Good 3-Year Outcomes With Aortic Valve-in-Valve Replacement for Failed SAVR
Early outcomes look favorable, but observers say a randomized trial against redo surgery is warranted.

NEW YORK, NY—Midterm results out to 3 years show that transcatheter aortic valve-in-valve (ViV) replacement for a failed surgical valve is a safe procedure associated with lower risks of death and stroke than native TAVI, a new registry analysis showed.
The promising findings, which were presented last week at New York Valves 2024, were seen across a wide range of patients, including those at low, intermediate, and high risk for surgery.
The results, according to lead investigator Tsuyoshi Kaneko, MD (Washington University School of Medicine, St. Louis, MO), suggest that “consideration may be given to broadening the indication of aortic valve-in-valve.” At the moment, the US Food and Drug Administration only allows aortic valve-in-valve replacements for patients deemed to be at high risk for surgery, he said.
Despite those criteria, as well as limited midterm or long-term data showing the safety and efficacy of ViV procedures for a failed surgical device, “the valve-in-valve TAVI numbers have been increasing in the United States,” said Kaneko. The annual number of repeat SAVRs, by contrast, has been relatively stagnant.
Surgeon Michael Reardon, MD (Houston Methodist DeBakey Heart & Vascular Center, TX), one of the panelists during the late-breaking clinical trial session, said he was struck that those undergoing ViV procedures had lower rates of stroke and mortality than the native-valve patients, despite having a higher STS risk score prior to propensity matching.
“Now the slope of your mortality curve is really related to your intrinsic risk of dying, which is related to age and how sick you are whereas the STS is your risk of dying at surgery, which includes both physiology and anatomy,” he said. “I would expect the native valves, which are going to get better hemodynamics, to survive longer than valve-in-valve.”
Kaneko said that this phenomenon has been observed in other registry analyses that have propensity-matched patients. While the native TAVI group had a higher STS score than the ViV group before matching, they were also quite a bit older (mean 73.8 vs 79.0 years). Kaneko said the new data indicate that ViV is safe to perform in appropriate patients, at least to the 3-year mark, but do not necessarily imply that patients will live longer with the ViV procedure than those undergoing native TAVI.
Propensity-Matched Data From TVT Registry
The analysis included patients enrolled in the STS/ACC TVT Registry between 2015 and 2023, of whom 13,711 underwent transcatheter aortic ViV replacement and 368,176 underwent native TAVI, all using balloon-expandable valves. From here, the analysis focused on 25,824 propensity-matched patients undergoing the ViV procedure or native TAVI for symptomatic severe aortic stenosis. Over time, the number of aortic ViV cases increased from 450 at 68 sites in 2015 to 2,258 cases at 510 sites through the first 9 months of 2023.
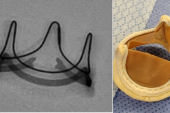
At discharge, the ViV patients had smaller effective orifice areas (EOA) and higher mean gradients but less paravalvular leak than those who underwent native TAVI. At 3 years, patients undergoing aortic ViV replacement had a significantly lower risk of death (HR 0.72; 95% CI 0.67-0.77) and stroke (HR 0.83; 95% CI 0.73-0.94) when compared with patients undergoing native TAVI. Those who underwent ViV procedures had a more than twofold higher risk of reintervention by 3 years, however (HR 2.36; 95% CI 1.86-2.99).
The researchers also performed several subanalyses. In the first, they stratified patients by surgical risk using the STS score. Across the range of STS scores, the 3-year risk of mortality was higher in patients undergoing native TAVI than in those undergoing a ViV procedure. Like the overall cohort, the need for aortic-valve reintervention was higher in the ViV patients.
Next, they stratified patients based on the type of balloon-expandable valve used in the ViV procedure. Here, they observed no difference in clinical outcomes at 30 days between ViV performed with the next-generation Sapien 3 Ultra Resilia and older Sapien 3/Ultra bioprostheses (all Edwards Lifesciences). However, mean gradients at discharge were lower and EOAs larger with the Sapien 3 Ultra Resilia at all valve sizes.
Finally, the group looked at ViV performed in failed stented versus stentless surgical valves. At discharge, patients with a ViV performed in a stentless valve had larger EOAs and lower mean gradients. At 3 years, however, there was no significant difference in clinical outcomes in those with a failed stented or stentless valve treated with a ViV procedure. Reintervention rates were higher in patients with a failed stented valve (4.5% vs 1.9% with a stentless surgical valve; P = 0.02).
Administrative Data and Randomized Trials
Vinayak Bapat, MD (Allina Health Minneapolis Heart Institute, MN), the discussant following Kaneko’s presentation, said that while these results are excellent, he questioned whether the follow-up is long enough to affirm safety.
“We are promising patients 10 years, 15 years, so should we still classify [3 years as ‘mid-term’]?” he asked. Bapat also questioned whether there was any difference in mortality with ViV replacement based on valve size. “We know from the TVT Registry that once the smaller valves are used, it can affect outcomes,” said Bapat.
Kaneko agreed, noting that they plan to reperform the same analysis with 5-year follow-up. He said they were unable to propensity-match patients based on valve size, which is one of the limitations of the registry-based analysis.
During the discussion, Martin Leon, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), called the new analysis “helpful,” noting that many physicians are already performing ViV procedures in lower-risk patients despite not having a good sense of outcomes. Leon added that he’s been troubled by some of the “hysteria” around recent administrative data suggesting an accrual of clinical events with longer follow-up in patients undergoing aortic ViV for a degenerated surgical valve.
“That has resulted in a call to arms that we need to do a redo SAVR versus surgical valve-in-valve study,” said Leon.
Kaneko said that administrative data are inherently flawed in that they are unable to account for multiple factors, including frailty, that could explain the differences seen in those prior analyses. Nonetheless, he thinks a randomized, controlled trial of redo SAVR versus ViV replacement would be warranted for low-risk patients, particularly younger ones, powered to see a difference in clinical outcomes.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Kaneko T, Kapadia S, Babaliaros V, et al. Midterm outcomes of balloon-expandable TAVR for the treatment of failed bioprosthetic valves in the United States. Presented at: New York Valves 2024. June 7, 2024. New York, NY.
Disclosures
- Kaneko reports consulting fees/honoraria from Edwards Lifesciences, Medtronic, Abbott, Johnson & Johnson.
- Bapat reports consulting fees/honoraria from Edwards Lifesciences, Medtronic, 4C, and Anteris.
- Leon reports grant/research support from Boston Scientific, Edwards Lifesciences, Abbott, and Medtronic.
- Reardon reports consulting fees/honoraria from Medtronic, Boston Scientific, WL Gore, and Abbott. He reports serving on the advisory board for JValve, High Life, BCSI, Medtronic, and GL Gore.




Comments