COVID-19: TCTMD’s Dispatch for May Week 1
We’re curating a list of COVID-19 research and other useful content, and updating it regularly.

Since March 2020, TCTMD reporter Todd Neale has been writing up breaking news and peer-reviewed research related to COVID-19 every weekday. In July 2021, we transitioned to Mondays, Wednesdays, and Fridays. If you have something to share, tell us. All of our COVID-19 coverage can be found on our COVID-19 Hub.
May 5, 2022
Governments around the globe have radically underestimated the number of deaths attributed to COVID-19, a global panel assembled by the World Health Organization has concluded. New York Times coverage of the report gives some examples, noting that excess deaths in Mexico were twice as high as the official government tally, while the true rate was eight times higher than the official count for Pakistan. The WHO analysis includes deaths directly caused by the virus as well as those who died because they couldn’t get access to urgent care for other conditions, including MI. “Overall, roughly 14.9 million more people worldwide died in 2020 and 2021 than would have been expected to in normal times, the experts estimated.”
 The US Food and Drug Administration is warning consumers about fake at-home, over-the-counter tests for COVID-19, launching a website to keep track of counterfeit tests. “The performance of these tests has not been adequately established and the FDA is concerned about the risk of false results when people use these unauthorized tests,” a statement reads.
The US Food and Drug Administration is warning consumers about fake at-home, over-the-counter tests for COVID-19, launching a website to keep track of counterfeit tests. “The performance of these tests has not been adequately established and the FDA is concerned about the risk of false results when people use these unauthorized tests,” a statement reads.
Researchers writing in a Lancet preprint paper have a theory as to why antigen tests seem to be less accurate as the pandemic drags on, saying not only evolving variants but also changing levels of preexisting immunity play a role. “Among hospital employees with symptomatic COVID-19 in Berlin, Germany, from late 2020 to early 2022, rapid antigen test sensitivity decreased over time, from 80% to 67%, despite a 5.6-fold increase in median viral RNA concentrations.”
Final results from the SOLIDARITY study, which randomized more than 14,000 patients hospitalized with COVID-19 to remdesivir (Veklury; Gilead Sciences) or placebo found no significant effect of the agent in preventing in-hospital death among patients already on a ventilator. For unventilated patients, however, the drug appears to have “a small effect against death or progression to ventilation (or both),” trialists report in the Lancet.
 The New England Journal of Medicine this week has phase 3 clinical trial results for two new COVID-19 vaccines, both of which do not require extreme cold-temperature storage. One is a plant-based coronavirus-like particle vaccine the other a receptor-binding domain–dimer–based vaccine, and study results for both were positive, showing significant benefit against confirmed infections, and even better efficacy against severe disease. An accompanying editorial notes that both studies included patients in developing nations, which represent settings where vaccines not requiring special storage and transport would be especially useful. They also were done when different variants were circulating, although they took place before Omicron and its variants became dominant. New vaccines are needed, the authors conclude, adding that the first vaccines that made it to market may not, ultimately, be the best ones down the road.
The New England Journal of Medicine this week has phase 3 clinical trial results for two new COVID-19 vaccines, both of which do not require extreme cold-temperature storage. One is a plant-based coronavirus-like particle vaccine the other a receptor-binding domain–dimer–based vaccine, and study results for both were positive, showing significant benefit against confirmed infections, and even better efficacy against severe disease. An accompanying editorial notes that both studies included patients in developing nations, which represent settings where vaccines not requiring special storage and transport would be especially useful. They also were done when different variants were circulating, although they took place before Omicron and its variants became dominant. New vaccines are needed, the authors conclude, adding that the first vaccines that made it to market may not, ultimately, be the best ones down the road.
“Long COVID” is the term that was collectively coined by patients struggling with a wide range of lasting symptoms after recovering from their initial illness. As an editorial in Lancet Respiratory Medicine points out, experts have not fully gotten behind the terminology and various agencies have evolved their own monikers. With millions of people affected by this condition in different ways, “there is an urgent need for unification of terminology for the sequelae of SARS-CoV-2 infection,” write Daniel Munblit, MD, PhD, and colleagues. “Different terms may be used, but only if they are well defined and help ensure that research is directed towards and translated into interventional trials to improve the outcomes of people with long COVID.”
The Omicron variant has not proved as lethal as Alpha and Delta in long-term care facilities in England, VIVALDI data confirm. “Observed reduced severity of the omicron variant compared with previous variants suggests that the wave of Omicron infections is unlikely to lead to a major surge in severe disease in long-term care facility populations with high levels of vaccine coverage or natural immunity,” authors conclude in the Lancet Healthy Longevity. But ongoing surveillance is warranted, they add, as new variants emerge.
COVID-19 killed 1 million Americans in 2 years and has not yet fallen into a seasonal cadence of infectiousness. But as a STAT story explores, “there are signs that the virus—and our relationship to it—is shifting in subtle ways that make it more like seasonal flu than it was at the start of the pandemic.” It’s more “uniformly infectious,” there are more options for vaccination and treatment, and the strains themselves are “more genetically predictable,” writes Megan Molteni.
Physical masking has helped curb the spread of COVID-19, but physicists checking the fluid dynamics of mask fit say face shape matters, and double-masking may not be the answer to a bad fit. Writing in the Physics of Fluids, investigators caution that double-making with coverings that don’t fit doesn’t actually improve efficacy, and may increase risk by producing a false sense of security.
Investigators writing in PLOS Biology affirm that despite the fact vaccines primarily work by inducing neutralizing antibody responses, “other, less well-understood, immune responses contribute to protection.” These include the Fc receptor, “a cell-surface molecule that recognizes the invariant part of antibodies, and can trigger the destruction of infected cells, and by T-cell responses, complementing the other antibody responses that directly neutralize the virus.” The insights, authors say, help explain why additional doses and boosting help protect against severe disease and death, and may help guide future vaccine development.
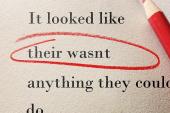
 More timely than ever amid all the rumors, snake oil, and misinformation circulating about COVID-19 and the vaccines approved to fight it, a perspective in NEJM offers support for healthcare workers to address fake medical news on social media.
More timely than ever amid all the rumors, snake oil, and misinformation circulating about COVID-19 and the vaccines approved to fight it, a perspective in NEJM offers support for healthcare workers to address fake medical news on social media.
May 2, 2022
The United States reported “double-digit increases” in both COVID-19 cases and hospitalizations last week, according to US Centers for Disease Control and Prevention data summarized by Becker’s Hospital Review. The 7-day hospital average was up 18.5%, compared to 1 week prior, while case averages were up more than 25%.
 New York has moved its risk level to “medium” (yellow) as COVID-19 cases rise again, a move that could trigger the reintroduction of public health restrictions, the New York Times reports. “The city is now seeing nearly 2,500 new cases per day, a significant jump from about 600 daily cases in early March. The latest rise, fueled by the highly contagious Omicron subvariant known as BA.2, does not rival the first Omicron surge in December and January, but recorded case levels are as high as they were when the Delta variant swept through the city last year.”
New York has moved its risk level to “medium” (yellow) as COVID-19 cases rise again, a move that could trigger the reintroduction of public health restrictions, the New York Times reports. “The city is now seeing nearly 2,500 new cases per day, a significant jump from about 600 daily cases in early March. The latest rise, fueled by the highly contagious Omicron subvariant known as BA.2, does not rival the first Omicron surge in December and January, but recorded case levels are as high as they were when the Delta variant swept through the city last year.”
In China, Beijing has reopened a 1,000-bed “mass isolation center” in the hopes of avoiding a citywide lockdown of the sort that is still being weathered by residents of Shanghai. The hospital was originally built to treat SARS patients in 2003 and was repurposed for COVID-19 in 2020, the Times reports.
“It is time to accept that the presence of SARS-CoV-2, the virus that causes COVID-19, is the new normal,” US Food and Drug Administration leaders write in a viewpoint in JAMA. “It will likely circulate globally for the foreseeable future, taking its place alongside other common respiratory viruses such as influenza.” That likely means getting vaccinated against the latest COVID-19 strains alongside seasonal influenza vaccination, which in turn means annual consideration by the agency of updates to vaccine composition—and an appetite in the public to stay up-to-date with the jabs.
 Seroprevalence data published in Morbidity and Mortality Weekly Report last week indicate that one in four children and adolescents have serologic evidence of previous COVID-19 infection, with one-third becoming newly seropositive since December 2021. In that same period, seroprevalence rates increased from 36.5% to 63.7% in adults aged 18-49 years, from 28.8% to 49.8% among those 50-64 years, and from 19.1% to 33.2% among those 65 and older. “Lower seroprevalence among adults aged ≥ 65 years, who are at greater risk for severe illness from COVID-19, might also be related to the increased use of additional precautions with increasing age,” authors note. Of note, seroprevalence tracked inversely with vaccination status, with full vaccination (as of April 2022) being most common (> 90%) among adults 65 and older.
Seroprevalence data published in Morbidity and Mortality Weekly Report last week indicate that one in four children and adolescents have serologic evidence of previous COVID-19 infection, with one-third becoming newly seropositive since December 2021. In that same period, seroprevalence rates increased from 36.5% to 63.7% in adults aged 18-49 years, from 28.8% to 49.8% among those 50-64 years, and from 19.1% to 33.2% among those 65 and older. “Lower seroprevalence among adults aged ≥ 65 years, who are at greater risk for severe illness from COVID-19, might also be related to the increased use of additional precautions with increasing age,” authors note. Of note, seroprevalence tracked inversely with vaccination status, with full vaccination (as of April 2022) being most common (> 90%) among adults 65 and older.
Two Omicron subvariants, BA.4 and BA.5, are driving the latest COVID-19 surge in South Africa, and are already circulating in the United States. According to Reuters, “the two new sublineages of the Omicron coronavirus variant can dodge antibodies from earlier infection well enough to trigger a new wave, but are far less able to thrive in the blood of people vaccinated against COVID-19.”
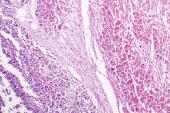
Researchers writing in Nature Communications have uncovered clues as to why such a small minority of children infected with SARS-CoV-2 go on to develop multisystem inflammatory syndrome (MIS-C) or COVID-19 induced acute respiratory distress syndrome (ARDS). The study, using mass spectrometry proteomics, discovered that certain plasma proteins not found in healthy kids are differentially expressed in MIS-C or COVID-19 ARDS and appear to be implicated in the complement activation and coagulation pathways. “This knowledge adds to our understanding of the severe COVID-19 phenotypes in children and suggests pathophysiological mechanisms that could be the subject of specific therapies to try and improve the outcomes for these children,” authors conclude. A story in the Guardian has more.
Also in Nature Communications today: a large, real-world analysis of how the Moderna and Pfizer/BioNTech vaccines hold up over time. The upshot: mRNA-1273 (Moderna) provides slightly more protection against SARS-CoV-2 infection than BNT162b2 (Pfizer/BioNTech), a difference that reaches statistical significance at 90 days with a number needed to vaccinate of 290 or more. “There are no differences in vaccine effectiveness for protection against hospitalization, ICU admission, or death/hospice transfer,” authors conclude.
 Another study, this one from Canada, indicates that the risk of hospitalization and ICU admission for COVID-19 was significantly higher among pregnant women than in a similar population of reproductive age females. Moreover, preterm births were higher among women with SARS-CoV-2, researchers write in JAMA. “During the time period of this analysis, before the Omicron variant, almost all cases of SARS-CoV-2 infection (98.7%) occurred among pregnant persons who had not been previously vaccinated.”
Another study, this one from Canada, indicates that the risk of hospitalization and ICU admission for COVID-19 was significantly higher among pregnant women than in a similar population of reproductive age females. Moreover, preterm births were higher among women with SARS-CoV-2, researchers write in JAMA. “During the time period of this analysis, before the Omicron variant, almost all cases of SARS-CoV-2 infection (98.7%) occurred among pregnant persons who had not been previously vaccinated.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full Bio



Comments