IVUS-Guided PCI Gains Support With Longer-Term ULTIMATE Results
“We really should . . . shift our thought process to using more IVUS guidance for our patients,” B. Hadley Wilson says.
The benefits of IVUS guidance in an all-comers population of patients undergoing PCI with second-generation DES persist through at least 3 years, extended follow-up of the ULTIMATE trial shows.
Target vessel failure (TVF) remained lower at that time point in patients whose procedure was guided by IVUS versus angiography (6.6% vs 10.7%; P = 0.01), a difference driven mostly by a reduction in clinically driven TVR (4.5% vs 6.9%; P = 0.05), Jun-Jie Zhang, MD, PhD (Nanjing First Hospital, Nanjing Medical University, China), reported during the virtual TCT Connect 2020.
Results favoring IVUS guidance were even better when criteria for an optimal procedural result were met. The findings were published simultaneously online in JACC: Cardiovascular Interventions.
“Both [the] IVUS-XPL trial and our study verified the gradually increasing clinical benefits of IVUS-guided DES implantation,” the investigators write in their paper, noting that a recent Medicare analysis showed that IVUS was used in only 5.6% of PCIs performed between 2009 and 2017.
“In view of the evidence from randomized trials, it is time to overcome the barriers, including cost, availability, expertise, and procedure prolongation, to promote IVUS use in daily clinical practice,” they say. “Further randomized studies are also warranted to identify the most optimal criteria for IVUS guidance and how to achieve these IVUS-defined optimal criteria.”
B. Hadley Wilson, MD (Sanger Heart & Vascular Institute, Atrium Health, Charlotte, NC), speaking for the American College of Cardiology, agreed that the totality of the evidence supports greater use of IVUS to improve patient outcomes. He added that these ULTIMATE results will help push interventional cardiologists in that direction, particularly for patients with multivessel disease and complex anatomy.
But, he told TCTMD, “we really should . . . shift our thought process to using more IVUS guidance for our patients across the board.”
ULTIMATE at 3 Years
Prior trials and observational studies have pointed to the benefits of using IVUS to guide PCI across lesion types. In ULTIMATE, for instance, the rate of TVF (cardiac death, target-vessel MI, and clinically driven TVR) was lower after IVUS-guided versus angiography-guided PCI in all-comers at 1 year. But the potential long-term benefits have not been well studied.
ULTIMATE, conducted at eight Chinese centers, compared the two strategies in 1,448 patients who had silent ischemia, stable or unstable angina, or MI with more than 24 hours between chest pain and admission. Most patients presented with ACS (78.5%) and had multivessel disease (54.9%), with a large proportion having diabetes (30.6%). Patients in the IVUS group, on average, received larger stents with more frequent postdilation using larger noncompliant balloons at higher pressures.
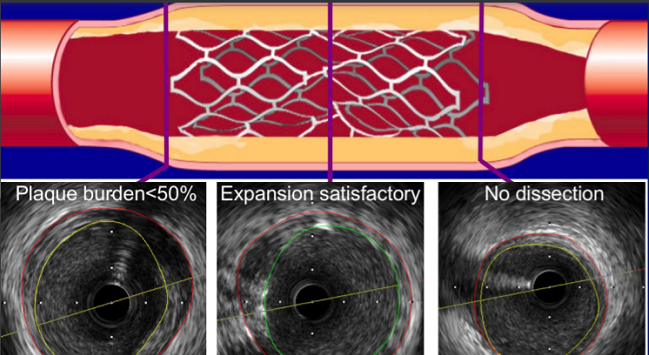
The investigators defined an optimal procedure based on three IVUS criteria (53% of patients met all of them):
- Minimum lumen area (MLA) of the stent segment > 5.0 mm2 or 90% of the MLA at the distal reference segments
- Plaque burden at 5 mm proximal or distal to the stent edge < 50%
- No edge dissection involving media with a length longer than 3 mm
Similar to what was seen at 1 year, TVF was significantly lower in the IVUS group at 3 years (HR 0.60; 95% CI 0.42-0.87), mostly due to less clinically driven TVR. There were no differences between groups in cardiac death or target-vessel MI. Findings were consistent across subgroups.
The main safety endpoint was definite/probable stent thrombosis—there was one case in the IVUS group and eight in the angiography group (0.1% vs 1.1%; P = 0.02).
“Our study, in line with other studies, showed that IVUS guidance could optimize stent implantation and reduce the rates of repeat revascularization and stent thrombosis compared with [rates] when using angiography guidance,” the investigators write.
Underuse of IVUS, Coronary Physiology Assessment
Juan Granada, MD, president and CEO of the Cardiovascular Research Foundation (New York, NY), who moderated a press briefing at which the results were discussed, said “this is a great example of how imaging can really guide better procedures. . . . Again and again and again, we see better outcomes with IVUS-guided studies.”
Addressing the documented underuse of IVUS, however, Granada said, “I don’t know what we need to do to essentially train operators and actually tell operators that precise PCI and thoughtful PCI actually does lead to better clinical outcomes.”
This is a great example of how imaging can really guide better procedures. . . . Again and again and again, we see better outcomes with IVUS-guided studies. Juan Granada
Discussant Allen Jeremias, MD (St. Francis Hospital, Roslyn, NY), also pondered the problem, not just with IVUS but also with coronary physiology assessments. “We know that when patients have those procedures, they have better outcomes,” he said. “So I think we have the guidance. We know how to do it. The problem is how do we convince more people to do it, because ultimately both physiology and imaging are underutilized.”
Study after study, including ULTIMATE, reiterate “the importance of routine imaging in our patients,” Jeremias said.
To TCTMD, Wilson cited some possible reasons why interventional cardiologists are not using IVUS more frequently: greater procedural time and contrast volume, which could increase the risk of contrast-induced nephropathy, as well as the added cost of the imaging. Moreover, he said, assessments of coronary physiology are a popular and important competitor to IVUS.
Jeremias disputed cost’s role in the underuse of IVUS. “I refuse to believe that we don’t want to spend . . . 5 minutes to do an IVUS study to get a better result because we don’t get paid enough,” he said.
He pointed to two other possibilities: lack of a large absolute impact on patient outcomes and issues with training. The relative benefits of IVUS guidance in terms of reducing outcomes like MI, stent thrombosis, and even mortality are large at 30% to 50%, he noted. “The problem is that the absolute difference is small because the technology we have now is so good that you might only change or improve outcomes in one, two, three, four patients out of a hundred. And because it’s only a few patients really that you change outcomes in, I think that’s why the adoption isn’t so large even though the relative difference is very large.”
Additionally, “my gut feeling is that fellows are just not well trained coming out of training programs,” he said, citing his own study showing that only 30% to 40% of fellows said they were comfortable performing IVUS on their own after training. “I think that’s really what the problem is.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Gao X-F, Ge Z, Kong X-Q, et al. Three-year outcomes of the ULTIMATE trial comparing intravascular ultrasound versus angiography-guided drug-eluting stent implantation. J Am Coll Cardiol Intv. 2020;Epub ahead of print.
Disclosures
- ULTIMATE was funded by the National Natural Science Foundation of China, and was jointly supported by the Six Talent Peaks Project of Jiangsu Province, Social Development Project of Jiangsu Province, Jiangsu Commission of Health, Jiangsu Provincial Special Program of Medical Science, Nanjing Commission of Health, and Nanjing Health Youth Talent Training project.
- Zhang, Wilson, and Granada report no relevant conflicts of interest.
- Jeremias reports personal fees from Abbott Vascular, Boston Scientific, Volcano Corporation, and ACIST.


Comments