Combo of Intravascular Imaging and Physiology for PCI Gains Steam in the US
The dual approach, though rare, was linked to fewer 2-year MACE and lower long-term costs compared with angiography alone.

Dual use of intravascular imaging and invasive physiology, though still rare, rose in the United States over recent years, according to a look at Medicare data spanning from 2016 to 2023. This adjunctive approach, as well as each test when used individually, was linked to fewer 2-year MACE and lower long-term costs compared to angiography alone.
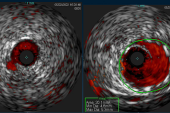
Senior author Eric A. Secemsky, MD (Beth Israel Deaconess Medical Center, Boston, MA), told TCTMD that there’s growing support for the idea that these tools, when used in addition to angiography, provide complementary information. Physiology can be used to identify clinically significant pathology that merits intervention, while “we’ve used intravascular imaging to really guide us during the intervention to make sure we’re doing [it] to the highest quality possible and optimizing our stents,” he explained.
Lead author Frank A. Medina, BA (Beth Israel Deaconess Medical Center and University of Chicago Pritzker School of Medicine, IL), noted that intravascular imaging, in particular, has been on the upswing thanks to its endorsement in the 2018 European and 2021 US revascularization guidelines. As of 2024 and 2025, European and US guidelines gave intravascular imaging a class 1a indication for guiding PCI in chronic and acute coronary syndromes, respectively.
With the current study, which was published in the January 12, 2026, issue of JACC: Cardiovascular Interventions, the researchers sought to gather evidence on the dual use of intravascular imaging and invasive physiology. Much like has been asked for imaging in the past, said Secemsky, “the question right now [for this combo approach] is . . . do we really need it in every case? Should this be the standard approach or is this for specific complex lesion subsets?”
He added: “I think we are better operators if we understand our limitations, and particularly our limitations with angiography alone when we aren’t using these tools. If we can do this in a cost-conscious way, I think that we can make a good case that this should be standard practice.”
Technological advancements in the cath lab are moving in the same direction with devices that by design integrate both intravascular imaging and physiological assessment, he pointed out.
Edward T. Ha, MD, Tatsunori Takahashi, MD, and Yuhei Kobayashi, MD (all from MedStar Washington Hospital Center, Washington, DC; Cedars Sinai-Medical Center, Los Angeles, CA; and NewYork-Presbyterian Brooklyn Methodist Hospital/Weill Cornell Medical College, NY), in an editorial, agree that these “truly integrated platforms” are likely to “streamline cardiac catheterization laboratory flow and achieve cost-effectiveness.”
When used to guide PCI, they can improve lesion selection by considering physiological significance and plaque vulnerability as well as enable better treatment of diffuse/tandem lesions and postprocedural optimization, the editorialists say. “It is imperative that we advocate for and implement these innovations to ensure the provision of precise, secure, and efficacious patient care.”
Medicare Trends
Using Medicare fee-for-service claims, Medina and colleagues tracked trends in intravascular imaging and/or invasive physiology from 2016 to 2023 among 1,958,990 beneficiaries undergoing their first PCI. Across that 7-year period, intravascular imaging was used in 15.1% of PCI cases (98.4% IVUS and 1.6% OCT), invasive physiology in 7.0%, and both modalities in 2.5%.
Intravascular imaging tended to be used more often in the inpatient versus outpatient setting, at larger hospitals and academic medical centers, in urban areas, in communities with higher economic well-being, and in the western and northern US. Dual use followed similar patterns apart from being more common in the outpatient setting. Physiological assessment without intravascular imaging occurred more frequently in the outpatient setting but also at larger hospitals, at academic medical centers, and in the western and northeastern US.
For PCI guidance, intravascular imaging rates rose between 2016 and 2023: from 7.7% to 29.6% for IVUS and from 0.13% to 0.32% for OCT. With physiological assessment, use trended slightly lower over time, while the dual approach to testing increased from 1.0% in 2016 to 4.7% in 2023.
Additionally, the Medicare data on diagnostic angiography showed invasive physiology was used in 6.9% of these cases that didn’t involve PCI, intravascular ultrasound in 1.7%, and both in 0.5%. Physiology in this setting rose from 5.9% in 2016 to 7.4% in 2023 (P = 0.0021).
The researchers analyzed 2-year clinical outcomes for 1,587,532 PCI patients (mean age 75.3 years; 63.9% men; 87.8% white). A little more than half (53.6%) were treated as inpatients, and 60.6% presented with acute coronary syndromes. Dual use and each of the tests individually were linked to lower 2-year rates of MACE and its individual components. For stroke/TIA, rates were reduced with intravascular imaging but not invasive physiology or dual use.
Two-Year Outcomes vs Angiography Alone: Adjusted HR (95% CI)
|
|
Intravascular Imaging |
Invasive Physiology |
Both |
|
MACE |
0.94 (0.93-0.95) |
0.85 (0.84-0.86) |
0.87 (0.85-0.89) |
|
All-Cause Death |
0.90 (0.88-0.91) |
0.84 (0.83-0.86) |
0.84 (0.81-0.87) |
|
MI |
0.94 (0.92-0.96) |
0.91 (0.89-0.93) |
0.86 (0.82-0.90) |
|
Repeat Revascularization |
0.96 (0.93-0.98) |
0.83 (0.81-0.84) |
0.88 (0.85-0.91) |
|
Stroke/TIA |
0.93 (0.90-0.97) |
1.00 (0.96-1.05) |
0.96 (0.88-1.03) |
For cost, the researchers limited their analyses to the 736,510 patients who had outpatient PCI to avoid inadvertently including unrelated expenses, Secemsky said. “Most of our PCIs go home the same day or stay just for overnight observation. [With] inpatient, you get a lot of charges that aren’t related to the intervention,” which makes it tricky to interpret the data.
Both intravascular imaging and dual use, but not invasive physiology, had higher index PCI costs compared with angiography, while provider payments were higher across all three categories of adjunctive assessment. Then, 2 years after PCI, those who had intravascular imaging and/or invasive physiology had lower average costs related to repeat revascularization and hospital readmissions. Provider payments, too, were lower for these endpoints.
We are better operators if we understand our limitations, and particularly our limitations with angiography alone when we aren’t using these tools. Eric Secemsky
Reimbursement challenges are one factor that have held back adjunctive assessment in the United States, Medina pointed out. Their analysis “speaks to potential cost savings not only from improved outcomes associated with these devices . . . but also in terms of optimizing lesion selection,” such that treatment is targeted to more severe cases while unnecessary PCIs are avoided,” he said.
“Future studies are needed to discern the appropriateness and benefits of this combined approach during PCI and to validate its cost-effectiveness,” the authors conclude.
Among the study’s limitations, the editorialists say, is the potential for confounding by indication, something that the researchers took steps to avoid, such as through the falsification endpoints of GI bleeding and hip fracture as well as Cox proportional regression models.
“These comparative studies of real-world evidence are going to always suffer from some aspect of treatment-selection bias. We do our best to overcome that, we acknowledge it,” Secemsky said. In this instance, though, it would make sense that the adjunctive tests are more likely to be employed when operators face more-severe lesions, “so we’d expect that to bias away from showing a benefit if that was the driver,” he commented. “The fact that we still had a treatment benefit with the combined approach is telling.”
Caitlin E. Cox is Executive Editor of TCTMD and Associate Director, Editorial Content at the Cardiovascular Research Foundation. She produces the…
Read Full BioSources
Medina FA, Mosarla RC, Kim JM, et al. Adjunctive imaging and physiology during percutaneous coronary intervention: trends, outcomes, and costs among Medicare beneficiaries. JACC Cardiovasc Interv. 2026;19:15-27.
Ha ET, Takahashi T, Kobayashi Y. Pursuit of state-of-the-art PCI with imaging and physiology. JACC Cardiovasc Interv. 2026;19:28-30.
Disclosures
- Medina is supported by the Sarnoff Cardiovascular Research Foundation.
- Secemsky has received research funding from the National Heart, Lung, and Blood Institute and Philips.
- Kobayashi has received institutional research support from CathWorks and has a consulting agreement with Abbott Vascular.
- Ha and Takahashi report no relevant conflicts of interest.




Comments