RAFT-AF: No Benefit of AF Ablation for Heart Failure Patients
The trial was stopped early for futility and missed its primary endpoint, but secondary outcomes point to potential gains.
Ablation-based rhythm control was no better than rate control at reducing mortality or heart failure (HF) events in patients with atrial fibrillation (AF) and heart failure (HF), although there were hints of benefit in the RAFT-AF trial, which was stopped early due to futility.
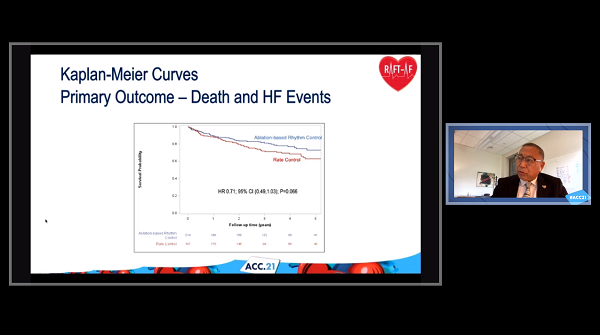
Through a mean follow-up of about 3.1 years, the rate of death/HF events was 23.4% with ablation-based therapy and 32.5% with rate control, a difference that did not reach statistical significance (HR 0.71; 95% CI 0.49-1.03).
There was a suggestion that outcomes were improved with ablation in patients with an LVEF of 45% or less (HR 0.63; 95% CI 0.39-1.02), although LV function was not found to significantly modify the treatment effect (P = 0.397 for interaction).
However, secondary outcomes pointed to improvements in LVEF, 6-minute walk distance, and quality of life, as well as a greater drop in NT-proBNP, in the ablation arm, with no difference in overall serious adverse events compared with rate control, Anthony Tang, MD (Western University, London, Canada), reported Monday during the virtual American College of Cardiology 2021 Scientific Session.
Interpretation of the results is complicated by the fact that the trial was stopped early after only about two-thirds of the planned number of patients were recruited, a decision made on the basis of lower-than-expected enrollment and event rates, and perceived futility at an interim analysis.
“One interpretation of the results is that there is no difference between the two study groups on mortality and heart failure events. An alternate interpretation is that there is a benefit,” he said, highlighting the lower-than-planned patient numbers. “In addition, there’s a time delay between treatment [and when there would be] effects on mortality and heart failure events. And there appears to be a differential effect of ablation-based rhythm control over rate control between patients with LVEF less than or equal to 45% and those greater than 45%.”
Referring to the suggestions of improved outcomes with the ablation-based approach on the primary and secondary outcomes at a press briefing, Tang said “one can probably say this is of clinical significance,” especially in patients with low LVEF.
Rachel Lampert, MD (Yale School of Medicine, New Haven, CT), discussing the results at the briefing, said “RAFT-AF is now joining a growing number of other studies which are suggesting what most of us electrophysiologists have felt in their gut—that sinus rhythm can only be a good thing if only we can achieve it without the [proarrhythmic] and other adverse effects of antiarrhythmic medications.”
She acknowledged that the primary outcome was not met but said the trial, along with others like CASTE-AF and EAST-AFNET 4, suggests that rhythm control achieved using ablation leads to better outcomes versus rate control.
And Lampert put the focus on the gains in quality of life with the ablation-based approach, noting that patients were outraged when CABANA—which also demonstrated quality-of-life improvements in the ablation arm—was being referred to as a negative trial. “In our era of patient-centered care, I think that’s an important message,” she said.
The RAFT-AF Trial
The trial results address a question asked in several other studies before, culminating in a 2018 meta-analysis showing that catheter ablation of AF was associated with lower rates of all-cause mortality and HF hospitalizations, along with improvements in LV function, functional capacity, and quality of life, compared with medications for rhythm or rate control in patients with heart failure. The largest trial in that analysis, with 398 patients, was CASTLE-AF, which demonstrated a lower rate of all-cause death/hospitalization for worsening heart failure with ablation versus medical therapy. A subgroup analysis of the CABANA trial also supported the benefits of ablation in patients with heart failure, most of whom had preserved ejection fraction.
Based on accumulated data, the most-recent update to the US AF guidelines introduced a new class IIb recommendation indicating that catheter ablation may be reasonable in selected patients with symptomatic AF and heart failure with reduced LVEF.
But trials continue, and RAFT-AF, conducted at 21 centers in Canada, Sweden, Brazil, and Taiwan, is the latest to report results. Ablation-based rhythm control involved one or more ablations for AF supported by antiarrhythmic drugs for AF recurrences. Rate control involved use of atrioventricular nodal blockers with or without ablation and biventricular pacing to achieve a resting heart rate of 80 bpm or less and a heart rate of 110 bpm or less after a 6-minute walk test. Crossover between groups was minimal.
Ultimately, the trial included 411 patients out of the planned 600 (mean age roughly 66 years; 74% men) with NYHA class II/III heart failure, elevated NT-proBNP, and a high burden of AF; LVEF was 45% or less for 58%.
The percentage of patients in atrial fibrillation or flutter at baseline was 80.4% in the ablation-based arm and 87.3% in the rate control arm. By 6 months, the rate had dropped in the former arm and remained roughly the same in the latter (14.2% vs 84.8%). That difference remained relatively consistent through 5 years of follow-up.
This did not, however, translate into a significant difference in the rate of all-cause mortality or HF events, either in the overall trial cohort or in the subgroups defined by LVEF at baseline.
Looking at secondary outcomes, ablation-based therapy was associated with significantly greater gains in quality of life assessed using the Minnesota Living With Heart Failure and AF Effect on Quality of Life questionnaires, in 6-minute walk distance, and in LVEF. In addition, there was a significantly greater fall in NT-proBNP levels in the ablation group. All of these effects were greater in patients with reduced versus preserved ejection fraction.
There was no difference in serious adverse events between ablation-based rhythm control and rate control (47.7% vs 50.3%; P = 0.5997). Ablation-related serious events included one atrioesophageal fistula resulting in death, six pericardial effusions requiring drainage, eight major bleeds, and five minor bleeds, Tang reported. He noted at the press briefing that the observed complications are similar to what has been previously seen in real-world data.
Next Steps
Addressing the complication rates, Anthony Tang, MD (Western University, London, Canada), who co-chaired the press briefing, noted that patients with heart failure are typically higher risk than the usual patients undergoing catheter ablation for AF. “That being said, the trade-off, I think, is still worth it because the cumulative complication rates are not really that much off” from other data, he commented.
Discussing the premature termination of enrollment in RAFT-AF and the lower-than-planned patient numbers results after Tang’s presentation, Christine Albert, MD (Smidt Heart Institute at Cedars-Sinai, Los Angeles, CA), suggested that the results may have been different with a larger sample size and longer follow-up.
“We need to wait to see sometimes the benefit of maintaining sinus rhythm, and we saw that with [EAST-AFNET 4], and so when we think about our trials and powering our trials we have to probably consider that,” Albert said. RAFT-AF was designed to be able to show a 30% relative risk reduction in the primary outcome, and that that is roughly what was shown, she pointed out. “So if you had had more patients in it, probably you would have had a positive study. We don’t know that for sure, but I think we have to keep that in consideration when we interpret these findings.”
For Albert, the results should not be interpreted to mean that catheter ablation is not useful in patients with heart failure and preserved ejection fraction. Tang, too, agreed that further studies are warranted in this particular population.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Tang A. A randomized ablation-based atrial fibrillation rhythm control versus rate control trial in patients with heart failure and high burden of atrial fibrillation: RAFT-AF. Presented at: ACC 2021. May 17, 2021.
Disclosures
- RAFT-AF is funded by the Canadian Institutes of Health Research.
- Tang reports research support from Abbott and Medtronic





Comments