‘Hot’ Plaque on Noninvasive PET May Presage MI, CV Death: PRE18FFIR
An expanded primary endpoint came up short, but 18F-sodium fluoride PET imaging shows promise for predicting future risk.

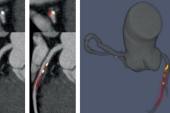
BARCELONA, Spain—A novel, noninvasive technique that takes its cue from cancer diagnostics looks promising for identifying “hot” plaques without the need for intravascular imaging, successfully predicting the future risk of MI or cardiovascular death, results from the prospective, multicenter PRE18FFIR study show.
The study’s primary endpoint, which had been expanded postlaunch to include unplanned coronary revascularization, was not met, due—ironically—to the lack of an association between hot plaques and subsequent reinterventions.
“This technique could be used to identify patients who have active disease and are at risk of heart attacks, tailor treatments to prevent future heart attacks, and assess the effectiveness of new treatments to prevent heart attacks,” said David Newby, MD, PhD (University of Edinburgh, Scotland), who presented the findings here at a European Society of Cardiology (ESC) Congress 2022 Hot Line session.
What it does not do, he stressed, is predict the need for future stents or bypass surgery.
Some Have It Hot
A prior retrospective, post hoc pooled analysis of patients with cardiovascular disease established a link between increased coronary microcalcification activity (CMA) on 18F-sodium fluoride positron emission tomography (PET) and subsequent risk of myocardial infarction in patients with established coronary artery disease. A similar imaging technique was used in the FAABULOUS 2 study to look for valve deterioration after TAVI.
The current study, conducted at nine centers in four countries between 2015 and 2020, prospectively enrolled 704 patients with recent MI (within the prior 21 days) and multivessel CAD. All patients underwent 18F-sodium fluoride positron PET and coronary CTA, then were followed for a minimum of 2 years (and an average of 4 years).
As Newby showed here, rates of the revised primary endpoint were no different between patients with and without CMA (HR 1.25; 95% CI 0.89-1.76) due in large part to the lack of an association with unscheduled coronary revascularization (HR 0.98; 95% CI 0.64-1.49).
But for the trial’s original endpoint, CV death or MI, event rates were significantly increased over follow-up in patients found to have evidence of “hot” arteries on PET imaging during their baseline scan (HR 1.82; 95% CI 1.07-3.10). Rates of death from any cause were also significantly higher (HR 2.43; 95% CI 1.15-5.12). For both endpoints, separation of Kaplan-Meier curves occurred within the first few months.
“This is the first demonstration of a method of directly seeing disease activity in heart arteries without the need to instrument the body,” Newby told journalists at an ESC press conference prior to his Hot Line presentation. PET, he noted, is “widely used” in cancer but PRE18FFIR carves out a role for cardiovascular risk assessment, independent from other methods of predicting atherosclerotic cardiovascular disease.
To TCTMD, Newby stressed that the goal of PET imaging in this context is not to identify “hot” plaques with the aim of treating them prophylactically, but rather to assess and quantify the degree of higher-risk plaques which, combined with CT, can generate a risk score that can be actionable.
Next steps, he said, are to “dig deeper” into the validation cohort, analyze the PET imaging alongside the CT scans to see whether similar information could be gleaned from CT alone, but also to extend the follow-up. The P values, while significant, were “quite nominal,” so longer follow-up would paint a clearer picture. “We're also very keen to work with pharma, to test this technique against their new therapies, because it will really enrich the population,” Newby added.
Digging Deeper
Commenting on the study for TCTMD, George Dangas, MD, PhD (Icahn School of Medicine at Mount Sinai, New York), noted that prior to this study, most of the imaging research into “vulnerable” plaques has relied on modalities like near-infrared spectroscopy (NIRS) measures of fibrous cap thickness, or the presence of lipid-rich plaques on optical coherence tomography (OCT), both of which require intravascular wires and catheters.
“Always the question was, if what you find from this sophisticated instrumentation is not related to the plaque you see right there, but is more of a patient risk, then why can't we find another way to detect that noninvasively? I think today’s study shows nicely that a scan, the 18F PET, can detect hot areas inside the coronary artery, but again, gives you a sense of the patient’s risk, not plaque risk,” he explained.
Perhaps subsequent analyses, Dangas continued, could “tell us what happened to those hot spots—a ‘hot spot analysis’ as well as a patient analysis. And then there is yet another step needed to see if treating those spots is going to make some difference in patient outcomes. . . . We need a couple more steps, but this is a very important first step showing that noninvasive detection is possible. We can now do studies with more patients, which was something we could not really do before with invasive methods [which were] too expensive, too invasive, and too risky.”
Also commenting for TCTMD, Sarah Clarke, MD (Cambridge Heart Clinic, England), pointed out that risk score calculators—alongside invasive tests—are what clinicians have at their disposal for trying to predict future events for patients recovering from a first MI. As such a noninvasive test for tracking coronary microvascular activity and modulation through lipid-lowering therapies, anti-inflammatory agents, or other novel drugs would be welcome.
“I think this can definitely be used for assessing new drugs, but I think it could also be clinically useful,” she observed. That said, “not everyone has a PET scanner, so the actual roll-out of this would be limited by the availability and access to a PET scanner, but certainly in the research world it would be very useful.”
Betty Raman, MBBS, DPhil (University of Oxford, England), the scheduled discussant after Newby’s presentation today, noted that particularly given the constraints of the pandemic, “it’s amazing and remarkable that the investigators were able to launch this study to evaluate the prognostic utility of microcalcification/plaque activity in high-risk patients.”
That said, she did offer a few words of caution. Serious adverse events in the trial were very low, she noted, “but accumulating radiation exposure remains a concern in the real world.”
Outcomes seen in the study may partly reflect changes in behavior associated with pandemic lockdowns, while the high cost of acquiring a PET scanner and accessing the procedure may limit its use in routine practice.
Lastly, she noted, Newby and colleagues themselves have done pioneering studies looking at the ability of low-attenuation plaque volume on coronary CTA to predict later events. “We do need to consider the incremental value of coronary microcalcification activity assessment on PET-CT over CT-based features of high-risk plaques, or vice versa,” said Raman, “and that remains to be studied.”
Shelley Wood was the Editor-in-Chief of TCTMD and the Editorial Director at the Cardiovascular Research Foundation (CRF) from October 2015…
Read Full BioSources
Newby, D. ‘Hot’ coronary artery disease predicts heart attacks. The PRE18FFIR study. Presented at: ESC 2022. August 28, 2022. Barcelona, Spain.
Disclosures
- Newby reports grants, consultancy, or clinical trial contracts with: Abbott, Amgen, AstraZeneca, Autoplaque, BMS, Boehringer Ingleheim, Cleerly, Elly Lilly, GE, GSK, Jansen, MSD, Novartis, Pfizer, Phillips, Roche, Sanofi, Siemens, Toshiba, UCB, Wyeth, and Zealand, and research funding from the British Heart Foundation, Medical Research Council, Welcome Trust, Chief Scientist Office, Chest, and Heart Stroke Scotland.
- Dangas reports consultant fees/honoraria from Biosensors and Janssen Pharmaceuticals; stock from ControlRad and Elixir; ownership interest/partnership/principal in Applied Therapeutics and STEL; and research grants from Abbott, AstraZeneca, and Daiichi Sankyo.
- Clarke reports no relevant conflicts of interest.
- Raman reports consulting for Axcella Therapeutics and holding a patent on a new oxygen-sensitive MRI technology.




Comments