More ARNI Insights Fortify Role in ‘Below Normal’ LVEF: PARAGLIDE-HF
The trial, as well as pooled data with PARAGON-HF, should solidify a role for sacubitril/valsartan after worsening HF events.
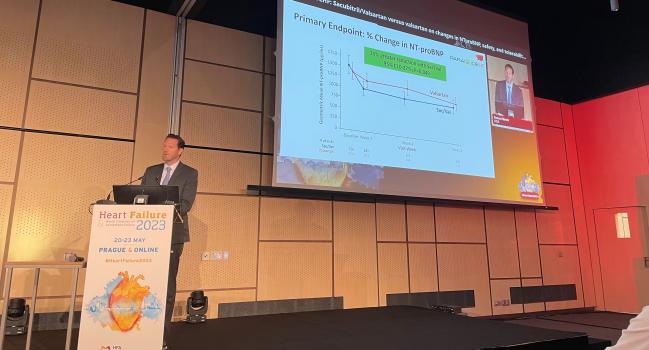
PRAGUE, Czechia—In patients with an ejection fraction > 40% recovering from a worsening heart failure (HF) event, sacubitril/valsartan (Entresto; Novartis) led to greater reductions in NT-proBNP levels than did valsartan alone in the randomized PARAGLIDE-HF trial, presented at the European Society of Cardiology Heart Failure 2023 Congress.
And in an analysis combining PARAGLIDE-HF with similar patients from the larger PARAGON-HF trial, also released here today, investigators saw a clear and rapid reduction in cardiovascular and renal events, with benefits appearing within the first few weeks of treatment—both among pooled patients stabilized after a recent event and in the two pooled trials overall.
In both PARAGLIDE-HF and in the pooled analyses, the treatment effects were larger among patients with an ejection fraction ≤ 60%. Both studies also confirmed a risk of increased symptomatic hypotension previously flagged with angiotensin receptor-neprilysin inhibitor (ARNI) use.
“In light of similar findings from PARAGON-HF, these [PARAGLIDE-HF] data provide additional support for a potential treatment benefit of sacubitril/valsartan in HF with an EF > 40%, particularly in those with an EF below normal,” said Robert Mentz, MD (Duke Clinical Research Institute, Durham, NC), who presented the PARAGLIDE-HF results. “These data may influence future guidance.”
The most recent US HF guidelines recommend consideration of an ARNI in chronic heart failure with mildly reduced (HFmrEF) or preserved (HFpEF) heart failure (LVEF ≥ 50%). The 2021 European HF guidelines, by contrast, acknowledge that new evidence is forthcoming but make no formal recommendations for sacubitril/valsartan in HFpEF; they do say, though, that the agent “may be considered” in HFmrEF.
What’s more, said Mentz, it wasn’t clear whether swiftly initiating the combination drug in these patients after a worsening heart failure event would be safe and beneficial. Patients with recently decompensated HF were excluded from the larger PARAGON-HF trial; however, a post hoc analysis had suggested there might be even larger gains with sacubitril/valsartan in patients who’d been recently hospitalized.
These data may influence future guidance. Robert Mentz
Keep in mind, Mentz told TCTMD, that despite positive trials and guideline support, uptake of these agents has lagged. “It's now been seen multiple times: that if you don't start [sacubitril/valsartan] in the hospital, patients aren't going to be on it at a couple of months or even a year later. It's just not used,” he said.
PARAGLIDE-HF was simultaneously published in the Journal of the American College of Cardiology. In the paper, the authors note that their trial is intended to complement PARAGON-HF, “similar to the manner in which PIONEER-HF complemented PARADIGM-HF” in heart failure with reduced ejection fraction (HFrEF) by clarifying the role of initiating the drugs soon after a worsening HF event.
PARAGLIDE-HF
The PARAGLIDE-HF trial was launched prior to PARAGON-HF, Mentz told TCTMD, in part to clarify this question about drug safety and efficacy in stabilized patients who’d been recently hospitalized or who’d sought urgent care for worsening HF.
The trial randomized 466 patients to the ARNI or valsartan alone, started in-hospital or within 30 days of a worsening HF event. By week 8, patients randomized to sacubitril/valsartan had a time-averaged 15% greater reduction in NT-proBNP—the primary endpoint—than patients randomized to valsartan, narrowly meeting the bounds of statistical significance (RR 0.85; 95% CI: 0.73-0.999).
A hierarchical endpoint of CV death, HF hospitalization, urgent HF visits, and change in NT-proBNP trended in favor of sacubitril/valsartan but was not statistically significant. The advent of the COVID-19 pandemic, Mentz told TCTMD, stymied some initial hopes of powering the trial for clinical endpoints.
In terms of safety, worsening renal function was significantly more common among valsartan-treated patients, whereas symptomatic hypotension was more common among ARNI-treated patients.
Given ongoing questions as to a threshold effect with sacubitril/valsartan, investigators prespecified a primary endpoint analysis using a LVEF of 60% as a cutoff. Here, said Mentz, patients with an EF ≤ 60% randomized to the combination therapy experienced a 22% greater reduction in NT-proBNP than those taking valsartan alone. NT-proBNP levels were roughly similar between treatment arms, however, in patients with an LVEF above 60%.
“So, as I think of applying this clinically, I say: if I've got a patient in front of me that does have an EF greater than 40%, their NT proBNP is up, we're managing their other comorbidities, we know that so many of them are going to be on an ACE inhibitor and ARB—now we’ve got data showing that ARNIs are better,” Mentz told TCTMD.
The symptomatic hypotension, he clarified following his presentation, tended to be more common in patients with LVEFs greater than 60%, but a deeper dive is planned to evaluate this further.
For now, Mentz noted to TCTMD, one thing he considers in his practice is swapping out a patient’s calcium channel blocker or other blood pressure medications—or holding off on initiating an antihypertensive—if he is starting that patient on an ARNI, in the hopes of averting hypotension symptoms.
Pooled Analysis With PARAGON-HF
Following Mentz’s presentation, Muthiah Vaduganathan, MD, MPH (Brigham and Women’s Hospital, Boston, MA), presented a primary, prespecified pooled analysis combining the PARAGLIDE-HF cohort with 622 PARAGON-HF patients who had been recently hospitalized for worsening HF, yielding a total of 1,088 patients and sufficient power to address clinical outcomes.
In this combined group, rates of total worsening HF events and CV death were significantly lower in the sacubitril/valsartan patients than in the valsartan group (27.5 vs. 34.5 events per 100 patient-years; RR 0.78; 95% CI 0.61-0.99).
In a secondary analysis, Vaduganathan and colleagues then pooled all participants from both trials (n= 5,262) and again demonstrated a significant reduction in total worsening HF events and CV death (RR 0.86; 95% CI 0.75-0.98), although the absolute difference was smaller (14.5 per 100 patient-years for the ARNI and 16.8 per 100 patient-years for valsartan alone).
Still, stressed Vaduganathan, the benefits emerged early: the first nominal statistical significance was evident on day 9 after medication initiation. “These clinical benefits appear to accrue extremely rapidly,” he commented.
Speaking with TCTMD, Vaduganathan agreed that the magnitude of absolute benefit in the overall pooled analysis is noticeably lower than that seen in the decompensated patients, but said that this makes sense, biologically.
“I do believe that there are benefits across the board [with sacubitril/valsartan] but the magnitude of benefit in absolute terms is definitely magnified as you get closer to a heart failure event,” he said. “That perhaps reinforces the fact that a patient presenting with acute decompensated heart failure or shortly thereafter offers a great timepoint for implementation.”
The analyses were simultaneously published online in the European Heart Journal.
Risks and Benefits
As in the smaller PARAGLIDE-HF trial, adverse renal events were significantly reduced in the sacubitril/valsartan group in the pooled analyses, while rates of symptomatic hypotension were greater, reaching 50% higher in all participants.
Here, too, benefits of the combination drug were seen among patients with LVEF ≤ 60% but not in patients with EFs > 60%, both in the primary pooled analysis of recent worsening HF events and in the entire pooled group.
“Taken together, these data really strengthen the current guidance and evidence base supporting the use of sacubitril/valsartan in patients with heart failure with mildly reduced or preserved ejection fraction, particularly in those with an LVEF below normal and across clinical care settings, whether in ambulatory care, recently hospitalized, or acutely hospitalized,” Vaduganathan concluded.
Implementing the Evidence
To TCTMD, Mentz, stressed the importance of discussing medication changes with patients, particularly the cost considerations, which for many patients can be a deal breaker. The evidence to date supports swift initiation of SGLT2 inhibitors, which are also expensive, but so long as patients have an EF of less than 60%, an ARNI could be started a few days later or within 30 days, he suggested.
“I would underscore from the analysis that [Vaduganathan] presented that the time to benefit was 9 days,” Mentz added. Waiting a month to initiate sacubitril/valsartan would be “time wasted” in the context of seeing that early benefit.
And while the prespecified aim of the pooled analysis was to zero in on patients treated within the window of time after a worsening heart failure event, pooling all patients from both trials also helps resolve an outstanding question, Mentz pointed out. As previously reported by TCTMD, PARAGON-HF missed its primary endpoint, although subgroup analyses at the time suggested that sacubitril/valsartan was beneficial among patients with EFs of 45% to 57%. By adding in this “handful” of HFmrEF and HFpEF patients from PARAGLIDE-HF, a clearer picture emerges, Mentz said.
“If you had a family member with HFpEF, with all these evolving data, which therapies would you use? You’d consider an SGLT2 inhibitor, and you’d consider an ARNI,” he specified.
Keeping that 60% cutoff in mind is important, stressed Vaduganathan during the Q&A following his talk.
“Ultimately both pooled analyses, whether taking a more narrow look at that worsening heart failure cohort or the overall cohort, did demonstrate significant reductions in cardiovascular events,” he said. “But in terms of clinical implementation, it does seem our highest value of utilization of this therapy appears in that population with an LVEF below normal.”
I think there's now compelling evidence that ARNIs should be a part of foundational therapy. Muthiah Vaduganathan
Session moderator Marco Metra, MD (University of Brescia, Italy), speaking with TCTMD after the session, said he thinks the trials, taken together, “may have an impact on practice: in essence leading to larger use of sacubitril/valsartan versus valsartan in patients with an ejection fraction above 40%”
Demonstrating a benefit of these agents in patients recovering from an episode of decompensation is important, he continued. “This is a patient population at high risk, where the likelihood of having an improvement is higher with evidence-based medicine.” In this group, safely implementing effective agents in a timely fashion is “another important message” from these studies, he said.
Vaduganathan, to TCTMD, suggested that people should take particular note of the reduction in adverse renal events across multiple markers of worsening renal function. “This is probably some of the best evidence we have from a clinical trial perspective in HFpEF of any therapy reducing these types of kidney outcomes,” he noted.
Predicting that this will be the last of the major “discovery” trials for sacubitril/valsartan, Vaduganathan agreed that in the years ARNIs have been available, adoption has been sluggish.
“I think the reason that there's been a lukewarm reception has been some implementation barriers, but I think also that people were relatively unconvinced after PARAGON-HF. Yes, PARAGON-HF suggested some signals, but I think people were kind of awaiting additional trial evidence and even though [PARAGLIDE-HF] is a kind of modest-sized trial, there is pretty striking consistency between the two trials in terms of the subgroups that benefit. I think this adds credence that this is a real finding,” he said. “I think there's now compelling evidence that ARNIs should be a part of foundational therapy.”
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Mentz RJ, Ward JH, Hernandez AF, et al. Angiotensin-neprilysin inhibition in patients with mildly reduced or preserved ejection fraction and worsening heart failure. J Am Coll Cardiol. 2023;Epub ahead of print.
Vaduganathan M, Mentz RJ, Claggett BL, et al. Sacubitril/valsartan in heart failure with mildly reduced or preserved ejection fraction: a pre-specified participant-level pooled analysis of PARAGLIDE-HF and PARAGON-HF. Euro Heart J. 2023;Epub ahead of print.
Disclosures
- PARAGLIDE-HF was funded by Novartis.
- Mentz reports receiving research support and/or honoraria from Novartis, Abbott, American Regent, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Boston Scientific, Cytokinetics, Fast BioMedical, Gilead, Innolife, Eli Lilly, Medtronic, Medable, Merck, Novo Nordisk, Pharmacosmos, Relypsa, Respicardia, Roche, Sanofi, Vifor, Windtree Therapeutics, and Zoll.
- Vaduganathan reports receiving research grant support, speaking engagements, or advisory board payments from American Regent, Amgen, AstraZeneca, Bayer, Baxter Healthcare, Boehringer Ingelheim, Chiesi, Cytokineitcs, Lexicon Pharmaceuticals, Merck, Novartis, Novo Nordisk, Pharmacosmos, Relypsa, Roche Diagnostics, Sanofi, and Tricog Health, as well as serving on clinical trial committees for studies sponsored by AstraZeneca, Galmed, Novartis, Bayer AG, Occlutech, and Impuse Dynamics.





Comments