Sizing Mismatch a Problem for Balloon-Expandable Valves in Small Annuli TAVI
Worryingly, mismatch at 1 year also predicted 3-year all-cause death, spurring calls for RCTs in this setting.

BOSTON, MA—Compared with balloon-expandable bioprosthetic aortic valves, self-expanding devices show superior hemodynamic performance at 1 year in patients with small annuli undergoing TAVI, according to new registry data. Moreover, use of a balloon-expandable valve was associated with moderate or severe patient-prosthesis mismatch (PPM) at 1 year, which also was an independent predictor of all-cause mortality at 3 years.
The observational results should be interpreted with caution, said Walid Ben-Ali, MD, PhD (Montreal Heart Institute, Canada), who presented the data today at TCT 2022, but “basically, when you have severe PPM at 1 year, you have a twofold relative hazard for all-cause mortality at 3 years.”
The findings aren’t yet enough to suggest that all patients with small annuli should be treated with self-expanding valves, though, several experts said.
“I think it’s very difficult when you have these propensity-matched analyses to really make definitive decisions on that basis,” said Alexandra Lansky, MD (Yale University School of Medicine, New Haven, CT), during a discussion in the late-breaking clinical trial session. “It’s important. I do think it needs to be validated. You need long-term follow-up. You need matched populations, et cetera. So I think validating this in a prospective trial is important.”
Likewise, Susheel Kodali, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, NY), cautioned the audience that it’s easy to be seduced by large, observational data sets and the signals they can suggest, “especially when you are dealing with devices that are so different.” He emphasized that valve types are chosen for a variety of reasons including lifetime management, need for pacemaker, and coronary access.
“We all agree we want the largest valve area, and we struggle with how to assess it, what the valve area truly is, and we make decisions based on a lot of factors,” Kodali continued. “This is really enticing, but we have to wait for the data to answer the question that was asked: will it impact . . . device choice?”
The panelists agreed that the ongoing SMART trial will hopefully give more definitive answers in this space.
FRANCE-TAVI Results
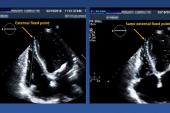
For the study, Ben-Ali and colleagues included data on 1,195 patients from the FRANCE-TAVI registry with small aortic annuli—defined as a diameter ≤ 23 mm or an indexed diameter ≤ 12 mm/m2 measured on CT—who underwent TAVI with either a supra-annular self-expanding valve (Evolut R/Pro; Medtronic) or a balloon-expandable device (Sapien 3; Edwards Lifesciences).
The researchers conducted propensity matching through two methods. The first (n = 928) used 10 anatomical and clinical variables to create a propensity score and patients were matched in a 1:3 fashion depending on whether they were treated with a self-expanding or balloon-expandable device. The second (n = 1,195) used the propensity score to generate an inverse probability treatment weighting (IPTW) as a sensitivity analysis.
After matching, both cohorts were comparable in terms of demographics and basic echocardiographic and CT data as well as procedural and postprocedural results. However, the hemodynamic performance was significantly better with the supra-annular self-expanding valves compared with balloon-expandable devices in terms of lower mean gradient and larger index effective orifice area at discharge, 30 days, and 1 year (P < 0.001 for all).
The rates of moderate or severe PPM at 1 year were significantly higher in the balloon expandable versus self-expanding valve groups before and after matching (P < 0.001 for all). Female sex (HR 1.59; 95% CI 1.14-2.17), small annuli (HR 2.38 per 1-mm decrease; 95% CI 1.27-4.55), postprocedural mean gradient (HR 1.04 per 1-mm Hg increase; 95% CI 1.01-1.06), and valve type (HR 2.94; 95% CI 1.79-4.76) were all found to be independent predictors of moderate to severe PPM at 1 year in both matching strategies.
“Patients treated with balloon expandable valves have threefold relative hazard to develop a moderate to severe PPM at 1 year,” Ben-Ali said.
Additionally, severe PPM at 1 year (HR 2.01; 95% CI 1.02-3.95), length of index hospitalization (HR 1.05 per 1-day increase; 95% CI 1.01-1.09), major bleeding (HR 2.86; 95% CI 1.07-7.66), and atrial fibrillation (HR 3.46; 95% CI 2.08-5.74) were all found to be independent predictors of 3-year mortality in the first matching strategy. Using the IPTW strategy, valve type (HR 1.93; 95% CI 1.2-3.11) and annulus size (HR 1.23 per 1-mm decrease; 95% CI 1.06-1.41) also were predictors of 3-year all-cause mortality.
‘Power of Large Registries’
During the discussion, Bernard Prendergast, MD (St Thomas' Hospital, London, England), said that the assessment of PPM is well known to be complicated “and achieving those measurements in the context of a national registry without a core lab is a very difficult call. That said,” he continued, “I think this study and [the TEER SHOCK registry presented in the same session] have shown the power of large registries to yield data which guide the field. And while patient-prosthesis mismatch may not be so important in very elderly patients, many of whom are in this registry, we know from the surgical data that PPM is important in younger patients.”
Prendergast added that “these data are a call to our colleagues in industry and the engineers who design new valves to think about the needs of patients with small annuli as we move into the fourth and fifth generations of TAVR devices.”
These data are a call to our colleagues in industry and the engineers who design new valves to think about the needs of patients with small annuli as we move into the fourth and fifth generations of TAVR devices. Bernard Prendergast
In a press conference, Michael Young, MD (Dartmouth-Hitchcock Medical Center, Lebanon, NH), said he is “cautiously reassured about the findings from this, because in our practice I do think that we're thinking about this very carefully.” He added that some of the surgeons at his institutions are “aggressive about doing root enlargements in the hopes for these small annuli getting a larger surgical prosthetic valve.”
In his practice, Young added, “we've swayed toward a supra-annular design” for patients with small annuli. Many end up with a “gradient of 17-20 mm Hg when they start with a gradient of 40 mm Hg. They feel better, they generally feel well, but you just don't know, number one, durability and then, number two, what their clinical outcomes are going to be.”
Another issue that comes into play when choosing a bioprosthesis relates to lifetime management of the patient, Young said. “That has actually come into discourse in terms of choosing SAVR vs TAVR at this point. Usually when the annulus is small, we’re also looking at the sinuses and sometimes the sinuses can be very small. So you worry about sinus sequestration and boxing the patient in, so to speak, in the next 5-10 years who knows what their coronary options will be.”
Also during the press conference, Robert Cubeddu, MD (NCH Heart Institute, Naples, FL), said that while the data support “what we already kind of know and think, we have to remind ourselves this is a retrospective view with a nonadjudicated core lab definitions of PPM et cetera, which are incredibly important.”
Awaiting SMART Results
The data place added pressure on the SMART trial data, said David J. Cohen, MD (St. Francis Hospital, Roslyn, NY), during the TCT session. “And not of the 1-year results, which are going to be presented first from that trial, but the 5-year results which will give us a sense of whether this really makes a difference for patients, especially patients who are not in the extreme elderly group who may expect to live for 5-10 years,” he clarified. “We need that desperately to really know what is best for that challenging group because the PPM rates here are not trivial.”
In agreement, panelist Anita Asgar, MD (Montreal Heart Institute, Canada), said all of these data will become increasingly important as TAVI moves into lower-risk patients. “Hemodynamics we maybe didn't ignore, but it wasn't perhaps as much of an issue in the elderly population,” she said. “And now with younger patients, we need to take all these things into consideration.”
What will also be important is “understanding how these hemodynamics vary under exercise and stress,” she added.
Session co-moderator Jane Leopold, MD (Brigham and Women’s Hospital, Boston, MA), reiterated this point, saying: “Exercise hemodynamics [are] incredibly important, because the hemodynamics at rest just don't predict what the patient does when the patient gets up and walks out from the hospital.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Ben-Ali W. Transcatheter aortic valve replacement in small aortic annuli: results from the FRANCE-TAVI registry: the Xs-TAVI Trial. Presented at: TCT 2022. September 17, 2022. Boston, MA.
Disclosures
- Ben-Ali reports receiving grant/research support from Edwards Lifesciences, Medtronic, and Fonds de Recherche Santé du Québec.



Comments