COVID-19: TCTMD’s Dispatch for April Week 2
We’re curating a list of COVID-19 research and other useful content, and updating it regularly.

Since March 2020, TCTMD reporter Todd Neale has been writing up breaking news and peer-reviewed research related to COVID-19 every weekday. In July 2021, we transitioned to Mondays, Wednesdays, and Fridays. If you have something to share, tell us. All of our COVID-19 coverage can be found on our COVID-19 Hub.
April 14, 2022
The United States yesterday renewed its COVID-19 public health emergency, first declared in January 2020, allowing for citizens to continue to receive free tests, vaccines, and treatments for at least another 3 months. “The Department of Health and Human Services HHS in a statement said it was extending the public health emergency and that it will give states 60 days’ notice prior to termination or expiration,” Reuters reports.
 Pfizer/BioNTech’s phase II/III clinical trial evaluating the safety, tolerability, and immunogenicity of a 10-µg booster dose of its COVID-19 vaccine in healthy children ages 5 through 11 years shows a 36-fold increase in neutralizing antibodies against Omicron and a sixfold increase against the wild-type strain, the companies announced today. The study was conducted in 140 kids in this age group. “Companies plan to submit these data to US Food and Drug Administration in the coming days with additional submissions to other regulatory agencies worldwide to follow,” a press release states.
Pfizer/BioNTech’s phase II/III clinical trial evaluating the safety, tolerability, and immunogenicity of a 10-µg booster dose of its COVID-19 vaccine in healthy children ages 5 through 11 years shows a 36-fold increase in neutralizing antibodies against Omicron and a sixfold increase against the wild-type strain, the companies announced today. The study was conducted in 140 kids in this age group. “Companies plan to submit these data to US Food and Drug Administration in the coming days with additional submissions to other regulatory agencies worldwide to follow,” a press release states.
British Prime Minister Boris Johnson has received multiple fines for breaking his own COVID-19 pandemic laws but refuses to say whether he will resign from his post over the penalties. “Johnson is likely to face a barrage of questions when he makes a statement to the Commons next week, including over the suggestion he may have misled parliament by assuring MPs on 1 December that ‘all guidance was followed completely in No 10,’” the Guardian reports.
New York health authorities say two new sub-substrains of the Omicron variant are circulating in the city that are even more contagious than the Omicron BA.2 strain, which was already more contagious than Omicron, which was itself more contagious than the original wildtype SARS-CoV-2 virus. BA.2 already accounts for 80.6% of COVID-19 infections in New York, and these “subvariants have been estimated to have a 23-27% growth advantage above the original BA.2 variant,” a press release notes, adding that while the strain is new, the tools to fight it—vaccines, testing, masking, vigilance for symptoms—are not.
 In many parts of the world, people are getting used to seeing “naked” faces again, unencumbered by masks. In JAMA, a movement-disorders neurologist, accustomed to assessing faces for signs and symptoms of illness like Parkinson’s, describes what it’s been like to once again see full facial expressions. “I find myself taken aback by the intimacy of seeing their faces,” writes Emily Anne Ferenczi, BMBCh, PhD, “a uniquely pandemic-era experience.”
In many parts of the world, people are getting used to seeing “naked” faces again, unencumbered by masks. In JAMA, a movement-disorders neurologist, accustomed to assessing faces for signs and symptoms of illness like Parkinson’s, describes what it’s been like to once again see full facial expressions. “I find myself taken aback by the intimacy of seeing their faces,” writes Emily Anne Ferenczi, BMBCh, PhD, “a uniquely pandemic-era experience.”
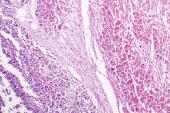
Similar to the increased risk of systemic vascular damage associated with COVID-19 in other organ systems, patients may face an increased risk of retinal vein occlusion in the 6 months after their infection, a paper in JAMA Ophthalmology warns.
A large, prospective, longitudinal observational study using data from the ZOE COVID app to compare symptoms when Delta was prevalent, as compared with symptoms during Omicron’s reign, confirms that loss of smell is significantly more common with Delta, while sore throat was more frequent with Omicron. Also: hospitalizations were significantly lower during the Omicron surge. “Our data indicate a shorter period of illness and potentially of infectiousness which should impact work-health policies and public health advice,” investigators write in the Lancet.
Data out of Israel, published in the New England Journal of Medicine, are once again offering other countries a glimpse of the benefits derived from swift and sweeping vaccination rollouts, this time the results of its nationwide fourth-dose campaign in people aged 60 and older, or with compromised immunity. In a matched-pair analysis, a fourth dose versus a third dose given at least 4 months earlier cut severe cases, hospitalizations, and deaths. As an editorial notes, the US Food and Drug Administration and Centers for Disease Control and Prevention considered these numbers when they made their recommendations for boosters in people 65 and older. What’s needed now, they write, is more clarity on the value in younger, healthier adults, not to mention some better education campaigns by health authorities as to what constitutes full vaccination and what kind of protection that affords.
 Also in the New England Journal of Medicine, Robert Bazell, CPhil, Howard Koh, MD, MPH, and Barry R. Bloom, PhD, make the case that the “Tobacco Wars” of the late 20th century can offer some clues in the fight against COVID-19 vaccine misinformation. “In the case of tobacco, preventable deaths were fueled by an industry that influenced millions of people with messages suggesting that using its products was glamorous and normal. Nearly half of US adults smoked cigarettes in the 1960s. The current rate of about 12.5% reflects decades of multifaceted public health efforts to deglamorize and denormalize tobacco use and make it less socially acceptable.”
Also in the New England Journal of Medicine, Robert Bazell, CPhil, Howard Koh, MD, MPH, and Barry R. Bloom, PhD, make the case that the “Tobacco Wars” of the late 20th century can offer some clues in the fight against COVID-19 vaccine misinformation. “In the case of tobacco, preventable deaths were fueled by an industry that influenced millions of people with messages suggesting that using its products was glamorous and normal. Nearly half of US adults smoked cigarettes in the 1960s. The current rate of about 12.5% reflects decades of multifaceted public health efforts to deglamorize and denormalize tobacco use and make it less socially acceptable.”
April 11, 2022
On Monday, Philadelphia became the first major US city to reinstate mask mandates, while some American colleges and universities are also bringing back mandatory masking, the New York Times reports. For the first time since mid-January 2022, COVID-19 cases are up nationwide in the United States, according to the Centers for Disease Control and Prevention (CDC) weekly tracker. In other US numbers summarized by Becker’s Hospital Review, the 7-day average for vaccines administered was up by 98% over last week’s figures. Just over 77% of people in the United States (255.9 million) have received at least one vaccine dose, but only half of the population—as of March 30—had gotten at least one booster.
 Writing in the Lancet, researchers propose a “novel approach to estimating past SARS-CoV-2 daily infections, cumulative infections, and the proportion of the population infected, for 190 countries and territories from the start of the pandemic to Nov 14, 2021.” By combining a range of data sources and correcting for biases, they estimate that the world has seen 3.8 billion infections and reinfections as of November 14, 2021, meaning that SARS-CoV-2 has infected nearly 44% of the world’s population. And that, they note, was before the advent of Omicron: “Cumulative infections for COVID-19 through to March 2022, might be nearly double what occurred through Nov 14, 2021.”
Writing in the Lancet, researchers propose a “novel approach to estimating past SARS-CoV-2 daily infections, cumulative infections, and the proportion of the population infected, for 190 countries and territories from the start of the pandemic to Nov 14, 2021.” By combining a range of data sources and correcting for biases, they estimate that the world has seen 3.8 billion infections and reinfections as of November 14, 2021, meaning that SARS-CoV-2 has infected nearly 44% of the world’s population. And that, they note, was before the advent of Omicron: “Cumulative infections for COVID-19 through to March 2022, might be nearly double what occurred through Nov 14, 2021.”
Back in June 2020, the RECOVERY trial results made it clear that corticosteroids are useful in severely ill hospitalized patients, but not in patients who don’t require supplemental oxygen. But as a research letter in JAMA makes clear, more than one in ten outpatients diagnosed with COVID-19 are still prescribed systemic corticosteroids. What’s more, steroid use appeared to increase over time—from 2.2% in April 2020 to 21.1% in August 2021 among Medicare patients and from 2.2% in April 2020 to 13.8% in July 2021 among patients included in the Sentinel database. “Given the increasing use of corticosteroids through August 2021, the potential safety signal, and the lack of efficacy data in patients with mild-to-moderate COVID-19, it is critical that prescribers consider the [National Institutes of Health] guidelines in the therapeutic management of nonhospitalized patients with COVID-19,” researchers conclude.
Also in the category of don’t-help-but-still-prescribed are antibiotics, which according to a separate research letter in JAMA were given to nearly 30% of outpatient COVID-19 patients early on in the pandemic. Antibiotic prescribing started at 17.5% in May 2020, then reached 33.3% by October 2020. Azithromycin was the antibiotic of choice in half of the instances, and emergency departments were most often the source of the prescription. The authors’ blunt reminder: “Antibiotics are ineffective treatment for viral syndromes, including COVID-19.”
A second paper in as many weeks is confirming that Food and Drug Administration (FDA) approval of the Pfizer/BioNTech vaccine did little to boost uptake by people who’d declared themselves to be hesitant to get vaccinated while the emergency use authorization was in place. “Unvaccinated Americans who said they were awaiting full FDA approval before being vaccinated may have been providing a socially desirable response, or they may subsequently have ‘moved the goalpost’ for the level of vaccine safety and efficacy data needed before vaccinating after FDA approval occurred,” authors write in JAMA Internal Medicine.
Meanwhile, a Nature news story looks into the lasting immunity conferred by a full course of vaccination, even on top of prior infection, drawing on three separate studies that showed consistent findings of an additive effect. All were done prior to the emergence of Omicron, “but if the findings hold up, they could inform vaccination schemes and vaccine passports, which some countries require for entry to places such as restaurants,” writes Saima May Sidik. “The work also counters high-profile claims that people who have had COVID-19 don’t benefit from vaccination.”
 As many parts of the world embark on plans to “live with COVID-19” as an endemic disease—even as new infections are breaking records—an editorial in Lancet: Diabetes and Endocrinology is calling out the “elephant in the room” amid these proposals. “In a world where the new mantra is to learn to live with COVID-19, long COVID cannot be ignored. Any strategy to learn to live with COVID-19 must also aim for a fair, thriving, and healthy postpandemic world—that is what return to normalcy should look like,” its authors urge.
As many parts of the world embark on plans to “live with COVID-19” as an endemic disease—even as new infections are breaking records—an editorial in Lancet: Diabetes and Endocrinology is calling out the “elephant in the room” amid these proposals. “In a world where the new mantra is to learn to live with COVID-19, long COVID cannot be ignored. Any strategy to learn to live with COVID-19 must also aim for a fair, thriving, and healthy postpandemic world—that is what return to normalcy should look like,” its authors urge.
After reviewing case reports and published literature, the Pharmacovigilance Risk Assessment Committee of the European Medicines Agency (EMA) has concluded that there is no plausible link between mRNA vaccines made by Pfizer/BioNTech and Moderna and autoimmune hepatitis (AIH).
Many health professionals—and others—have taken to social media to express their frustration with the burden unvaccinated patients are placing on hospitals, and the risks those pose for others. In a perspective published this week in the New England Journal of Medicine, Amanda Garfinkel, MD, describes the death of one fully vaccinated, immunocompromised patient alongside the survival of an unvaccinated patient who’d received a monoclonal antibody infusion, and how she’s managed the difficult journey from resentment to reconnection.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full Bio



Comments