IVL Effective in Severely Calcified Lesions, Especially in Women
EMPOWER-CAD and BALI reinforce the utility of coronary lithotripsy, but the effect on hard outcomes is still unclear.
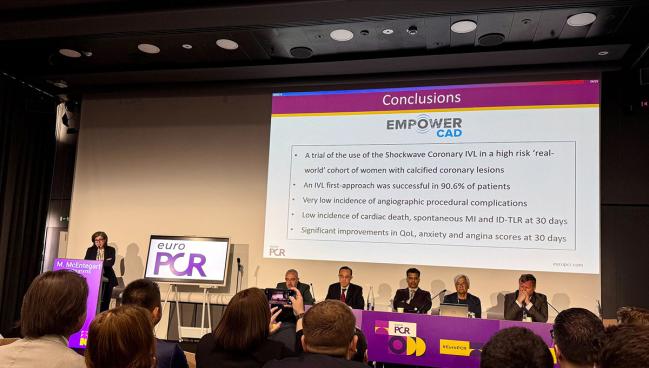
Photo Credit: Shockwave Medical
PARIS, France—Intravascular lithotripsy (IVL) can safely aid in lesion preparation before PCI in patients with severe calcification and can lower the rate of postprocedural patient adverse outcomes, according to data from two new studies presented here at EuroPCR 2025.
In BALI, presented by Andreas T. Kristensen, MD (Arhus University Hospital, Denmark), there was a significant advantage with coronary IVL (Shockwave Medical) in terms of the combined primary endpoint of procedural failure and 1-year target vessel failure among patients who were randomized to lithotripsy or conventional care.
Notably, researchers did not find a significant benefit in terms of target vessel failure alone.
In EMPOWER CAD, which was led by Margaret McEntegart, MD, PhD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), investigators focused exclusively on female patients and showed the IVL-first approach was successful for more than nine in 10 women. There were low rates of angiographic procedural complications, few clinical events at 30 days, and significant improvements in both quality of life and symptoms over follow up.
Neither study answered all the open questions floating around about IVL, such as how the tool is best used in sequence with other debulking devices as well as its potential to cause periprocedural MI, and cost is still a significant barrier, though researchers across the board felt the data were encouraging enough to support more routine use of the device.
“Lithotripsy should be routinely used in most patients, I would say,” Kristensen told TCTMD. “But we have to keep in mind that our primary endpoint was partly driven by a surrogate endpoint—imaging-based residual area stenosis—and whether this directly translates to improved clinical outcomes, target vessel failure, and improved prognosis, we would really need a 2,000-patient randomized control trial to confirm that.”
Renu Virmani, MD (CVPath Institute, Gaithersburg, MD), who served as a discussant during the EuroPCR session, said that IVL makes sense from a pathological point of view.
“I can tell you the cracks are very clean, and therefore I’m not surprised that the balloon dilatation is much easier,” she said. “I would say in the long run, this is the better way to go than the conventional way of just ballooning. There, you’re doing it blind. You are tearing the vessel apart. Here at least you’ve broken the calcium, and that’s where it’ll separate when you do a balloon afterwards.”
EMPOWER CAD
Coronary IVL, approved in Europe in 2017 and in the US in 2021, has aided physicians who regularly perform complex PCI, with real-world data suggesting positive outcomes. However, the technology has faced criticism over its high price, and the Centers for Medicare & Medicaid Services reacted to these concerns by allowing it to be better reimbursed as an add-on payment.
Data on lithotripsy in women has also been limited, as the population of DISRUPT CAD III—the trial that led to FDA approval—was made up of mostly men.
In EMPOWER CAD, which enrolled 399 women between April 2023 and October 2024, the only exclusion criteria were cardiogenic shock and in-stent restenosis in order to have a high-risk population that mimics real-world practice. Almost half of patients (45.6%) were enrolled with stable angina, but 23.3% had NSTE ACS and 2.5% had STEMI. All patients were deemed candidates for IVL before randomization, and while predilatation was used in 68.4%, rotational atherectomy and cutting/scoring balloons were only deployed in 7.3% and 2.0%, respectively.
Of the 449 lesions, 7.3% were in the left main, and 12.6% and 25.1% of patients had multiple lesions or one or more nontarget lesions, respectively. In total, 99.3% of patients had core lab- confirmed severe calcification.
Post-IVL, rotational atherectomy was needed in 0.4% and cutting/scoring balloons in 2.9%. Procedural success was 86.9%, with a final mean minimal lumen diameter of 2.6 mm.
The incidence of the primary safety endpoint of target lesion failure at 30 days was 12.1%, including five cardiac deaths (1.3%),42 MIs (rates of 9.6% and 1.5% for periprocedural and spontaneous, respectively), and five cases of ischemia-driven target lesion revascularization (1.3%).
Regarding the periprocedural MIs, which were defined using the broader SCAI definition, the “majority were biomarker elevations alone without clinical symptoms or sequelae,” said McEntegart. Using the Fourth Universal Definition and ARC-2 definition of MI, the rates were 4.5% and 1.5%, respectively.
McEntegart said she slightly regrets using the SCAI definition of periprocedural MI given how the high rate looks but said “it’s important for us to not be in denial about what happens in these high-risk patients.” Understanding enzyme elevations after complex PCI is important “because that's how we continue to iterate and improve what we do,” she added. “It’s incumbent on us and on the operators receiving the information to understand what the data means.”
There were six type D dissections following IVL and three perforations after stenting, but all complications were resolved by the end of the procedure with no clinical events. Quality of life as measured by the EQ-5D-5L and SAQ-7 increased by 12% and 26%, respectively, over 30 days, while anxiety as measured by the GAD-7 survey went down by 38%.
McEntegart, who uses IVL “pretty much every day that I’m in the lab,” said the study findings confirm the technology can be used “in a large proportion of our patients as your first and only calcium mediation-technology.”
Because of the complexity of the EMPOWER CAD cohort, McEntegart expected to see a higher risk of procedure-related complications. “But actually, it’s very reassuringly low,” she noted. “So, what it makes me think is, okay, when I’m dealing maybe specifically with female patients, with all their associated morbidities and frailties, maybe this should be my approach.”
Notably, 70% of the investigators in the study were female, McEntegart highlighted. “We wanted to use it as an opportunity to encourage more female operators to get involved in clinical research,” she said. “We feel proud of the fact that hopefully we've engaged a younger generation of women.”
BALI Data
The BALI trial was a smaller undertaking, with 200 patients (mean age 75 years; 23.5% female) from nine European centers randomized to IVL or usual care. Most presented with chronic coronary syndromes (77.5%), and just over half of the total lesions were in the LAD (< 1% in the left main). Almost 97% of lesions were confirmed to be severely calcified by a core lab analysis.
In this study, operators were encouraged to use their judgement on the use of adjunctive tools. Rotational atherectomy was used in 31% and 42% of the IVL and conventional therapy arms, respectively, noncompliant balloons were used in 69% and 82%, and cutting/scoring balloons in 12% and 57%. The researchers did not provide data on the sequence in which these tools were used.
The risk of procedural failure/1-year target vessel failure was lower in the IVL arm compared with conventional therapy (35.4% vs 51.5%; RR 0.69; 95% CI 0.48-0.97). There were no significant differences in the risks of residual area stenosis ≥ 20% on OCT (32.3% vs 44.6%; RR 0.73; 95% CI 0.49-1.04) and target vessel failure at 1 year (4.0% vs 10.9%; RR 0.37; 95% CI 0.07-1.09).
There were no periprocedural MIs in the lithotripsy group, but the rate was 5% in the conventional arm (ARC-2 definition; P = 0.07). The perforation rates were similar between the strategies, with two distal wire perforations in the IVL group deemed not related to the device.
Researchers identified trends favoring IVL for both in-stent minimal lumen area and residual area stenosis on OCT response regarding the final post-procedural OCT.
McEntegart, who also served as the discussant for BALI, acknowledged the challenge in performing a randomized trial, and in this case especially, controlling for the interaction between multiple different debulking tools to treat these lesions.
“It’s quite difficult to do a clean comparison because often in these cases you use multiple technologies in both arms, you get lots of crossover,” she said, adding that the ongoing 400-patient Short-Cut trial, which designated a more structured pathway of using adjunct devices, should help in this regard.
But she sees a bright future for IVL, especially with how easy it is to use compared with rotational atherectomy, say. “It’s a very, very accessible technology,” McEntegart said, adding that its main limitation is cost. Also, she added, as intravascular imaging use becomes more routine, it’s likely that physicians will more appropriately recognize lesion calcium severity and be able to deploy tools like IVL more effectively.
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
McEntegart M. The EMPOWER CAD study: women with calcified coronary arteries treated with intravascular lithotripsy. Presented at: EuroPCR 2025. Paris, France. May 20, 2025.
Kristensen AT. Randomised comparison of lithotripsy vs. conventional preparation in severely calcified coronary lesions (BALI). Presented at: EuroPCR 2025. Paris, France. May 20, 2025.
Disclosures
- EMPOWER CAD was sponsored by Shockwave Medical.
- BALI was supported by Abbott Vascular and Shockwave Medical.
- McEntegart reports receiving honoraria from and serving on the speaker’s bureau for Shockwave Medical.





Comments