OCT-Guided PCI Bests Angiography in ACS Patients: OCCUPI
OCT seems to reduce periprocedural MI, a benefit not seen in the chronic coronary syndrome patients that deserves further study.
PARIS, France—In patients with ACS and complex lesions, the incidence of adverse events is lower when OCT rather than angiography is used to guide PCI, according to a subanalysis of the OCCUPI trial.
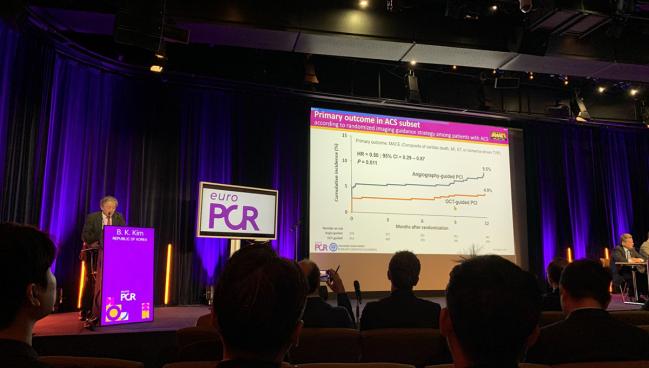
At 1 year, the combined rate of cardiac death, MI, stent thrombosis, or ischemia-driven TVR was markedly lower in the OCT-guided group (4.9% vs 9.5%; HR 0.50; 95% CI 0.29-0.87).
This is in line with the primary results of OCCUPI, which were released last year and showed the benefit of OCT over angiographic guidance was driven by lower rates of spontaneous MI and TVR in patients with a variety of anatomically complex lesions.
The new data, presented here last week at EuroPCR 2025, focused on 790 patients with ACS in the 1,604-patient trial.
“These findings directly support the use of OCT as an effective intravascular imaging technique to guide PCI in ACS patients with complex lesions as endorsed by the current guidelines,” Byeong-Keuk Kim, MD, PhD (Severance Hospital, Yonsei University College of Medicine, Seoul, Republic of Korea), reported.
The American College of Cardiology, the American Heart Association, and the Society for Cardiovascular Angiography and Interventions (ACC/AHA/SCAI) guidelines for coronary revascularization recommend IVUS for procedural guidance, particularly in cases of left main or complex CAD, while OCT is considered a reasonable alternative for procedural guidance, except in ostial left main disease. The European Society of Cardiology and European Association for Cardio-Thoracic Surgery (ESC/EACTS) also recommend IVUS or OCT to optimize stent implantation in select patients.
Discussant Lorenz Räber, MD PhD (Bern University Hospital, Switzerland), noted that one reason the subanalysis is important is because the evidence to support the use of OCT in ACS is limited.
However, OCCUPI wasn’t solely focused on ACS patients, so one major limitation is that there was no specific guidance for operators on how to deal with things like lipid-rich plaque and protruding atherothrombotic material.
“I think what we don't know today is really whether imaging guidance is helpful in lesions that carry a certain lipid and thrombus burden,” Räber added.
In a press conference prior to the presentation, Thomas Cuisset, MD (La Timone Hospital Marseille, France), noted that South Korean investigators have contributed greatly to the accumulating evidence showing the benefit of OCT imaging in complex lesions because uptake of the technology is so high in their country. Training physicians in the use of OCT-guided imaging as well as efforts to get reimbursement are still hurdles to its routine use elsewhere.
In the United States, OCT during PCI has been slowly increasing, with data from the VA Clinical Assessment Reporting and Tracking (CART) program showing that it climbed from 12.3% in 2010 to 43.1% in 2022. But that analysis also showed wide variation, with median usage of 33.5% of all PCIs at the hospital level and 32.4% at the physician level in 2022.
To TCTMD, Kim said an analysis looking at the impact of operator experience in OCCUPI on outcomes is planned. One prior Korean registry study, he noted, suggested that the use of IVUS guidance in complex PCI procedures is of particular benefit for less experienced operators, and it remains to be seen if the same may be true of OCT guidance.
OCCUPI Subanalysis
The trial enrolled patients between January 2019 and September 2022 at 20 centers in South Korea, 49.3% of whom had ACS. Within that group, 412 patients (mean age 62.5 years; 18% female) were randomly assigned to OCT-guided PCI and 378 to angiography-guided PCI. Presentations were unstable angina in 60% of the OCT group and 57% of the angiography group; NSTEMI in 28.6% and 27.8%; and STEMI in 11.2% and 15.3%.
Approximately half of patients had diabetes, one-quarter were current smokers, and prior PCI had been performed in 19.7% of those in the OCT-guided group and in 16.4% of those in the angiography-guided group.
The investigators encouraged operators to use OCT to optimize stent implantation and meet optimization criteria for edge dissection, stent expansion, and stent apposition.
Compared with the angiography-guided group, the OCT group had larger stent diameters, greater maximal inflation pressures, and more frequent use of high-pressure balloon postdilatation. However, in the OCT group procedures were longer and required more contrast volume use than in the angiography group (P < 0.001).
The minimal lumen diameter postprocedure was larger in the OCT group than in the angiography group (2.78 mm vs 2.62 mm) and diameter stenosis was reduced (11.1% vs 14.0%; P < 0.001 for both comparisons).
There were no cardiac deaths in the OCT-guided group compared with three in the angiography-guided group. Rates of MI were 3.6% versus 6.9%, respectively (P = 0.04), and rates of TVR were 1.9% and 4.0% (P = 0.09).
In a post hoc analysis, the primary composite endpoint of cardiac death, MI, or stent thrombosis was less common with OCT compared with angiography (3.6% vs 7.1%; P = 0.029) as was the composite of cardiac death, spontaneous MI, ST, or TVR (2.2% vs 4.8%; P = 0.047).
Räber pointed out that for the primary endpoint there was an early separation of the curves between the OCT- and angiography-guided groups in the ACS analysis that has not been observed previously for IVUS or OCT in studies such as RENOVATE-COMPLEX-PCI. The result also differed from the main OCCUPI trial when those with chronic coronary syndromes (CCS) were included.
Among ACS patients, this early separation was driven by a higher rate of periprocedural MI in the angiography-guided group (4.8% vs 2.7% in the OCT-guided group). In contrast, the CCS patients had rates of periprocedural MI that were higher with OCT than with angiography (2.8% vs 0.9%).
“I think this is something which we do need to understand from a mechanistic standpoint what the potential underlying reason could be,” he said.
L.A. McKeown is a Senior Medical Journalist for TCTMD, the Section Editor of CV Team Forum, and Senior Medical…
Read Full BioSources
Kim B-K. Optical coherence tomography-guided PCI in acute coronary syndrome patients with complex lesions: a subgroup analysis of the randomized OCCUPI trial. Presented at: EuroPCR 2025. May 22, 2025. Paris, France.
Disclosures
- Kim reports grants/research support from Abbott, Medtronic, Biotronik, MicroPort, Boston Scientific, and Genoss; and honoraria/consultant fees from Daiichi Sankyo and Asahi Intecc.




Comments