COVID-19: TCTMD’s Daily Dispatch for August Week 1
We’re curating a list of COVID-19 research and other useful content, and updating it regularly.

Since March 2020, TCTMD reporter Todd Neale has been writing up breaking news and peer-reviewed research related to COVID-19 every weekday. In July 2021, we transitioned to Mondays, Wednesdays, and Fridays. If you have something to share, tell us. All of our COVID-19 coverage can be found on our COVID-19 Hub.
August 6, 2021
Following last week’s emergency use authorization update by the US Food and Drug Administration (FDA) for the casirivimab and imdevimab combo (REGEN-COV; Regeneron) as postexposure prophylaxis for COVID-19 in people age 12 years and older, a New England Journal of Medicine paper shows that subcutaneous use of the agent led to greater than 60% reductions in symptomatic and asymptomatic disease in previously uninfected household contacts of persons with a diagnosis of SARSCoV-2 infection. Minor to no adverse events were reported.
Also in the New England Journal of Medicine, therapeutic-dose anticoagulation with heparin appears to be superior to standard thromboprophylaxis at improving survival with reduced need for organ support in noncritically-ill COVID-19 patients, TCTMD’s Shelley Wood reports. Yet the data, from a large, global collaboration of RCTs, suggest that the therapy does not beat out usual-care thromboprophylaxis in those who require ICU-level care. 
The Biden administration’s COVID-19 data director says vaccinations are on the rise this summer in the United States. In a tweet, Cyrus Shahpar, MD, said more than 864,000 doses were administered on August 5, which included 585,000 newly vaccinated individuals. Those were the highest single-day numbers since early July. CNN reports that Jeff Zients, the White House coronavirus response coordinator, attributed much of the momentum to businesses and colleges adopting vaccination requirements.
The European Medicines Agency (EMA)'s Pharmacovigilance Risk Assessment Committee (PRAC) is recommending an update to the product information for the Janssen COVID-19 vaccine that calls attention to the potential for immune thrombocytopenia, dizziness, or tinnitus as adverse reactions.
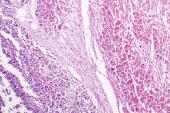
 Data from electronic medical records suggest that the incidence of myocarditis and pericarditis following vaccination for COVID-19 is 1.0 case per 100,000 and 1.8 cases per 100,000, respectively. Although those numbers are higher than what the Centers for Disease Control and Prevention (CDC) previously reported, the lead author told TCTMD’s Michael O’Riordan that physicians should be reassuring when conveying the risk to patients, adding that the likelihood of developing myocarditis after the jab is almost 10 times smaller than the chance of being struck by lightning.
Data from electronic medical records suggest that the incidence of myocarditis and pericarditis following vaccination for COVID-19 is 1.0 case per 100,000 and 1.8 cases per 100,000, respectively. Although those numbers are higher than what the Centers for Disease Control and Prevention (CDC) previously reported, the lead author told TCTMD’s Michael O’Riordan that physicians should be reassuring when conveying the risk to patients, adding that the likelihood of developing myocarditis after the jab is almost 10 times smaller than the chance of being struck by lightning.
Healthcare workers in South Africa who received the single-dose Johnson & Johnson vaccine are seeing high levels of protection from COVID-related death. The study’s co-lead author told Reuters that the more than 477,000 vaccinated healthcare workers have shown up to 96.2% protection against death compared with unvaccinated controls. Additionally, 96% of breakthrough infections among the workers have been mild, and rates of protection against hospitalization are durable at 65% out to 120 days postvaccination.
Research on patients with long COVID supports the idea that specialized clinics are needed to triage patients for further testing and treatment. “Females under 50, and those with severe acute disease requiring critical care had the worst long-term outcomes even after adjusting for severity of the initial illness,” the authors write in the Lancet.
Individuals who have been previously infected with COVID-19 have higher antibody levels after a single dose of the Pfizer/BioNTech vaccine than people who have received two doses of the vaccine but were not previously infected, a small study suggests. “This study highlights the potential for recommending a single dose for previously infected individuals and may be useful for discussions surrounding vaccination strategy,” researchers write in a letter published in JAMA Network Open.
 On Thursday, Tokyo reported more than 5,000 new COVID-19 cases, marking the Olympic host city’s highest ever single-day total, Time reports.
On Thursday, Tokyo reported more than 5,000 new COVID-19 cases, marking the Olympic host city’s highest ever single-day total, Time reports.
States such as Texas and Iowa that have banned schools and state government agencies from implementing mask mandates are putting immunocompromised individuals at risk in the workplace and denying them safety accommodations that they are entitled to under the Americans with Disabilities Act (ADA), a JAMA viewpoint contends.
L.A. McKeown contributed today’s Dispatch.
August 4, 2021
Japanese officials are warning of an “unprecedented” new phase of COVID-19, blamed on the influx of cases and opportunities for transmission at the Olympic Games. “Tokyo reported a record 4,166 new cases on Wednesday,” Reuters reports. “Nationwide, newly reported cases totaled a new record of over 14,200, according to public broadcaster NHK.”
 The World Health Organization (WHO) called today for a moratorium on booster shorts for COVID-19 (following full vaccination) until the end of September, hoping that by that time all countries will have vaccinated at least 10 percent of their populations. “We cannot—and we should not—accept countries that have already used most of the global supply of vaccines using even more of it, while the world’s most vulnerable people remain unprotected,” Director General Tedros Adhanom Ghebreyesus said in a briefing. The New York Times has details.
The World Health Organization (WHO) called today for a moratorium on booster shorts for COVID-19 (following full vaccination) until the end of September, hoping that by that time all countries will have vaccinated at least 10 percent of their populations. “We cannot—and we should not—accept countries that have already used most of the global supply of vaccines using even more of it, while the world’s most vulnerable people remain unprotected,” Director General Tedros Adhanom Ghebreyesus said in a briefing. The New York Times has details.
Also in the New York Times, the US Food and Drug Administration (FDA) has signaled that it would formally approve the Pfizer/BioNTech vaccine as soon as early September. All of the vaccines currently in use in the United States to date have been cleared under the agency’s expedited emergency use authorization.
The United Kingdom’s Joint Committee on Vaccination and Immunization has announced that COVID-19 vaccination can now be offered to 16- and 17-year-olds, who do not need a parent’s permission to get it, the Guardian reports. The Guardian also offers an exploration of which countries around the globe have opened up vaccines to minors, a more pressing concern than ever as the more transmissible Delta variant spreads and kids return to school.
The Delta variant is responsible for more breakthrough infections than originally feared, the latest analysis from the UK’s REACT-1 survey suggests. In an update released today, REACT-1 investigators say that infections “were three times lower in people who were fully vaccinated, compared to unvaccinated people. The data also suggested that people who were fully vaccinated were less likely to pass the virus on to others, due to having a lower viral load on average and therefore shedding less virus.” But as a preprint study and accompanying explainer make clear, 44% of infections occurred in fully vaccinated subjects, driven by “complete replacement” of the Alpha variant by Delta.
The European Medicines Agency (EMA) and the European Centre for Disease Prevention and Control (ECDC) today issued a strongly worded press release urging all Europeans to get fully vaccinated. “While the available vaccines are highly effective in protecting people against severe COVID-19, until higher proportions of the population are immunized, the risk is not beyond us,” Mike Catchpole, ECDC’s chief scientist is quoted. “We are now witnessing an increasing number of COVID-19 cases across the EU/EEA and vaccines remain the best available option to avoid an increase in severe disease and death.”
 The risk of acute MI or stroke was increased threefold in the first 2 weeks after COVID-19 infection among all Swedish residents who contracted the virus over more than a 7-month period, according to a large cohort study published in the Lancet. Speaking with TCTMD’s L.A. McKeown, senior author Anne-Marie Fors Connolly, PhD stressed: “As a clinician it’s important to note that [acute MI or stroke] could be the first thing you see in a COVID-19 patient,” a concern that she said should help drive people to get fully vaccinated.
The risk of acute MI or stroke was increased threefold in the first 2 weeks after COVID-19 infection among all Swedish residents who contracted the virus over more than a 7-month period, according to a large cohort study published in the Lancet. Speaking with TCTMD’s L.A. McKeown, senior author Anne-Marie Fors Connolly, PhD stressed: “As a clinician it’s important to note that [acute MI or stroke] could be the first thing you see in a COVID-19 patient,” a concern that she said should help drive people to get fully vaccinated.
Children are much less likely to develop long COVID symptoms, researchers report in the Lancet: Child and Adolescent Health. “Fewer than one in 20 children with symptomatic COVID-19 experienced symptoms lasting longer than 4 weeks, and almost all children have fully recovered by 8 weeks,” a press release issued by investigators at Kings College London explains.
An analysis of the 40 hospitals in the Pacific Northwest Providence Health System indicates that of more than 2 million vaccinated subjects, 20 had vaccine-related myocarditis and 37 developed pericarditis. Median time to myocarditis was 3.5 days, and three-quarters of the subjects were male. Pericarditis, on the other hand, developed a median 20 days after vaccination, although again 73% were male. Unlike earlier series, median age was older in this series—36 years for myocarditis and 59 years for pericarditis. “Myocarditis developed rapidly in younger patients, mostly after the second vaccination. Pericarditis affected older patients later, after either the first or second dose,” the authors summarize. The incidence of the two vaccine-related cardiac effects appears to be higher than what the CDC has suggested, they write in JAMA.
A new review in JAMA Network Open exposes the widely disparate recommendations for respiratory protection among healthcare professionals in different national and international guidelines. Conflicting evidence regarding transmission, particularly for airborne, likely played a role in influencing the different recommendations, the authors note but caution: “Inconsistencies in respiratory protection guidelines between neighboring countries created confusion over optimal measures. Strong collaborations between national and international organizations are critical in such circumstances.”
 Countries all over the world reported a stark decline in hospitalizations for acute MI and stroke during the early COVID-19 pandemic. Now, a study published in JAMA Cardiology reveals that in the United States, Medicare beneficiaries nationwide were even less likely to report to hospitals with MI and stroke than were younger, commercially insured adults. And while rates have returned closer to normal in many analyses, they’ve remained “substantially lower” for Medicare patients than in years prior.
Countries all over the world reported a stark decline in hospitalizations for acute MI and stroke during the early COVID-19 pandemic. Now, a study published in JAMA Cardiology reveals that in the United States, Medicare beneficiaries nationwide were even less likely to report to hospitals with MI and stroke than were younger, commercially insured adults. And while rates have returned closer to normal in many analyses, they’ve remained “substantially lower” for Medicare patients than in years prior.
TCTMD Managing Editor Shelley Wood contributed today’s Dispatch.
August 2, 2021
Late Friday, the US Food and Drug Administration (FDA) updated the emergency use authorization for the casirivimab and imdevimab combination (REGEN-COV; Regeneron) as postexposure prophylaxis for COVID-19 in adults and pediatric individuals 12 years of age and older who would be at high risk for progression to severe COVID-19, hospitalization, or death if they contracted the virus. Prescribing details spell out both the definition of "exposure" as well as the type of patient in whom prophylactic administration is intended to help—singling out unvaccinated patients, as well as those in whom a strong immune response is unlikely, for example, immunocompromised patients. The agent is not authorized for pre-exposure prophylaxis to prevent COVID-19 before being exposed to the SARS-CoV-2 virus “and is not a substitute for vaccination,” the FDA warns in bold font.
Two papers, relying on the now-suspect Surgisphere data set, became the poster children for shoddy research and patchy peer review earlier in the pandemic: one on hydroxychloroquine, published in the Lancet, and the other on the association between CVD, renin-angiotensin–aldosterone system inhibitors, and COVID-19 outcomes, published in the New England Journal of Medicine. Both were rapidly retracted. Now, a new paper tallies up the number of times the NEJM paper was cited in the medical literature, both prior to and after retraction, including 21 citations in May 2021 alone. “Our findings challenge authors, peer reviewers, journal editors, and academic institutions to do a better job of addressing the broader issues of ongoing citations of retracted scientific studies and protecting the integrity of the medical literature,” investigators conclude.
Members of the Centers for Disease Control and Prevention (CDC) have published their analysis of reactions to the Pfizer/BioNTech mRNA vaccine among 12-to 17-year-olds during the period from December 14, 2020, to July 16, 2021. Among 8.9 million adolescents vaccinated during that time, “reports were received for approximately one per 1,000 vaccinees, and 90% of these reports were for nonserious conditions.” Injection site pain, fatigue, headache, dizziness, syncope, and myalgia were the most common; myocarditis (and conditions associated with myocarditis) were among the most serious. Fewer than 10% of patients reported serious events including chest pain and death; most of these were in males following their second dose, median age 15. “Fewer than 1% of adolescents aged 12-17 years required medical care in the week after receipt of either dose; 56 adolescents (0.04%) were hospitalized,” investigators conclude in Morbidity and Mortality Weekly Report.
 In a Lancet comment, Beate Kampmann, PhD, and Uduak Okomo, MBBCh, PhD, address yet another layer of vaccine inequity: more than 30 randomized trials are recruiting children as young as 6 months old as candidates for COVID-19 vaccination, but other lifesaving vaccinations are falling by the wayside. While the safety data to date in kids are “reassuring” for the COVID-19 vaccines already in use for adults and there’s plenty of reason to assume they’d also be effective, the ethics of prioritizing COVID-19 vaccination in the young are fraught. There’s a paucity of vaccines in low- and middle-income countries where even the highest-risk members of the population have not yet received their first COVID-19 doses, yet vaccine programs, by focusing on adults, are dropping the ball on vaccinations already known to benefit babies and kids, according to Kampmann and Okomo. “During deliberations on the potential benefits of COVID-19 vaccines for children and young people, it is important to recognize that this pandemic has already deprived more than 8 million children, primarily in low- and middle-income countries, from lifesaving, routine childhood vaccines,” they write.
In a Lancet comment, Beate Kampmann, PhD, and Uduak Okomo, MBBCh, PhD, address yet another layer of vaccine inequity: more than 30 randomized trials are recruiting children as young as 6 months old as candidates for COVID-19 vaccination, but other lifesaving vaccinations are falling by the wayside. While the safety data to date in kids are “reassuring” for the COVID-19 vaccines already in use for adults and there’s plenty of reason to assume they’d also be effective, the ethics of prioritizing COVID-19 vaccination in the young are fraught. There’s a paucity of vaccines in low- and middle-income countries where even the highest-risk members of the population have not yet received their first COVID-19 doses, yet vaccine programs, by focusing on adults, are dropping the ball on vaccinations already known to benefit babies and kids, according to Kampmann and Okomo. “During deliberations on the potential benefits of COVID-19 vaccines for children and young people, it is important to recognize that this pandemic has already deprived more than 8 million children, primarily in low- and middle-income countries, from lifesaving, routine childhood vaccines,” they write.
Meanwhile, in JAMA Pediatrics, a viewpoint published today serves as a reminder that “long COVID,” increasingly discussed in adults, is poorly understood in children and young people have typically not been the focus of studies. Their paper lays out a framework for addressing unmet needs and the potential future impact of long COVID-19 symptoms on children and society.
Last week, a host of cardiology groups signed a joint statement supporting mandatory COVID-19 vaccinations for healthcare workers, but the American Heart Association (AHA) was conspicuously absent. Contacted by TCTMD, an AHA spokesperson said in an email that the organization “routinely collaborates” with colleagues at the American College of Cardiology (ACC) and other professional societies. “Sometimes our collaboration is reflected in joint activities and statements, other times not. The AHA continues to closely align with and publicly support the US Centers for Disease Control and Prevention’s recommendations: all adults and children ages 12 and older in the US are recommended to receive a COVID-19 vaccine as soon as they can receive it, as authorized by the US Food and Drug Administration.”
 In a troubling finding, researchers studying prescribing patterns among 75,000 Ontario, Canada, nursing home residents found that during the first 6 months of the pandemic in 2020, prescriptions for psychotropic, anticonvulsant, and opioid medications increased significantly, whereas no changes were seen for antibiotics, ACE inhibitors, or ARBs. The study findings were reported in JAMA Network Open. “The short-term increase in prescribing of these potentially inappropriate medications with known harms is concerning, especially given that the conditions that nursing home residents were living under during the pandemic may have resulted in these changes,” an editorial notes.
In a troubling finding, researchers studying prescribing patterns among 75,000 Ontario, Canada, nursing home residents found that during the first 6 months of the pandemic in 2020, prescriptions for psychotropic, anticonvulsant, and opioid medications increased significantly, whereas no changes were seen for antibiotics, ACE inhibitors, or ARBs. The study findings were reported in JAMA Network Open. “The short-term increase in prescribing of these potentially inappropriate medications with known harms is concerning, especially given that the conditions that nursing home residents were living under during the pandemic may have resulted in these changes,” an editorial notes.
Japan’s COVID-19 Olympics nightmare will soon be “coming true,” the Globe and Mail predicts. Over the weekend, new case counts set a record, with 4,058 infections on Saturday and more than 3,000 on Sunday. “’Tokyo is heading toward an explosive spread of infection never experienced before,’ the city’s municipal government said. Hospitalizations have doubled in the past month, ‘and the situation is starting to place a strain on the healthcare system,’” Nathan Vanderklippe reports.
TCTMD Managing Editor Shelley Wood contributed today’s Dispatch.
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full Bio



Comments