COVID-19: TCTMD’s Dispatch for July 2022
We’re curating a list of COVID-19 research and other useful content, and updating it regularly.

Since March 2020, TCTMD reporter Todd Neale has been writing up breaking news and peer-reviewed research related to COVID-19 every weekday. In July 2021, we transitioned to Mondays, Wednesdays, and Fridays. If you have something to share, tell us. All of our COVID-19 coverage can be found on our COVID-19 Hub.
July 28, 2022
The latest numbers from the US Centers for Disease Control and Prevention (CDC) show that the BA.5 Omicron subvariant accounts for about 82% of circulating SARS-CoV-2 in the country, up from about 76% the week before, Reuters reports. The BA.4 subvariant accounted for 13% of circulating virus. “The US Food and Drug Administration has asked vaccine manufacturers to target the two currently dominant subvariants for a potential fall season booster dose,” the story notes.
 Two studies in Science—here and here—have bolstered the idea that SARS-CoV-2 first emerged from the Huanan Seafood Wholesale Market in Wuhan, China, the Los Angeles Times reports. “Though the exact species of animal isn’t yet known, the authors conclude that SARS-CoV-2 was most likely present in animals sold at the market in late 2019, and jumped into human workers or shoppers in at least two separate instances,” the story notes. One researcher said the new data has convinced him “it’s just not plausible that this virus was introduced in any other way than through the wildlife trade at the Huanan market.”
Two studies in Science—here and here—have bolstered the idea that SARS-CoV-2 first emerged from the Huanan Seafood Wholesale Market in Wuhan, China, the Los Angeles Times reports. “Though the exact species of animal isn’t yet known, the authors conclude that SARS-CoV-2 was most likely present in animals sold at the market in late 2019, and jumped into human workers or shoppers in at least two separate instances,” the story notes. One researcher said the new data has convinced him “it’s just not plausible that this virus was introduced in any other way than through the wildlife trade at the Huanan market.”
The antiviral therapies molnupiravir (Lagevrio) and nirmatrelvir-ritonavir (Paxlovid) each likely reduce the risk of death in adult patients with nonsevere COVID-19, with the latter treatment likely being more effective for lowering the risk of hospital admission, according to a systematic review and network meta-analysis in CMAJ. Remdesivir (Veklury) doesn’t appear to influence mortality risk, although it may reduce hospitalizations. CIDRAP News has more.
STAT’s Matthew Herper sums up the White House COVID-19 vaccine summit held Tuesday: “For starters, there was tremendous optimism about the prospects for developing next-generation vaccines. And there were, in fact, glimmers of a tractable path to better products—if Congress will provide billions of dollars to speed things up.” But difficulties remain. “As meeting organizer and White House COVID coordinator Ashish Jha pointed out, the challenge is that the current vaccines are terrific and new vaccines have to be better than terrific.”
 TCTMD has a story on the JAMA research letter previously mentioned in the Dispatch showing that among patients with COVID-19, risks of acute MI and stroke are lower in those who have been fully vaccinated than in those who haven’t received any doses. “A protective effect against COVID-19 and its progression to severe disease is by itself a sufficient reason to get vaccinated,” a study author told TCTMD. “But our findings add an important additional benefit.”
TCTMD has a story on the JAMA research letter previously mentioned in the Dispatch showing that among patients with COVID-19, risks of acute MI and stroke are lower in those who have been fully vaccinated than in those who haven’t received any doses. “A protective effect against COVID-19 and its progression to severe disease is by itself a sufficient reason to get vaccinated,” a study author told TCTMD. “But our findings add an important additional benefit.”
A Nature news story digs into what’s known about how long people infected with SARS-CoV-2 can spread the virus. “Those with SARS-CoV-2 are often advised to isolate for only a few days. But evidence is mounting that some people can continue to pass on the virus for much longer,” David Adams writes, noting that many scientists have pushed back against a shortening of the recommended isolation period by the CDC.
Vaccination appears to provide protection against reinfection after an initial bout of COVID-19, researchers report in JAMA Network Open. Compared with remaining unvaccinated, completing the primary vaccination series after recovery was associated with 47% to 62% protection against reinfection among residents and employees of long-term congregate care facilities and the general population during periods when wild-type, Alpha, and Delta strains of SARS-CoV-2 were circulating.
The vaccine from Pfizer and BioNTech doesn’t increase the risk of myopericarditis in children ages 5 to 11, according to data published in Pediatrics. Out of 208,088 children vaccinated, only one case of myocarditis was identified, indicating a rate similar to the background incidence in that age group. CIDRAP News provides more details.
 An analysis in the BMJ suggests that smell and taste dysfunction may linger over the long term after SARS-CoV-2 infection in more than 15 million and 12 million people, respectively, across the world. Women were less likely than men to recover their sense of smell and taste. “Health leaders, policy makers, and research funders should realize the extraordinary importance of good chemosensory function for the well-being of humans, allocate adequate resources to support chemosensory research, and sustain medical specialists faced with an exceptional number of patients with smell and taste dysfunction,” authors of an accompanying editorial write.
An analysis in the BMJ suggests that smell and taste dysfunction may linger over the long term after SARS-CoV-2 infection in more than 15 million and 12 million people, respectively, across the world. Women were less likely than men to recover their sense of smell and taste. “Health leaders, policy makers, and research funders should realize the extraordinary importance of good chemosensory function for the well-being of humans, allocate adequate resources to support chemosensory research, and sustain medical specialists faced with an exceptional number of patients with smell and taste dysfunction,” authors of an accompanying editorial write.
July 25, 2022
US President Joe Biden, who tested positive for COVID-19 last Thursday, has completed his fourth full day of Paxlovid treatment as of last night and his symptoms have “almost completely resolved,” White House physician Kevin C. O’Connor, DO, reported today. “At this point, he only notes some residual nasal congestion and minimal hoarseness. His pulse, blood pressure, respiratory rate, and temperature remain absolutely normal. His oxygen saturation continues to be excellent on room air. His lungs remain clear.”
 On Tuesday, Biden’s administration is hosting a summit to kick off a new and comprehensive initiative to develop the next generation of COVID-19 vaccines geared towards preventing transmissions and new infections, rather than just reducing deaths and hospitalizations, which is where the current shots have proved their mettle. The event will be livestreamed, but requires registration. STAT has the details on the plan.
On Tuesday, Biden’s administration is hosting a summit to kick off a new and comprehensive initiative to develop the next generation of COVID-19 vaccines geared towards preventing transmissions and new infections, rather than just reducing deaths and hospitalizations, which is where the current shots have proved their mettle. The event will be livestreamed, but requires registration. STAT has the details on the plan.
In the US, Omicron BA.5 now accounts for 78% of cases and infections and new hospitalizations are up, but nationally, death rates are slightly lower, according to numbers from the US Centers for Disease Control and Prevention (CDC). Becker’s Hospital Review has a summary.
One-third of older age care homes in Australia are currently seeing virus outbreaks, with that number expected to climb to two-thirds in the next few weeks, the Guardian reports, adding: “The Aged and Community Care Providers Association said 6,000 residents and 3,400 staff were infected in 1,013 facilities as of Thursday.”
New Zealand, too, the longtime poster child for pandemic protections, is currently seeing record numbers of COVID-19 deaths, due largely to the highly transmissible BA.5 Omicron variant. “Deaths from the virus reached 151 in the 7 days to July 16, compared with 115 in the worst week of the previous wave, in March, according to Health Ministry data,” Reuters reports. To put that in perspective, however, fewer than 2,000 people have died of COVID-19 over the entire pandemic in New Zealand, which has a population of 5.1 million, according to the New York Times tracker. By contrast, in the state of South Carolina—with a similarly sized population—more than 18,000 people have died.
Full vaccination against COVID-19 was associated with a reduced risk of acute MI and ischemic stroke after COVID-19 infection, Korean investigators report in JAMA today. Check back for TCTMD’s full coverage.
Researchers say they may have found a potential route through which the SARS-CoV-2 spike protein damages the heart. In a study slated for presentation today at the American Heart Association’s Basic Cardiovascular Sciences Scientific Sessions 2022, investigators compared the SARS-CoV-2 spike protein to that of another coronavirus, HCoV-NL63, and demonstrated that the former activates specific immune reactions, including an inflammatory response in heart muscle cells, not seen with the NL63 spike protein. Importantly, say the authors, their work provides evidence that the SARS-CoV-2 spike protein does not need ACE2 to injure the heart but rather presents “a novel, ACE2-independent pathological role” for this protein. A press release has more.
 Loss of smell, hair loss, ejaculation difficulty, and reduced libido are the most common post-COVID conditions lasting beyond 12 weeks, a retrospective, matched cohort study of nonhospitalized UK adults indicates. Risk factors for long COVID in this analysis included female sex, belonging to an ethnic minority, socioeconomic deprivation, smoking, obesity, and a wide range of comorbidities, most notably COPD, benign prostatic hyperplasia, fibromyalgia, anxiety, erectile dysfunction, depression, migraine, multiple sclerosis, celiac disease, and learning disability. The risk of developing long COVID tends to increase at younger ages, the authors conclude in Nature Medicine.
Loss of smell, hair loss, ejaculation difficulty, and reduced libido are the most common post-COVID conditions lasting beyond 12 weeks, a retrospective, matched cohort study of nonhospitalized UK adults indicates. Risk factors for long COVID in this analysis included female sex, belonging to an ethnic minority, socioeconomic deprivation, smoking, obesity, and a wide range of comorbidities, most notably COPD, benign prostatic hyperplasia, fibromyalgia, anxiety, erectile dysfunction, depression, migraine, multiple sclerosis, celiac disease, and learning disability. The risk of developing long COVID tends to increase at younger ages, the authors conclude in Nature Medicine.
Children, too, are at risk for post-COVID conditions, researchers report in JAMA Network Open. Nearly 6% of children who tested positive for COVID-19 during an emergency room visit at one of 36 emergency departments in eight countries during the first year of the pandemic reported a post-COVID condition over the next 90 days. The rate was higher among hospitalized children, reaching nearly 10%, and the most common post-COVID condition symptoms were respiratory (2%) and systemic (1.8%), with fatigue or weakness as the most reported individual symptoms. “Risk factors for reporting post-COVID conditions included the number of acute symptoms, length of hospitalization, and older age,” the authors say.
July 21, 2022
President Biden is fully vaccinated, twice boosted, and experiencing mild symptoms following a positive COVID-19 test. Read a letter from Dr. Kevin O’Connor, Physician to the President: pic.twitter.com/Vq9iuAfBdO
— The White House (@WhiteHouse) July 21, 2022
United States President Joe Biden has tested positive for COVID-19, the White House announced this morning. “He is fully vaccinated and twice boosted and experiencing very mild symptoms,” a statement reads. “He has begun taking Paxlovid. Consistent with CDC guidelines, he will isolate at the White House and will continue to carry out all of his duties fully during that time.” The White House has said it will provide daily updates on the 79-year-old president’s health, noting that he tested negative on a Tuesday test. Symptoms began with a dry cough, runny nose, and fatigue last night, according to the president’s physician.
More-viscous blood, which increases the propensity for clotting, is a sign that patients hospitalized for COVID-19 are more likely to do worse over the short term, according to data from a New York City health system. The findings, published in the Journal of the American College of Cardiology, may have critical implications for patient care, investigators say. “If you have elevated blood viscosity, high shear or low shear, those individuals are in an accelerated pathway for death,” senior author Robert Rosenson, MD, told TCTMD’s Todd Neale. “Those individuals should be appropriately hydrated to decrease the plasma viscosity, they should receive high-intensity glucocorticoids to decrease the inflammatory response, and they should be monitored much more closely because of the prognostic significance of an elevated blood viscosity,” he advised.
The vaccine rollout in the UK, starting in December 2020, likely averted infections for one out of every ten patient-facing healthcare workers during the pandemic’s second wave, research in the BMJ estimates, preventing 69% of staff absences. What’s more, the odds of catching COVID-19 increased by 2% every day that a health worker went without getting vaccinated, authors say.
A second BMJ study, looking at the effectiveness of the Pfizer/BioNTech and Oxford/AstraZeneca vaccines, indicates that both agents helped prevent infection and were equally protective in 317,341 English health and social care workers vaccinated in the first 2 months of 2021. “Together, these [two BMJ studies] provide essential insights into SARS-CoV-2 infection in health and social care workers that can be used to guide further infection prevention and control measures,” a press release notes.
Waning efficacy of vaccines has been a hot topic for months, but a new BMJ analysis of more than 7 million UK adults, comparing those who had two doses of the Pfizer/BioNTech or Oxford/AstraZeneca vaccines to those who remained unvaccinated, indicates that the double doses provided strong protection against COVID-19 hospital admission, COVID-19 death, or a positive SARS-CoV-2 test out to 6 months. “Although we found that protection against severe COVID-19 provided by two doses of vaccine wanes over time, the very high initial protection means that, despite waning, protection remains high 6 months after the second dose,” lead author Elsie Horne, PhD, said in a press statement. “This finding was consistent across all adults, including older adults and those who are at risk of severe COVID-19.”
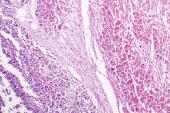
 Myocarditis following COVID-19 infection has increased hospitalizations and deaths among people who fall ill with the virus, but as research in the Journal of the American College of Cardiology makes clear, not all myocarditis is the same. As TCTMD’s Michael O’Riordan reports, researchers found that COVID-19-related myocarditis in adult patients who did not have evidence of multisystem inflammatory syndrome (MIS-A) progressed quickly toward refractory cardiogenic shock and had poorer outcomes. By contrast, patients who also met the criteria for MIS-A presented with different biomarkers of illness, had a less-serious clinical course, and responded to different treatments.
Myocarditis following COVID-19 infection has increased hospitalizations and deaths among people who fall ill with the virus, but as research in the Journal of the American College of Cardiology makes clear, not all myocarditis is the same. As TCTMD’s Michael O’Riordan reports, researchers found that COVID-19-related myocarditis in adult patients who did not have evidence of multisystem inflammatory syndrome (MIS-A) progressed quickly toward refractory cardiogenic shock and had poorer outcomes. By contrast, patients who also met the criteria for MIS-A presented with different biomarkers of illness, had a less-serious clinical course, and responded to different treatments.
Text messages with vaccine reminders and appointment times have a role to play in upping adherence to vaccine schedules, but the efficacy of the approach wanes with time, research in JAMA Network Open implies. In a randomized study of 2,000 subjects, those who received a text message reminder and suggested appointment time were more likely to get vaccinated within 2 weeks. By week 4, however, there was no difference in overall vaccination adherence required by workplace vaccination policies between participants who got text reminders and those who did not.
In Singapore, mRNA vaccination in children aged 5 to 11 effectively reduced the risk of SARS-CoV-2 infection, as well as COVID-19-related hospitalizations, during the early Omicron wave, researchers report in the New England Journal of Medicine. Among children who’d received a single dose, vaccine effectiveness was 24.3% against PCR-confirmed infection and 42.3% against hospitalization. Fully vaccinated children saw vaccine effectiveness rise to 36.8% and 82.7% for both outcomes, respectively.
Also in the NEJM, a research letter offers some insights into the efficacy of different monocloncal antibodies and antiviral drugs against newer Omicron variants. According to live-virus focus reduction neutralization testing, the three small-molecule antiviral drugs remdesivir, molnupiravir, and nirmatrelvir “may have therapeutic value against the sublineages BA.2.12.1, BA.4, and BA.5,” the authors write. Bebtelovimab appears to hold up against BA.2.12.1, BA.4, and BA.5, while combination therapy with casirivimab and imdevimab, and with tixagevimab and cilgavimab, as well as the stand-alone sotrovimab, appear to be less effective against these strains. “Our findings show that the selection of monoclonal antibodies to treat patients who are infected with Omicron variants should be carefully considered,” researchers conclude.
 TCTMD’s coverage of the “living evidence syntheses and review” covering the knowns and unknowns of vaccine-linked myocarditis is now live. As noted in Monday’s Dispatch, the document was published in the BMJ last week; it is also the focus of an upcoming interview on the Heart Sounds podcast.
TCTMD’s coverage of the “living evidence syntheses and review” covering the knowns and unknowns of vaccine-linked myocarditis is now live. As noted in Monday’s Dispatch, the document was published in the BMJ last week; it is also the focus of an upcoming interview on the Heart Sounds podcast.
COVID-19 travel restrictions continue to wane, the New York Times reports, including those of nations and territories where bans and requirements were among the strictest in the world. These are happening even as case counts climb in many countries, due to highly transmissible Omicron variants. “The Centers for Disease Control and Prevention provides a four-tier ranking for coronavirus risk in other countries, with the highest ‘Level 4’ ranking for countries that have ‘special circumstances,’ including the threat of collapse to the healthcare infrastructure and extremely high case counts,” the Times notes. “The CDC’s list currently has no countries so designated.”
July 18, 2022
Editors-in-chief of the BMJ and HSJ are calling on public health leadership in the National Health Service (NHS) to stay “honest” about the threat still posed by the COVID-19 pandemic. “The NHS is not living with COVID,” they allege in an editorial today. “It’s dying from it.” Hospitalizations in the first 6 months of the year for people testing positive for COVID-19 have averaged just over 9,000 per week, they note, compared with an average of < 6,000 in 2021 and < 7,000 in 2020. “How is the government responding to this crisis? Largely by pretending it is not happening or implying it is all under control. . . . [T]he government must stop gaslighting the public and be honest about the threat the pandemic still poses to them and the NHS.”
 The Omicron BA.5 wave is still rising in at least 40 US states, leading to a 20% increase in hospitalizations, but unlike during prior surges, something is different this time around, the New York Times reports. “Public health officials are sounding only quiet warnings amid a picture that they hope has been changed by vaccines, treatments, and rising immunity.” The article quotes Allison Arwady, the commissioner of the Chicago health department saying, “I feel strongly that you can’t just kind of cry wolf all the time. . . . I want to save the requirements around masks or updating vaccine requirements for when there’s a significant change.”
The Omicron BA.5 wave is still rising in at least 40 US states, leading to a 20% increase in hospitalizations, but unlike during prior surges, something is different this time around, the New York Times reports. “Public health officials are sounding only quiet warnings amid a picture that they hope has been changed by vaccines, treatments, and rising immunity.” The article quotes Allison Arwady, the commissioner of the Chicago health department saying, “I feel strongly that you can’t just kind of cry wolf all the time. . . . I want to save the requirements around masks or updating vaccine requirements for when there’s a significant change.”
A “living evidence synthesis and review” spanning 46 studies and published in the BMJ last week affirms what other papers have found regarding the risk of myocarditis and mRNA vaccination—namely, that risk is highest in adolescent and young adult men, and that “use of a Pfizer vaccine over a Moderna vaccine and waiting for more than 30 days between doses might be preferred for this population.” Authors also found that the clinical course of myocarditis “appeared to be benign” in the vast majority of cases, and that myocarditis was “very rare” in children ages 5 to 11.
The US Food and Drug Administration (FDA) has updated its online resource for SARS-CoV-2 viral mutations and their impact on COVID-19 tests. The web page includes a list of antigen tests expected to fail to successfully detect infections caused by the Omicron variants, as well as those that previously were listed as “expected to fail” that have since been modified to fix this issue.
Systemic reactions are more common when COVID-19 mRNA booster doses and seasonal influenza vaccines are administered in tandem, as compared with a COVID-19 booster alone, researchers conclude in JAMA Network Open. “In both groups, most reactions reported in the week following vaccination were generally mild,” the authors write. “These results may help better characterize the outcomes associated with simultaneously administered COVID-19 mRNA booster and influenza vaccines in the US population.”
 In immunocompromised individuals ages 12 and older, fewer serious adverse events were reported to two US programs for tracking vaccine side effects following a second booster shot than after the first, researchers report in Morbidity and Mortality Weekly Report. The analysis tracked reports made to the v-safe voluntary, smartphone-based US active safety surveillance system and the Vaccine Adverse Event Reporting System (VAERS) passive surveillance system for all vaccine-associated adverse events co-managed by the US Centers for Disease Control and Prevention and the FDA. Most local and systemic reactions were minor and similar to those seen with dose three, authors say. A total of 145 reports of reactions were made to VAERS after 518,113 persons ages ≥ 12 received their fourth doses, of which just 17 were deemed to be serious.
In immunocompromised individuals ages 12 and older, fewer serious adverse events were reported to two US programs for tracking vaccine side effects following a second booster shot than after the first, researchers report in Morbidity and Mortality Weekly Report. The analysis tracked reports made to the v-safe voluntary, smartphone-based US active safety surveillance system and the Vaccine Adverse Event Reporting System (VAERS) passive surveillance system for all vaccine-associated adverse events co-managed by the US Centers for Disease Control and Prevention and the FDA. Most local and systemic reactions were minor and similar to those seen with dose three, authors say. A total of 145 reports of reactions were made to VAERS after 518,113 persons ages ≥ 12 received their fourth doses, of which just 17 were deemed to be serious.
Also in MMWR are more data supporting the efficacy of a fourth vaccine dose (or second booster) against the newer Omicron sublineages, even in adults without immune disorders. “Immunocompetent persons should receive recommended COVID-19 booster doses to prevent moderate-to-severe COVID-19, including a first booster dose for all eligible persons and second dose for adults aged ≥ 50 years at least 4 months after an initial booster dose,” the investigators write. “Booster doses should be obtained immediately when persons become eligible.”
Of note, the US is one of very few countries offering a fourth booster dose to immunocompetent adults ages 50 and older. Last week, European agencies revised their recommendations to suggest that people 60 and older should get a second booster at least 4 months after the first. The cutoff in the UK is currently age 75 and older after 4 months. Canada offers second boosters in non-immunocompromised adults over age 70, after a 6-month interval. Israel, on the other hand, started offering fourth doses to adults 18 and older back in January 2022.
 Contrary to reports from Europe and Asia, US adolescents and youth were more likely to catch COVID-19 than older adults during the first 6 months of the pandemic, when wild-type SARS-CoV-2 was surging. “For example,” researchers write in JAMA Network Open, “in Florida, the incidence rate in adolescents and youth was 0.055 compared with 0.028 in older adults—adolescents and youth had 1.94 times the risk of contracting COVID-19 compared with older adults (IRR 1.94; 95% CI 1.92-1.95).” Florida, they note, has recently decided to formally recommend against vaccines for children ages 5 to 17. These new data, as well as the more than 1,000 lives lost among those 18 and younger in the US, “argues against Florida’s position and supports CDC recommendations.”
Contrary to reports from Europe and Asia, US adolescents and youth were more likely to catch COVID-19 than older adults during the first 6 months of the pandemic, when wild-type SARS-CoV-2 was surging. “For example,” researchers write in JAMA Network Open, “in Florida, the incidence rate in adolescents and youth was 0.055 compared with 0.028 in older adults—adolescents and youth had 1.94 times the risk of contracting COVID-19 compared with older adults (IRR 1.94; 95% CI 1.92-1.95).” Florida, they note, has recently decided to formally recommend against vaccines for children ages 5 to 17. These new data, as well as the more than 1,000 lives lost among those 18 and younger in the US, “argues against Florida’s position and supports CDC recommendations.”
July 14, 2022
 The US Food and Drug Administration (FDA) yesterday gave the nod—through an emergency use authorization—to the protein-based COVID-19 vaccine with plant-based adjuvant from Novavax, for use in people 18 years and older. Agency scientists, as well as other vaccine experts, have said they hope that the more-traditional vaccine formulation may persuade unvaccinated Americans, wary of the newer mRNA products, to get the shot.
The US Food and Drug Administration (FDA) yesterday gave the nod—through an emergency use authorization—to the protein-based COVID-19 vaccine with plant-based adjuvant from Novavax, for use in people 18 years and older. Agency scientists, as well as other vaccine experts, have said they hope that the more-traditional vaccine formulation may persuade unvaccinated Americans, wary of the newer mRNA products, to get the shot.
“Today’s authorization offers adults in the United States who have not yet received a COVID-19 vaccine another option that meets the FDA’s rigorous standards for safety, effectiveness, and manufacturing quality needed to support emergency use authorization,” said FDA Commissioner Robert Califf, MD, in a statement. “COVID-19 vaccines remain the best preventive measure against severe disease caused by COVID-19 and I encourage anyone who is eligible for, but has not yet received a COVID-19 vaccine, to consider doing so.”
As STAT’s Matthew Herper explains, Novavax, a small Maryland biotech firm, faced a “bumpy path” in bringing its vaccine to the US market, as it was slow to wrap up clinical studies and then was plagued by manufacturing concerns.
Many patients with long COVID are spending hefty sums to travel to private clinics in Cyprus, Germany, and Switzerland for unproven treatments like apheresis and combination antithrombotic therapy, often driven by anecdotal reports of success on social media, an investigation by the BMJ and ITV News reveals. Speaking with TCTMD, one physician urged patients to be cautious. “We understand the need for symptom relief. We understand [the need] for people to put their lives back together and to move on, but be very cautious of treatments that are unproven, that have potential medical harm, and that are expensive.”
Just 6 weeks after ending its strict and highly contentious 2-month lockdown, Shanghai, China, is reporting a surge in COVID-19 cases. “Since early this month, Shanghai has recorded over 400 infections across the city, many of which have been traced to a cluster at a karaoke bar,” the New York Times reports. “Residents wary of being suddenly confined [again] in their homes have been alarmed by mixed messages from official sources circulating on social media, including advice that they stock up on food and medicine.”
 Eight clinical variables can serve as useful predictors of in-hospital mortality in STEMI patients with a current or recent COVID-19 infection, according to new data from the North American COVID-19 Myocardial Infarction (NACMI) registry published this week in JSCAI. Of 24 clinical variables identified, the ones most associated with in-hospital mortality were: respiratory rate > 35 breaths/minute, cardiogenic shock, oxygen saturation < 93%, age > 55 years, infiltrates on chest X-ray, kidney disease, diabetes, and dyspnea. TCTMD’s L.A. McKeown has the full story.
Eight clinical variables can serve as useful predictors of in-hospital mortality in STEMI patients with a current or recent COVID-19 infection, according to new data from the North American COVID-19 Myocardial Infarction (NACMI) registry published this week in JSCAI. Of 24 clinical variables identified, the ones most associated with in-hospital mortality were: respiratory rate > 35 breaths/minute, cardiogenic shock, oxygen saturation < 93%, age > 55 years, infiltrates on chest X-ray, kidney disease, diabetes, and dyspnea. TCTMD’s L.A. McKeown has the full story.
Just how long does immunity last after COVID-19 infection, and does that vary by age? Authors of a new study delving into this question performed serologic testing in 252 family clusters to look at the rate of waning, based on age. They found that among 902 study participants, 697 had confirmed SARS-CoV-2, including 351 children and 346 parents. At 1, 4, 5, and 10 months postinfection, children had significantly higher antibody titers, despite being more likely to have asymptomatic infections. Antibodies, the authors write in JAMA Network Open, “were found across several age classes of individuals with asymptomatic or mild COVID-19, which could help in optimizing COVID-19 vaccination strategies and prevention policies. This work provides further evidence of sustained immune response in children up to 1 year after primary SARS-CoV-2 infection.”
A JAMA news story, taking its cue from an earlier study published in Obstetrics & Gynecology, explains how booster shots during the second trimester of pregnancy help shore up maternal antibody titers that are also augmented in infants at the time of birth. “The findings support a COVID-19 maternal booster following full COVID-19 vaccination to protect both pregnant people and their infants,” writes Jennifer Abbasi.
 There’s more evidence that a fourth mRNA vaccine dose protects against severe outcomes in COVID-19, this time from Swedish long-term care facilities (LTCFs). Writing in the Lancet Regional Health – Europe, investigators say that a fourth dose, or second booster, of an mRNA COVID-19 vaccine, administered during the Omicron era, “was associated with reduced risk of death from all causes in residents of LTCFs and in the oldest old during the first 2 months, after which the protection became slightly lower.”
There’s more evidence that a fourth mRNA vaccine dose protects against severe outcomes in COVID-19, this time from Swedish long-term care facilities (LTCFs). Writing in the Lancet Regional Health – Europe, investigators say that a fourth dose, or second booster, of an mRNA COVID-19 vaccine, administered during the Omicron era, “was associated with reduced risk of death from all causes in residents of LTCFs and in the oldest old during the first 2 months, after which the protection became slightly lower.”
So is it time to definitively update what it means to be fully vaccinated? Becker’s Hospital Review summarizes the disparate viewpoints.
July 11, 2022
The European Centre for Disease Prevention and Control (ECDC) and the European Medicines Agency (EMA) are now recommending second booster shots of COVID-19 vaccines for people between 60 and 79 years old and those with comorbid conditions that increase the risk of severe disease. “These could be administered at least 4 months after the previous one, with a focus on people who have received a previous booster more than 6 months ago,” a press release states.
COVID-19 hospitalizations are up in the United States, as are deaths, rising 18% over the last 2 weeks and hitting the highest national average since March, Becker’s Hospital Review reports. Spikes in hospitalizations have been highest in Southern states: South Carolina saw numbers rise by 54% in the last 14 days, while those figures are 47% in Arkansas, 46% in Alabama, and 42% in Louisiana.
 Around the United Kingdom, hospitals and general practice clinics have returned to mandatory mask wearing by staff and patients as COVID case counts rise, the BMJ reports.
Around the United Kingdom, hospitals and general practice clinics have returned to mandatory mask wearing by staff and patients as COVID case counts rise, the BMJ reports.
Health authorities in many parts of the world have tried to strike a compromise between controlling transmission and minimizing socioeconomic disruptions by requiring people who test positive for COVID-19 to isolate for 5 days. As correspondence in the New England Journal of Medicine makes clear, however, viral shedding with the Omicron variant, as with Delta before it, likely continues in some people beyond the 5-day window following a positive test or symptom onset.
“America has decided the pandemic is over. The coronavirus has other ideas,” writes Joel Achenbach in the Washington Post, documenting the rise in reinfection rates with the latest COVID-19 variant. “It’s the Wild West out there,” epidemiologist Ziyad Al-Aly, is quoted in the article. “We’re in a very peculiar spot, where the risk is vivid and it’s out there, but we’ve let our guard down and we’ve chosen, deliberately, to expose ourselves and make ourselves more vulnerable.”
 Ambulatory patients who tested positive for COVID-19, and then were managed via remote patient monitoring programs staffed by round-the-clock nurses, appeared to have fewer hospitalizations, shorter lengths of stay if admitted, and less likelihood of needing ICU-level care, a study in JAMA Network Open suggests. “These findings suggest that remote patient monitoring for COVID-19 may help patients better manage symptoms at home and help hospitals better manage bed capacity,” the authors conclude.
Ambulatory patients who tested positive for COVID-19, and then were managed via remote patient monitoring programs staffed by round-the-clock nurses, appeared to have fewer hospitalizations, shorter lengths of stay if admitted, and less likelihood of needing ICU-level care, a study in JAMA Network Open suggests. “These findings suggest that remote patient monitoring for COVID-19 may help patients better manage symptoms at home and help hospitals better manage bed capacity,” the authors conclude.
The phase III ACTIV-3–TICO study suggests that the intravenous monoclonal antibody combination, tixagevimab-cilgavimab, compared with placebo, did not improve a primary outcome of time to sustained recovery, but it did lead to a 30% relative risk reduction for mortality up to day 90 in patients hospitalized with COVID-19. Though the study was conducted prior to the rise of Omicron, investigators note in the Lancet Respiratory Medicine that “in vitro data suggest that although the half maximal inhibitory concentration for tixagevimab-cilgavimab is higher against the Omicron (B.1.1.529 or BA.2) variant as compared with previous variants, clinical activity might be retained, albeit higher doses might be required.” The implication would be that this particular antibody combo might retain efficacy against newer variants where others have flagged and been removed from use, although this was not expressly tested. Importantly, the authors add, only 14% to 15% of patients in this trial were fully vaccinated.
An accompanying comment helps put the monoclonal antibody story in perspective as this virus evolves, concluding: “New trials adequately powered to current event rates within the emerging variant and immunity landscape are needed to establish whether there is a benefit to any antiviral or immunomodulatory therapy for patients with COVID-19.”
 It doesn’t bode well for future CVD prevention: children and teens worldwide experienced “measurable reductions” in physical activity during the first 2 years of the pandemic, a new review concludes. The analysis of more than 120 articles indicates that the percentage change in the duration total daily physical activity time from before COVID-19 was −20% and was particularly marked for higher-intensity activities. “There is an urgent need for public health initiatives to revive young people’s interest in, and support their demand for, physical activity during and beyond the COVID-19 pandemic,” researchers conclude in JAMA Pediatrics.
It doesn’t bode well for future CVD prevention: children and teens worldwide experienced “measurable reductions” in physical activity during the first 2 years of the pandemic, a new review concludes. The analysis of more than 120 articles indicates that the percentage change in the duration total daily physical activity time from before COVID-19 was −20% and was particularly marked for higher-intensity activities. “There is an urgent need for public health initiatives to revive young people’s interest in, and support their demand for, physical activity during and beyond the COVID-19 pandemic,” researchers conclude in JAMA Pediatrics.
July 7, 2022
As the highly transmissible BA.4 and BA.5 Omicron subvariants continue to their global sweep, several countries around the world have announced they are in, or entering, their “seventh wave” of the COVID-19 pandemic. The term made headlines in France and Canada this week, but countries worldwide have already seen case counts soar, the New York Times reports. The Times quotes cardiologist Eric Topol, MD, who last week wrote a summary of BA.5’s rise to prominence calling it “the worst version of the virus that we’ve seen.”
 There may be hope for the millions of people worldwide reporting loss of smell following COVID-19 infection. In the SCENT2 randomized, phase II clinical trial, participants treated with theophylline, a phosphodiesterase inhibitor, added to saline nasal irrigation reported greater gains in olfactory function as compared with those treated with a placebo. Those randomized to theophylline also had more improvement in objective smell identification scores after 6 weeks of twice-daily nasal irrigation. Full results appear in JAMA Otolaryngology-Head & Neck Surgery.
There may be hope for the millions of people worldwide reporting loss of smell following COVID-19 infection. In the SCENT2 randomized, phase II clinical trial, participants treated with theophylline, a phosphodiesterase inhibitor, added to saline nasal irrigation reported greater gains in olfactory function as compared with those treated with a placebo. Those randomized to theophylline also had more improvement in objective smell identification scores after 6 weeks of twice-daily nasal irrigation. Full results appear in JAMA Otolaryngology-Head & Neck Surgery.
The World Health Organization (WHO) is urging nations to “plug immunity gaps quickly before they are exploited by new sublineages of SARS-CoV-2,” the BMJ reports. In four out of six WHO regions, cases have risen by almost 30% in 2 weeks, amounting to 4.6 million new infections and representing the fourth week of rising numbers after declining trends this past spring. “Officials told a media briefing on 6 July that poorer nations are particularly vulnerable to a surge driven by the new lineages of the Omicron variant, as many of those countries have still not reached WHO’s vaccination targets or gained access to antivirals.”
Also in the BMJ, researchers write that a fourth vaccine dose helped to protect long-term care residents in Ontario, Canada, during an Omicron-dominant period, over and above the protection offered by a third dose. The marginal effectiveness gains were greater if subjects had received their last dose more than 84 days earlier. Compared with unvaccinated controls, effectiveness for vaccine recipients increased with each additional dose, and with the fourth dose was 49% against infection, 69% against symptomatic infection, and 86% against severe outcomes.
 Vaccine mandates have been vociferously lauded and opposed around the globe: nearly two and a half years into the pandemic, scientists are now trying to determine whether the benefits outweighed the potential damage to public trust, writes Liam Drew in a Nature news feature. Most studies indicate that mandates led to marked increases in vaccinations, Drew says, but they also exacted a toll in terms of public confidence, especially when policy makers were not crystal clear in their messaging around the rationales and aims of mandatory vaccines.
Vaccine mandates have been vociferously lauded and opposed around the globe: nearly two and a half years into the pandemic, scientists are now trying to determine whether the benefits outweighed the potential damage to public trust, writes Liam Drew in a Nature news feature. Most studies indicate that mandates led to marked increases in vaccinations, Drew says, but they also exacted a toll in terms of public confidence, especially when policy makers were not crystal clear in their messaging around the rationales and aims of mandatory vaccines.
Declines in life expectancy in California, seen in the first year of the pandemic, worsened in 2022, new data show. Those declines were greatest among racial and ethnic minority populations, particularly those living in lower-income areas. “The disproportionately large decreases in life expectancy among Hispanic and non-Hispanic Black populations reflect their exposure to higher COVID-19 infection, hospitalization, and death rates, especially early in the pandemic,” investigators write in JAMA.
An analysis of the different approaches taken by major cities around the globe to combat the pandemic offer insights into what works and what doesn’t for controlling transmissions in crowded urban settings. “The proposed population-level Swiss cheese model shows that it is not one barrier that is responsible for reducing the spread of the virus, rather multiple barriers and the interactions between those barriers are the driving force in determining the final output,” researchers write in the Lancet Regional Health: Southeast Asia.
In an analysis of 10 US states, immunocompromised patients accounted for more than 12% of all adult COVID-19 hospitalizations “and had increased odds of ICU admission and in-hospital death compared with nonimmunocompromised patients, irrespective of vaccination status,” researchers write in Morbidity and Mortality Weekly Report. While vaccination appears “highly protective” against hospitalization leading to fewer admissions and deaths, once hospitalized, the vaccination status of immunocompromised individuals did not seem to make a difference to ICU admissions, authors note.
A perspective by two American Board of Internal Medicine physicians in the New England Journal of Medicine this week asks: should physicians who spread misinformation be sanctioned? Policing physician opinion is a thorny business, they write, but “with nearly 1 million Americans dead from COVID, and deaths—some of them clearly preventable—continuing at a rate of more than 200,000 per year, it has become imperative for our profession to empower our institutions to signal clearly who is—and who is not—providing evidence-based information.”
July 4, 2022
Two studies of enoxaparin for thromboprophylaxis in COVID-19 have come up empty-handed. ETHIC, an open-label, multicenter, randomized, controlled, phase 3b trial conducted at 15 centers in six countries found no benefit to low-molecular weight heparin in unvaccinated symptomatic COVID-19 outpatients for a composite of all-cause mortality and hospitalization at 21 days, as compared with standard of care.
Likewise, OVID, a randomized, open-label, parallel-group, investigator-initiated, phase 3 trial of outpatients aged 50 years or older, conducted at eight centers in Switzerland and Germany, found no difference in a composite of hospitalization and all-cause death within 30 days between treated and untreated patients. Both trials were stopped early for futility. They are published this week in Lancet Haematology.
 COVID-19 has been blamed for widening existing inequalities: now survey results by McKinsey and Company suggest that men are more likely than women to be offered the option of remote work. As Becker’s Hospital Review summarizes, “men have more opportunities to work remotely full time than women do, with 38 percent of full-time employed men having remote work options, but only 30 percent of women having the same opportunity.”
COVID-19 has been blamed for widening existing inequalities: now survey results by McKinsey and Company suggest that men are more likely than women to be offered the option of remote work. As Becker’s Hospital Review summarizes, “men have more opportunities to work remotely full time than women do, with 38 percent of full-time employed men having remote work options, but only 30 percent of women having the same opportunity.”
A July 1, 2022 workshop co-chaired by the European Medicines Agency (EMA) and the US Food and Drug Administration (FDA) under the umbrella of the International Coalition of Medicines Regulatory Authorities saw regulators agreeing on key principles for the adaptation of vaccines to tackle virus variants, “ensuring global regulatory alignment,” a press release states.
Last week, the FDA committed to updating vaccines for the fall, but as the New York Times reports, the two mRNA vaccine-makers poised to offer updated boosters targeting the BA.4 and BA.5 strains say they won’t be ready until October—and that’s likely too late for the current surge in cases.
Obesity is a known risk factor for more severe COVID-19 illness, hospitalization, and death, but a new study in Lancet Diabetes & Endocrinology shows that vaccines appear to offer protection across the spectrum of body mass index (BMI). The study of more than 9 million adults in England showed that people with low or high BMI were at greater risk than healthy-weight, vaccinated adults, but vaccinated fared better than unvaccinated. Notably, the researchers say, underweight people were less likely to be vaccinated.
A longitudinal observational study of healthcare workers with prior SARS-CoV-2 infections not requiring hospitalization indicates that the likelihood of developing Long COVID is reduced in people who have had two or three mRNA vaccine doses. Lasting symptoms were more common in the first wave of the pandemic than in subsequent waves, and in people with older age, higher BMI, allergies, and/or obstructive lung disease, researchers write in JAMA.
 An analysis of vaccination facilities and uptake of vaccines in children aged 5-11 indicates that pediatric clinics, family medicine clinics, and federally qualified health centers increase the likelihood of childhood vaccinations. While most US counties had pharmacies or public health centers offering vaccines to kids, those facilities more recognizable by parents as providing pediatric care appeared to boost confidence in vaccine safety, improving access, researchers write in Morbidity and Mortality Weekly Report. “Providers that serve as a medical home for routine pediatric care has important implications for COVID-19 vaccination coverage.”
An analysis of vaccination facilities and uptake of vaccines in children aged 5-11 indicates that pediatric clinics, family medicine clinics, and federally qualified health centers increase the likelihood of childhood vaccinations. While most US counties had pharmacies or public health centers offering vaccines to kids, those facilities more recognizable by parents as providing pediatric care appeared to boost confidence in vaccine safety, improving access, researchers write in Morbidity and Mortality Weekly Report. “Providers that serve as a medical home for routine pediatric care has important implications for COVID-19 vaccination coverage.”
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full Bio



Comments