Evinacumab Helps Severe Hypercholesterolemia Patients Reach LDL Targets
The study included patients with heterozygous FH who may not see adequate LDL drops with statins and PCSK9 inhibitors.
Patients with severe hypercholesterolemia who are unresponsive to a number of lipid-lowering therapies, including a PCSK9 inhibitor and high-dose statin, can have a significant reduction in LDL-cholesterol levels when treated longer-term with evinacumab (Evkeeza; Regeneron), a new open-label study shows.
LDL levels were cut nearly in half from baseline and more than 50% of patients got to the recommended treatment target of less than 70 mg/dL, report investigators, while one-third got down below 55 mg/dL. In terms of safety, the most common side effect was nasopharyngitis (12.5%), but no treatment-emergent adverse events led to deaths or stopping treatment.
“Of patients with heterozygous familial hypercholesterolemia, which was about three-quarters of our population—they had clinical characteristics and genetically confirmed familial hypercholesterolemia—about 20% still have an LDL-cholesterol level above the minimally acceptable targets,” lead investigator Robert Rosenson, MD (Icahn School of Medicine at Mount Sinai, New York, NY), told TCTMD. “The reason that it's so important to achieve the targets is that these individuals had an elevated LDL cholesterol before they were born and we know that the onset of coronary heart disease begins early.”
The most common cause of familial hypercholesterolemia (FH) is a mutation in the LDLR gene, which leads to diminished or absent uptake and clearance of circulating LDL-cholesterol levels by the liver. Other less common causes include missense mutations of the apolipoprotein B (ApoB) gene and gain‐of‐function mutations in the gene for proprotein convertase subtilisin/kexin 9 (PCSK9).
“Individuals who have the most severe cholesterol-raising traits are those with impaired LDL receptor activity,” said Rosenson. “If the LDL receptor activity is genetically low, upregulating the LDL receptor by the use of a statin or a PCSK9 inhibitor is probably going to produce half the benefit that it will in somebody without that type of mutation. Those individuals need something more. Something more means a therapy that doesn't work by upregulating a defective LDL receptor alone, but one that works by lowering cholesterol by a non-LDL receptor approach.”
Evinacumab is one such option. It is a fully human monoclonal antibody inhibitor of angiopoietin-like protein 3 (ANGPTL3), which plays a role in regulating lipid metabolism. It was approved in 2021 by the US Food and Drug Administration as a breakthrough therapy for patients with homozygous FH (HoFH), including pediatric patients. It’s administered by weight (15 mg/kg) and comes with a hefty price tag: the average wholesale acquisition cost is roughly $450,000 per year.
Pathway is Effective
The new study, which is published this week in JAMA Cardiology, focuses on patients with primary hypercholesterolemia refractory to lipid-lowering therapy. It is an open-label extension study of patients who participated in the phase II, double-blind study that showed evinacumab at the maximum dose (delivered subcutaneously or intravenously) reduced LDL cholesterol by approximately 50% from baseline. The open-label study aimed to evaluate the longer-term safety and tolerability of evinacumab 15 mg/kg delivered intravenously every 4 weeks.
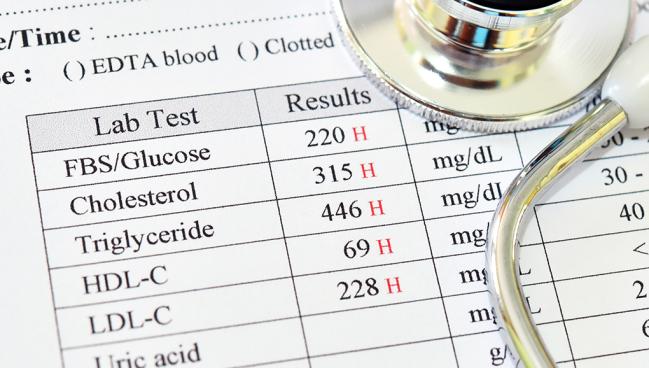
Of the 96 patients included, 82.3% had a diagnosis of heterozygous (HeFH) and 17.7% had a history of clinical atherosclerotic cardiovascular disease (ASCVD) without FH. The vast majority of patients were white (89.6%), with just 13 patients self-reporting as Black, Asian, or Hispanic/Latino. The mean LDL level at baseline—the start of the double-blind treatment study—was 145.9 mg/dL even though nearly all patients (95.8%) were taking a PCSK9 inhibitor and a statin (84.4%). More than half of patients were taking a high-intensity statin (53.1%), and all were taking maximal doses they could tolerate. More than one-third were also taking ezetimibe.
At week 72, the end of the open-label treatment period, LDL-cholesterol levels were reduced by 45.5%. For those who received evinacumab 15 mg/kg or 5 mg/kg intravenously in the double-blind study, LDL levels were reduced by 43.0% and 49.9% from baseline. For the placebo-treated patients in the double-blind study, LDL levels were reduced by 43.8% when switched to evinacumab in the open-label treatment period. LDL levels were reduced to a similar extent in patients with loss-of-function LDLR variants, gain-of-function PCSK9 variants, or missense variations in LDLR.
By the end of the study, 31.3% achieved the LDL-cholesterol target of less than 55 mg/dL and 52.5% got down below 70 mg/dL, which are the recommended treatment goals for very-high-risk and high-risk patients.
Need for Price to Come Down
While HoFH is very rare—the prevalence is estimated to be roughly one in 300,000—HeFH is more common, affecting approximately one in 250 people. Intravenous evinacumab is priced as an orphan drug for HoFH but would be prohibitively expensive to use more liberally in patients with the more common HeFH. Other companies are currently developing small interfering ribonucleic acid (siRNA) therapies designed to silence expression of the ANGPTL3 gene and the hope is that if they come to fruition, creating marketplace competition, the cost of treatment would come down, said Rosenson. Additionally, subcutaneous drug delivery, which has already been shown to reduce LDL levels by 50%, would be more convenient for patients as the monthly intravenous infusion requires a full hour.
“This [study] supports that this pathway is effective,” said Rosenson. “Maybe the IV formulation is going to limit the widespread applicability, and it may be better with a subcutaneous formulation, but there are multiple pharmaceutical companies that are investigating RNA inhibitors directed against ANGPTL3. There are opportunities for this non-LDL-receptor pathway for lowering LDL cholesterol. In other words, this isn't the end of the story.”
In 2022, Pfizer and Ionis Pharmaceuticals discontinued the development of vupanorsen, an antisense oligonucleotide aimed at ANGPTL3 mRNA in the liver, following safety concerns in the TRANSLATE-TIMI 70 study. In that small, placebo-controlled study, vupanorsen modestly lowered non-HDL-cholesterol levels, it but was associated with increases in liver fat, elevation in liver enzymes at higher doses, and frequent injection-site reactions.
Michael O’Riordan is the Managing Editor for TCTMD. He completed his undergraduate degrees at Queen’s University in Kingston, ON, and…
Read Full BioSources
Rosenson RS, Burgess LJ, Ebenbichler CF, et al. Longer-term efficacy and safety of evinacumab in patients with refractory hypercholesterolemia. JAMA Cardiol. 2023;Epub ahead of print.
Disclosures
- Rosenson reports grant support and/or personal fees from Regeneron, Amgen, Arrowhead, Avilar Therapeutics, CRISPR Therapeutics, Kowa, Lilly, Lipigon, Merck, Novartis, Precision Biosciences, UpToDate, UltraGenyx, and Verve Therapeutics. He reports stock holdings in MediMergent.





Comments