DCBs Show Consistent Long-term Benefits in Complex Fem-Pop Patient Subsets
Separate analyses expand knowledge of endovascular therapy in long lesions as well as in smaller vessel diameters.
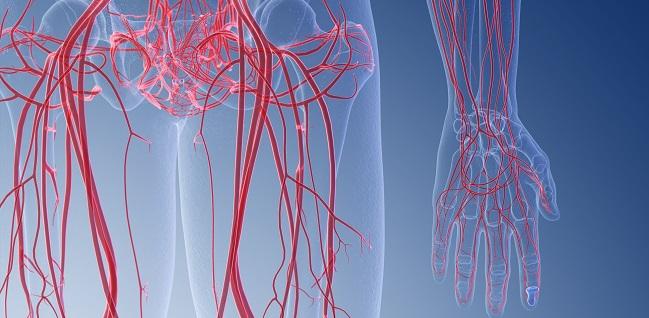
LEIPZIG, GERMANY—Two new analyses presented here support the use of endovascular drug-coated balloon (DCB) therapy in a variety of complex patient subsets, including long femoropopliteal lesions and small reference vessel diameters.
Both updates come from the real-world IN.PACT Global study, which in addition to its clinical cohort of 1,416 patients, also included a subset of 119 patients with lesion lengths of 15 cm or longer who were treated with a 150-mm paclitaxel-coated IN.PACT Admiral (Medtronic) that was not used in any of the clinical-cohort patients. The longer balloon was provided to only a subset of the 64 participating treatment centers throughout Europe, the Middle East, Latin America, and Asia, noted Marianne Brodmann, MD (Medical University of Graz, Austria).
The subset was predominantly male with high rates of hypertension and hyperlipidemia, consistent with the patients in the IN.PACT Global clinical cohort. However, while the clinical cohort excluded those with Rutherford classifications of 5 or 6, these patients were allowed into the subset.
Presenting 3-year efficacy outcomes for 107 of the 150-mm DCB patient group on Wednesday at LINC 2020, Brodmann said the 74.5% rate of freedom from clinically driven TLR translated to a mean number of days from balloon intervention to TLR of 540 for the cohort. The primary safety composite (freedom from device- and procedure-related death through 30 days plus freedom from target limb major amputation and clinically driven TVR within 12 months) was 73.6%, and the rate of all-cause death was 12.5%, with only one major amputation reported.
The analysis also included the causes of death among the 12 patients who died in year 3. Half of the deaths were cardiac-related, while the rest were attributed to respiratory issues (n = 3), infection (n = 1), other (n = 1), and unknown (n = 1).
According to Brodmann, the results are “really very good for this complex lesion cohort” given that mean legion length was 20 cm and nearly 60% of patients had total occlusions. She also pointed out that 87% of patients had calcified lesions, with 17% of those being severely calcified.
Consistent Results Across Vessel Sizes
The other IN.PACT Global analysis presented at LINC 2020 focused on outcomes of the DCB by reference vessel diameter in the clinical cohort.
“Numerous global studies have demonstrated the superiority of the DCBs over the conventional PTA for the treatment of PAD. However, poor outcomes of endovascular therapy in smaller fem-pop lesions have been reported,” observed Yoshimitsu Soga, MD, PhD (Kokura Memorial Hospital, Kitakyushu, Japan).
Patients in the analysis were categorized by reference vessel diameter into terciles: lower (mean, 4.1 mm), mid (mean, 5.0 mm), and upper (mean, 5.9 mm).
Freedom from clinically driven TLR through 12 months was highest in the upper tercile at 94.5%, but the mid and upper terciles did not lag far behind at 92.9% and 89.6%, respectively. When the cumulative incidence of the primary efficacy endpoint was compared across the three terciles, there was no significant difference (P < 0.001). Additionally, there were no differences across terciles for the individual endpoints of clinically driven TLR (P = 0.029) or any TLR (P = 0.037).
Similarly, safety analyses through 12 months showed no difference by tercile for the primary composite safety endpoint nor in the individual endpoints of all-cause death, clinically driven TLR, major target limb amputation, or thrombosis at the target lesion.
During his presentation, Soga showed a peripheral angiogram from a 74-year-old woman with a reference vessel diameter of just 3.6 mm. While tiny compared with the majority of the IN.PACT cohort, Soga said such small vessel sizes are actually quite common among PAD patients in Asian countries. The patient was treated with the smallest available size of the DCB, the 4.0 mm, and continued to be free of restenosis out to 4 years, he reported.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Brodmann M. IN.PACT global study 150mm cohort: outcomes through 3 years. Presented at: LINC 2020. January 29, 2020. Leipzig, Germany.
Soga Y. Drug-coated balloon outcomes in the femoropopliteal vessels of a Japanese population–impact of vessel size. Presented at: LINC 2020. January 29, 2020. Leipzig, Germany.
Disclosures
- None disclosed.


Comments