Registry Shows Watchman FLX Beating First-Gen Device for Early LAAO Outcomes
This lowers the risk calculus of LAA occlusion, as well as barriers to referral of patients for the procedure, James Freeman says.

SAN FRANCISCO, CA—The redesigned Watchman FLX device (Boston Scientific) provides safer left atrial appendage occlusion (LAAO) in patients with atrial fibrillation compared with the first-generation Watchman 2.5 device, a large registry study shows.
A composite of in-hospital major adverse events occurred at a rate of 1.35% with Watchman FLX and 2.40% with the older device, a difference that remained significant after multivariable adjustment (OR 0.57; 95% CI 0.50-0.65).
That was driven, reported James Freeman, MD (Yale School of Medicine, New Haven, CT), here at Heart Rhythm 2022, by a “marked decrease” in pericardial effusion requiring intervention (0.42% vs 1.23%), with significantly lower rates of death, device embolization, cardiac arrest, and major bleeding as well.
Implant, device, and procedural success rates were slightly higher with the Watchman FLX, which was also associated with procedures that were about 4 minutes shorter on average.
“With the device redesign, we’ve improved the safety profile of the procedure substantially,” Freeman told TCTMD.
That doesn’t necessarily change who is offered LAAO, but it may affect who is referred for the procedure by easing concerns about the associated risks in older, sometimes frail patients, he said. “Because the risk calculus has changed pretty dramatically for this device, . . . I’m hopeful that it will continue to lower the barrier for referral to us.”
A Watchman Redesign
The first-generation Watchman 2.5 device was approved by the US Food and Drug Administration in April 2015, although the device had been used in Europe for several years before that. More than 5 years later, in July 2020, the FDA approved the next-generation Watchman FLX.
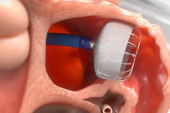
The newer device comes with an additional row of anchors and expanded mesh coating—which may lessen risks of device embolization and device-related thrombus, respectively—along with additional struts, which may improve how it conforms to the LAA. But the biggest change, according to Freeman, was the closing of the end of the device: the Watchman 2.5 had an open end, which carried a greater risk of perforation. The closed end allows for the delivery of the Watchman FLX in a ball configuration, which facilitates atraumatic delivery and the ability to reposition the device for optimal positioning. Moreover, the sheath doesn’t have to be placed as far into the appendage, Freeman noted.
With the device redesign, we’ve improved the safety profile of the procedure substantially. James Freeman
To assess the impact of the changes on early outcomes after the procedure, Freeman and colleagues turned to the LAAO Registry, part of the American College of Cardiology’s National Cardiovascular Data Registry. At each of the 611 sites that implanted the Watchman FLX, an equal number of Watchman 2.5 procedures performed immediately before the switch to the newer device were included in the analysis, leading to an equal number of patients in each study group—27,103 treated with the Watchman FLX and 27,103 treated with the Watchman 2.5 (mean age 76 years; 59% men). In that way, Freeman said, each center acted as its own control, with no changes in indications for the procedure or operators.
The primary outcome of in-hospital major adverse events included death, cardiac arrest, stroke, TIA, intracranial hemorrhage, systemic embolism, major bleeding, major vascular complications, MI, pericardial effusion requiring intervention, and device embolization. A significant difference favoring the Watchman FLX was seen overall and for the following events:
- Death (0.12% vs 0.21%)
- Pericardial effusion requiring intervention (0.42% vs 1.23%)
- Device embolization (0.02% vs 0.06%)
- Cardiac arrest (0.13% vs 0.24%)
- Major bleeding (1.08% vs 2.05%)
The other components of the composite outcome—which wouldn’t necessarily be expected to be affected by the device redesign, Freeman said—occurred at similar rates in the two groups. “I think this is really reassuring when you’re looking at an observational study, because what we think this means is that our findings were not secondary to residual confounding, to differences in the baseline characteristics,” he said. “The findings were really due to the difference in the devices.”
The researchers also examined procedural variables, finding that use of the Watchman FLX was associated with slightly higher rates of implant success (97.8% vs 96.8%), device success (97.4% vs 96.6%), and procedural success (96.1% vs 94.6%), as well as a slightly shorter procedure duration (mean 83.0 vs 86.8 min; P < 0.001 for all).
Large peridevice leaks (> 5 mm) were infrequent overall, although there was a numerically lower rate with the Watchman FLX (0.03% vs 0.06%; P = 0.234).
Overall, the findings were similar in a propensity-matched analysis.
‘Pretty Extraordinary’ Findings
Discussing the results after Freeman’s presentation, Vivek Reddy, MD (Icahn School of Medicine at Mount Sinai, New York, NY), said the study provides very important data, noting that the types of patients who received LAAO fit the expected profile based on the initial trials and FDA approval.
Regarding the observational study design, Reddy said the results are valid for three reasons: the study was comprehensive, there is unlikely to be an issue with a learning curve between the Watchman 2.5 and FLX periods, and the findings of the unadjusted and adjusted analyses were similar. Because events like MI and cardiac arrest did not differ between groups, that “gives us additional confidence that there were not residual confounders that were not adjusted for,” Reddy said.
Moreover, he said the reduction in major adverse events with the newer device was “pretty extraordinary when you think about the number of operators that are performing this procedure around the country,” adding that the effect on tamponade was impressive.
Reddy said that he’d like to see what happens regarding outcomes over the longer term. Prior research has shown that peridevice leaks are less frequent with the Watchman FLX than with the first-generation device, he noted. “The question is: will that actually translate to better clinical outcomes? There’s emerging data that when we don’t have leak we may have extremely low ischemic stroke rates, and I’d like to see what happens in this registry.”
Freeman acknowledged that the current study is limited in that it didn’t assess postdischarge events, noting that pericardial effusion, for instance, is known to occur after patients leave the hospital. That will be looked at in a future study, he said.
However, he told TCTMD, “if we conjecture that leak closure is better, that we’re minimizing leaks, particularly some of the larger leaks, I think that could have some downstream consequences in terms of thromboembolism.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full BioSources
Freeman JV. Safety and acute procedural outcomes of LAAO with the first-generation Watchman and next-generation Watchman FLX devices. Presented at: HRS 2022. May 1, 2022. San Francisco, CA.
Disclosures
- The study was funded by grants from the National Heart, Lung, and Blood Institute, with partial funding from Boston Scientific.
- Freeman reports receiving research funding/salary support from the National Heart, Lung, and Blood Institute and the American College of Cardiology Foundation; serving on advisory boards or consulting for Medtronic, Boston Scientific, Biosense Webster, and PaceMate; and having equity in PaceMate.
- Reddy reports receiving honoraria or speaking/consulting fees from Abbott, and CoreMap; having stock options from Acutus Medical, Biosig Technologies, Aquaheart, Autonomix, Axon, BackBeat, Circa Scientific, Corvia Medical, AFTX, Farapulse, FIRE1, Luxcath, Medlumics, NewPace Ltd, Surecor, VytronUS, Valcare, CardiaCare, Ablacon, Dinova, Kardium, HRT, Intershunt, AtaCor Medical, Sirona Medical Technologies, and Corisma; and owning stocks from Affera, EpiEP, CardioNXT, Manual Surgical Sciences, VIZARA, and Restore Medical.




Comments