes more-complex anatomies like long lesions and calcified vessels, among others. “If we did everything [as best] we could by angiography,” he said, “like we did in iSIGHT, getting 90% expansion on average, will intravascular imaging add any benefit in terms of clinical endpoints?”
Inclusion criteria of the ongoing ILUMIEN IV trial fit the bill for complexity, he said, and may be able to tease out clinical benefit. With planned follow-up of 2 years, the trial is powered to detect not only an imaging outcome but also target vessel failure (cardiac death, target-vessel MI, or ischemia-driven TLR).
Ali reported to TCTMD that ILUMIEN IV completed enrollment in December 2020.
Akiko Maehara, MD (Cardiovascular Research Foundation and NewYork-Presbyterian/Columbia University Irving Medical Center), writing in an accompanying editorial, agrees that iSIGHT’s algorithms may well increase stent expansion and do it safely.
More broadly, she notes, “we have learned that intravascular imaging improves PCI outcomes over angiography guidance. Whether one should use IVUS or OCT is not a question anymore; however, there is still the challenge of getting the operator who does not use either method to start using one for stent optimization effectively.”
Guideline endorsement and reimbursement are two determinants that could improve adoption, she says, adding that these may come on the heels of results from ILUMIEN IV as well as the OCT-focused OCTOBER trial and IVUS-focused IMPROVE trial. Having standard algorithms might move things along, as could “education along with improvement of imaging software to simplify and facilitate quick and accurate image interpretation,” she suggests.
Note: Maehara, Ali, and senior study author Alexandre Abizaid, MD, PhD, are faculty members of the Cardiovascular Research Foundation, the publisher of TCTMD.
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Chamié D, Costa JR Jr, Damiani LP, et al. Optical coherence tomography versus intravascular ultrasound and angiography to guide percutaneous coronary interventions: the iSIGHT randomized trial. Circ Cardiovasc Interv. 2021;14:e009452.
Maehara A. Optical coherence tomography versus intravascular ultrasound versus angiography, once again. Circ Cardiovasc Interv. 2021;14:e010593.
Disclosures
- Chamié reports no relevant disclosures.
- Maehara reports receiving research grants from and consulting for Boston Scientific and Abbott Vascular.
- Ali reports holding grant support from Abbott Vascular and serving as an advisor to Boston Scientific.




Comments