CTO Diagnosed, Now What? European Experts Offer Advice on Revascularization
The consensus paper, which calls for a team approach, is aimed at referring physicians who need to know next steps.

Patients diagnosed with coronary chronic total occlusions (CTOs) can benefit from a team approach to decision-making about revascularization, according to a newly released expert consensus from various subspecialties within the European Society of Cardiology (ESC).
The statement, published this week in EuroIntervention, was developed by the European Association of Percutaneous Cardiovascular Interventions (EAPCI), the European Association of Cardiovascular Imaging (EACVI), and the ESC Working Group on Cardiovascular Surgery.
Alfredo R. Galassi, MD (University of Palermo, Italy), its lead author, pointed out that the current work builds on a 2016 document that had been aimed at the operators deciding on the appropriateness of a CTO PCI. Nearly a decade later, the current paper is informed by a wider multidisciplinary scope of expertise and is a “clinical consensus,” he noted to TCTMD. “We are realizing that nowadays chronic total occlusions are revascularized largely by dedicated operators,” so it’s important to educate not just the people who are doing the procedures but also those who are managing patients in clinical settings.
Aimed specifically at referring physicians, the document offers an algorithm for how to evaluate CTO patients prior to intervention and summarizes current evidence on the revascularization’s clinical effectiveness, with an eye toward the role of optimal medical therapy (OMT).
For these healthcare professionals, said Galassi, it’s important to recognize that they might encounter CTOs in an array of scenarios: in symptomatic patients who have stable angina or ACS with multivessel disease, for instance, or in asymptomatic patients as an incidental finding on noninvasive testing or in conjunction with type 2 MI.
“Clinicians more and more often are exposed to the [reality] that they found a CTO in the patient and they should know what to do in this situation,” he observed.
At experienced CTO centers, success rates are now as high as 85-90% and complication rates no more than 3%, the paper notes. Still, many clinicians may be reluctant to pursue revascularization, thinking that medical therapy may be enough, whereas on the flip side, interventionalists may lean more heavily toward doing a procedure.
In taking a balanced approach, “this document for the first time is assessing the real value of revascularization and indications for revascularization,” Galassi observed.
He specified that, at least based on current evidence, “PCI does not extend life. . . . But in terms of quality of life and in terms of recurrent symptoms that bring you back to the cath lab, this is something that makes a difference. So, the patients who are [going for] PCI are feeling better.”
PCI does not extend life. . . . [But] the patients who are [going for] PCI are feeling better. Alfredo R. Galassi
Emmanouil Brilakis, MD, PhD (Minneapolis Heart Institute, MN), who in 2019 led a global expert consensus document outlining guiding principles for CTO PCI, commented on the new paper for TCTMD. It does a good job at summarizing the existing data and specifying that “symptom improvement is the main reason for doing complex CTO PCI,” he said.
While there’s not a lot of new information here for the operators who routinely do CTO PCI, the document does provide helpful background for referring physicians, as well as common-sense tips, said Brilakis. “There are a lot of misconceptions out in the real world about what CTO PCI is and when it should be used.”
Symptoms as a Starting Point
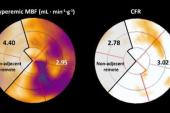
Today, decision-making in CTOs is driven mostly by symptoms, Galassi said, stressing that angina isn’t the only condition to look out for: dyspnea and impaired health status are also relevant. When any of these are present, “usually revascularization is advised if there is normal wall motion,” he explained. “Conversely, when there are symptoms but there is an akinetic or dyskinetic segment, then it’s better to look for viability.” If there is viable myocardium, then revascularization again is advised. “If viability is not found despite symptoms—and this is something very new, probably in light of advancements in medical therapy—optimized medical therapy and follow-up is advisable,” added Galassi.
But if symptoms aren’t an issue, only patients with LV dysfunction paired with significant ischemia and viability might be considered for revascularization in select cases, their algorithm states. The rest will be served best by OMT and follow-up.
The consensus statement also emphasizes a team approach. For non-LAD CTOs, isolated CTO PCI is the natural choice, Galassi noted. But for CTOs in the LAD, in the context of multivessel disease, or in those with a previous CABG, the heart team—with an interventionalist, cardiac surgeon, cardiac imager, and anesthesiologist—should evaluate the various options in light of factors such as CTO complexity, local PCI expertise, surgical risk, availability of arterial or venous conduits, concomitant valvular heart disease, bleeding risk, and the presence of porcelain aorta or aortic arch atherosclerosis.
There are a lot of misconceptions out in the real world about what CTO PCI is and when it should be used. Emmanouil Brilakis
Galassi highlighted two papers from EUROCTO, the first randomized trial of CTO PCI, that support their recommendations. The main results, as reported by TCTMD in 2017, showed fewer physical limitations, better quality of life, and less frequent angina with PCI versus OMT at 1 year. Then, 3-year follow-up published in EuroIntervention in 2023, confirmed that PCI was safe over the long term (with similar rates of CV death and nonfatal MI) and showed a lower MACE rate with PCI, though the difference was due mainly to ischemia-driven revascularization.
Whether or not CTO revascularization does in fact reduce hard outcomes isn’t yet definitive, he said. There could be some subgroups particularly apt to benefit from intervention, something that needs to be clarified in randomized trials, added Galassi. “Probably future studies where patient selection might be more accurate will tell us the difference in outcome,” and extended follow-up is needed to examine the signal of benefit seen in some registry studies.
Brilakis said that ISCHEMIA-CTO, an ongoing 1,500-patient randomized trial, will likely provide some answers. That study isn’t set to end until 2028, he noted, “so it will probably be a while before this is completely done.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Galassi AR, Vadalà G, Werner GS, et al. Evaluation and management of patients with coronary chronic total occlusions considered for revascularisation. A clinical consensus statement of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) of the ESC, the European Association of Cardiovascular Imaging (EACVI) of the ESC, and the ESC Working Group on Cardiovascular Surgery. EuroIntervention. 2024;20:e174-e184.
Disclosures
- Galassi reports no relevant conflicts of interest.



Comments