Long-term CTO Data Raise Questions Over Primary Goals of Care
Two new papers highlight the need for optimal revascularization, but debate will go on over angina relief versus harder outcomes.

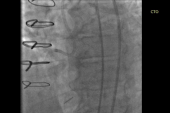
There is no difference in 10-year mortality between patients whose total occlusion lesions had been successfully reopened by PCI or CABG, as compared with those in whom revascularization or recanalization was unsuccessful, according to a new analysis. Another study published the same week emphasizes that physicians should aim for complete and optimal revascularization when performing PCI for chronic total occlusion (CTO) lesions, but also that if the effort fails, they should abort the procedure rather than settle for sub-par outcomes.
Taken together, the two studies make the case for being judicious in selecting the best CTOs for intervention, with a focus on reperfusing both the occluded vessel as well as any side branches, while using the best techniques and technology to improve the chances for success.
CTO interventions are a challenging, niche field where innovation has rapidly progressed despite gaps in data. There is no large randomized controlled trial evidence to show that successfully treating these lesions improves hard outcomes, but many proponents of the procedure argue that a key aim is improving angina symptoms and quality of life. Questions remain also regarding the clinical and financial costs for attempting a CTO intervention but failing to achieve the desired results.
“At a minimum the symptom benefit is there and . . . there may indeed be benefit in harder outcomes,” said Kalra.
Additionally, he noted, findings from these older data sets—both papers focus on patients treated about a decade ago—suggest “that revascularizing lesions using the old way was not good enough; it's not that it didn't work. [They also suggest] that the more you revascularize the better your outcomes are going to be and the more you revascularize the more comfortable your patients are going to be. That's important.”
Also commenting on both studies for TCTMD, Sunil Rao, MD (Duke Clinical Research Institute, Durham, NC), said they indicate how “our systems for collecting data around PCI are just completely outdated.
“We have to move beyond this to actually show that what we're doing and what we're offering to patients is something that's safe and beneficial,” he stressed. “What would be ideal is if these data collection methods or these registries served as a platform for doing the randomized trial, so that we can add to the evidence base.”
Impact of CTO Interventions
In the first study, published in the February 9, 2021, issue of the Journal of the American College of Cardiology, Hideyuki Kawashima, MD (University of Amsterdam, the Netherlands), and colleagues broach the question of whether successful CTO interventions actually improve hard outcomes. To this end, they looked at 10-year results for 460 patients with at least one total occlusion who participated in the SYNTAXES study and were randomized to PCI or CABG with the aim of comparing outcomes based on whether the occlusion had been successfully reopened.
They found that all-cause mortality at 10 years was similar between those who underwent successful intervention and those who did not, regardless of whether the lesions had been tackled with PCI or CABG.
10-Year Mortality by Revascularization/Recanalization Success
|
|
Successful |
Unsuccessful |
Adjusted HR |
95% CI |
|
PCI |
29.9% |
29.4% |
0.99 |
0.47-2.08 |
|
CABG |
28.0% |
21.4% |
0.66 |
0.28-1.53 |
Moreover, the location of the total occlusion didn’t seem to affect mortality. When they looked at total occlusions in only the left main and/or left anterior descending artery, there were no differences in death based on recanalization/revascularization success (34.5% vs 26.9%; adjusted HR 0.90; 95% CI 0.31-2.56).
Of note, however, success rates were lower with PCI than with CABG (43.5% vs 60.5%; P < 0.001). “This . . . may be due to the complexity of the total-occlusion lesion or the unavailability of contemporary devices and techniques during the SYNTAX trial enrollment (2005 to 2007),” the authors note. The more-contemporary trial, SYNTAX II, enrolled patients a decade later and achieved recanalization rates as high as 87%, they point out.
The lack of survival benefit with successful intervention is in keeping with other studies including EUROCTO and DECISION-CTO, they conclude. The former showed gains in quality of life, whereas the latter did not—proponents of CTO procedures have long argued that angina relief should be the chief reason for intervening on these lesions.
“The present study might support contemporary practice among high-volume CTO PCI centers where recanalization is primarily offered to patients for the management of angina refractory to medical therapy when myocardial viability is confirmed,” Kawashima and colleagues write.
‘Mixed Bag’
In an editorial accompanying the Kawashima paper, Jeffrey W. Moses, MD, and Megha Prasad, MD (both Columbia University Irving Medical Center, New York, NY), cite several challenges with the data set including the study’s “mixed bag of occlusions.” As they note, “the analysis fails to differentiate main branch occlusions from distal and/or side branch occlusions, and chronic occlusions from recent occlusions, thus essentially treating all occlusions equally.”
Neither the anatomic location nor the age of the total occlusions was accounted for, which doesn’t allow for differentiation of chronic lesions and recent missed MIs, Moses and Prasad say.
Because of all these limitations, they say there’s a continued role for CTO PCI. Still, “careful weight must be given to the extent of myocardium at risk, the chances of uncomplicated success, along with the treatment objectives for individual patients. Unlike humans, all CTOs are not created equal,” Moses and Prasad conclude.
Doing It Right
For the second analysis, published in the February 8, 2021, issue of JACC: Cardiovascular Interventions, Changdong Guan, MSc (Fu Wai Hospital, Beijing, China), et al looked at 5-year outcomes of 2,659 CTO patients treated at their institution between 2010 and 2013. The cohort was divided into three groups:
- Optimal recanalization (58.7%): reperfusion of the occluded vessel and side branches (if any) with TIMI flow grade 3
- Suboptimal recanalization (15.0%): major side branches still occluded, final TIMI flow 1/ 2, or residual diameter stenosis > 30%
- Procedural failure (26.3%): failure to cross a lesion with a balloon angioplasty catheter
At 5 years, successful CTO recanalization was not associated with a reduced risk of the composite endpoint of cardiac death or MI, compared with failure, but this endpoint was highest in those with suboptimal outcomes (10.1%) compared with those who had optimal recanalization (6.5%; P = 0.02) and compared with patients whose procedures failed (6.3%; P = 0.03). Similar patterns were seen for MI alone, while ischemia-driven TVR and target lesion revascularization were both higher for the suboptimal recanalization cohort compared with those receiving optimal results.
Side branch occlusion was a major reason for MI events in the suboptimal group, consistent with prior reports,” Guan and colleagues note.
Unsuccessful procedures carry real costs, they add. Suboptimal recanalizations proved to be more expensive than optimal procedures ($14,940 vs $11,905) and failures ($8,256; P < 0.0001 for both).
“Considering the ‘time economy’ of CTO PCI, which is a major factor dissuading physicians in real clinical settings, it is necessary to systematically review cases and conduct sufficient preprocedural planning before CTO PCI using various prediction tools such as the J-CTO score or coronary computed tomography angiography,” they advise. “Reducing complications, especially significant side branch occlusion, could decrease costs and also provide better clinical outcomes.”
The Guan paper “shows us that, as operators, we should not accept suboptimal results, especially if a side branch is lost,” write Luiz F. Ybarra, MD, PhD, MBA, and Rodrigo Bagur, MD, PhD (both Western University, London, Canada), in an accompanying editorial.
“Considering the growing evidence on symptom alleviation and quality-of-life improvement, coupled with the current procedural safety and success, CTO PCI numbers are expected to rise even further,” they conclude. “Despite its limitations, the study by Guan et al provides evidence that, in the absence of optimal CTO recanalization, the ‘do not stent’ approach may be a better option for cases in which stenting would lead to suboptimal results.”
Notably, the study report did not include angina results, which could have further reinforced the main reasoning many CTO operators have for performing this procedure in the first place.
Rao, who started a discussion on Twitter about this issue, said the main challenge with CTO PCI data is that registries capture hard outcomes because it’s “relatively easy” to do so. However, “if you look at PCI overall in the elective setting, it does not affect death or MI, so why would we expect it to do that in a CTO situation?” he asked. “There was a group of people who believe that a chronically totaled artery really was a high-risk lesion for poor outcomes, so if we open that we can potentially improve the risk of MI or even potentially improve survival. I think it’s pretty clear that's not the case, and these two studies now show that.”
At this point, the takeaway should be that “number one, the only reason to do CTO PCI is for symptom relief, and number two, our data collection strategies just have to get better at capturing angina relief and more patient-centered outcomes,” Rao said. “It is getting harder and harder to show that our strategies are actually going to affect any hard outcomes, because I think the randomized trials show that in the elective setting PCI doesn't. . . . It really is sort of a wake-up call for us to construct better data collection forms and better registries.”
Shoot for Complete and Optimal
After reviewing both papers for TCTMD, Kalra stressed that procedural safety is “paramount.”
“When we try to achieve results, we have to work very hard to make sure that when we're stenting these patients that we're using all of our best technologies and techniques to get optimal results with TIMI 3 flow and watching out for side branches,” he said. “It is not acceptable to just lose a side branch and say, ‘That's fine, it's a minor branch in comparison to what we've opened,’ because we now recognize that that in fact can lead to deleterious outcomes.”
It may be worthwhile to plan CTO PCIs as two staged procedures, Kalra said, where if an optimal result is not achieved in the first, subintimal tracking and reentry or subintimal plaque modification can be used to increase the likelihood of an optimal result in a secondary procedure.
“Periprocedural MIs are real and now we know that even in this subset where we lose side branches and that drives a large component of this endpoint, the loss of side branches is not denied,” he said. “As a community, we have to work very, very hard to prevent ourselves from having that problem. If that means using more retrograde in the context of an informed consent discussion, where we discuss MACE associated with these more advanced and more aggressive techniques, then that's fine. If you're going to take it on, then you have to do it right.”
That said, Kalra continued, it’s hard to glean anything more granular from either study given how fast the field moves, a point also made by Kawashima et al.
CTO PCI practiced today is different from what it once was, Kalra stressed. Now “it's different equipment, different techniques, and different stents,” he said, adding that ongoing trials and registries should be able to lend more insight into whether the “optimal result,” which has changed in recent years, will lead to changes in hard endpoints down the line.
The entire concept of “complete revascularization” also needs to be further defined, especially given the lack of core lab data in many occasions, Rao said. “The term gets thrown around a lot without really a lot of granularity on what it means.”
A big challenge that the entire field of interventional cardiology will be tasked with is how to move forward with CTO PCI, he said.
“[We have] these technique advances that allow us to address different lesions or more complicated situations and CTO PCI is one of them. The added layer of complexity for CTO PCI is that there is a fair amount of reimbursement at the physician-level—so you get a lot of RVUs for doing a CTO procedure—and, quite frankly, that’s part of defining oneself as a complex PCI operator is that you do CTOs. So when you have all those incentives it can become very tough to do a randomized trial,” observed Rao.
While many high-volume CTO operators have called for randomized trials in this space, they haven’t materialized, he continued. “There are folks who say, ‘I can get most people symptom free with very, very aggressive medical therapy,’ and another camp that says, ‘Well even if you try aggressive medical therapy, there's a subset that needs to have revascularization and that's where my skills come in.’ And probably the truth is somewhere in the middle. I think we absolutely need to have a randomized trial of CTO PCI to see if the risks associated with it are actually worth the benefits.”
Note: Ajay J. Kirtane, MD, a co-author of the paper by Guan et al, is a faculty member of the Cardiovascular Research Foundation, the publisher of TCTMD.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Kawashima H, Takahashi K, Ono M, et al. Mortality 10 years after percutaneous or surgical revascularization in patients with total coronary artery occlusions. J Am Coll Cardiol. 2021;77:529-540.
Moses JW, Prasad M. Are all total occlusions created equal? Striving for complete revascularization while differentiating apples from oranges. J Am Coll Cardiol. 2021;77:541-543
Guan C, Yang W, Song L, et al. Association of acute procedural results with long-term outcomes after CTO PCI. J Am Coll Cardiol Interv. 2021;14:278-288.
Ybarra LF, Bagur R. When something can be worse than failing: suboptimal results in CTO PCI. J Am Coll Cardiol Interv. 2021;14:289-291.
Disclosures
- The SYNTAXES study was supported by the German Foundation of Heart Research. The SYNTAX trial, during 0- to 5-year follow-up, was funded by Boston Scientific Corporation.
- The study by Guan et al was supported by research funding from the Chinese Academy of Medical Sciences Innovation Project (2018-12M-AI-007) and the Beijing Municipal Science and Technology Commission Project.
- Kawashima, Guan, Moses, Prasad, Ybarra, Bagur, and Rao report no relevant conflicts of interest.
- Kalra reports serving as a consultant to Boston Scientific and providing medical education for Abbott Vascular, Asahi, Abiomed, CSI, Translumina Therapeutics and Philips Healthcare.




Comments