‘Proof-of-Concept’ AI-ECG May Improve STEMI Care: ARISE
The tool cut the time from ECG to cath lab by 10 minutes, but the positive result comes with caveats about the trial’s methodology.
An artificial intelligence (AI) algorithm that mines ECG data and alerts the primary PCI team to activate the cath lab can reduce STEMI patients’ arrival times by as much as 10 minutes, according to the single-center, randomized ARISE trial.
The AI-based algorithm joins a growing field where machine-based learning is used to glean information clinicians might miss to improve patient care—including for identifying low LVEF, LV systolic dysfunction, long QT syndrome, diabetes, atrial fibrillation, coronary calcium, and even “physiologic age.”
No randomized trials have yet explored using ECGs to diagnose STEMI, a condition wherein reducing time to treatment can mean life or death, said Chin-Sheng Lin, MD, PhD (Tri-Service General Hospital, Taipei, Taiwan), who presented the ARISE data during a late-breaking science session at American Heart Association (AHA) 2023 Scientific Sessions. “It is still a challenge to rapidly recognize STEMI with the initial misdiagnosis rate of 20.5%,” he said. “Therefore, developing a decision support system to early diagnose acute MI by ECG provides unmet needs for clinical physicians.”
The AI-assisted technique, specifically, sends a text message to the emergency department and on-call cardiologists to activate the cath lab for primary PCI upon identifying likely STEMI on an ECG, thus shaving precious time off the process. The exact methodology by which ARISE identifies STEMI is a “black-box system,” Lin said during a press conference, but it can predict both the presence of STEMI and NSTEMI, though the latter has yet to be studied.
ARISE proposes a unique solution to a plateau in STEMI care seen in recent years, after so much improvement seen in reducing door-to-balloon times across the United States with dedicated teams and care pathways, according to Rohan Khera, MD (Yale School of Medicine, New Haven, CT), who served as a panelist during the session.
“We have spent so much time optimizing STEMI management over the years,” he told TCTMD. “And often we don't know what the next add-on would be. Like, how would we go further and better?”
Commenting on the findings during an AHA press conference, Brahmajee Nallamothu, MD, MPH (University of Michigan, Ann Arbor), commended the authors for studying “an incredible application of an AI technology in a real-world problem.” With many such tools “struggling to find any kind of meaningful use,” he said, the algorithm used in ARISE might have “large implications, particularly for under-resourced areas.”
AI-ECG Comes Out Ahead
For ARISE, Lin and colleagues randomized 43,994 patients (mean age 60.2 years; 49.5% male) who presented to the emergency department or inpatient clinic with suspected acute MI and received an ECG to AI-guided (n = 21,989) or routine care (n = 22,005). The study was conducted at a single center by 20 cardiologists between May 2022 and April 2023, with randomization done by day of the week that the patient presented.
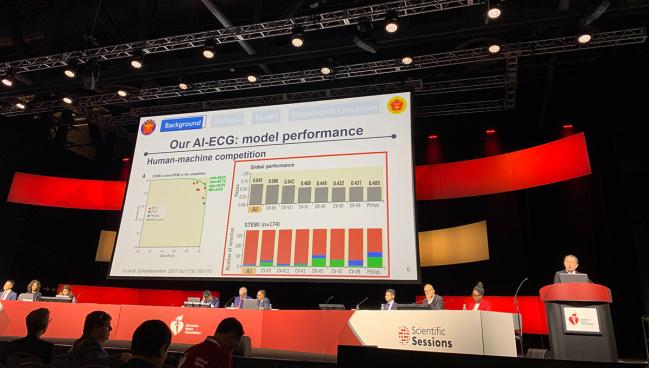
To engage the physicians with ARISE initially, Lin said they held an informal “competition” pitting the AI-tool against humans to see who could better predict STEMI in hundreds of cases. With AI coming out on top, this helped the cardiologists get on board with the technology and trial, he said.
Among the 124 patients with confirmed STEMI on coronary angiography, the primary outcome of the time from ECG to cardiac catheterization laboratory was significantly reduced by almost 10 minutes in those with treatment guided by AI compared with control (43.3 vs 52.3 minutes; P = 0.003). The findings were similar when limited to only patients who presented to the emergency department (43.0 vs 52.3 minutes) and even more robust when only patients presenting during regular working hours were analyzed (33.1 vs 61.6 minutes; P = 0.001 for both).
The algorithm performed with high positive (88%) and negative predictive values (99.9%) as well as good sensitivity (88.8%) and specificity (99.9%), Lin reported.
He acknowledged the small scale of this study and said larger, multicenter trials are needed “to further confirm the effects of AI-ECG on STEMI diagnosis and treatment.”
Nallamothu heralded the drop in ECG-to-cath-lab-door time as an “enormous improvement, particularly at an institution where they were already a high-functioning system.”
Going forward, he said, he would like to see tools like the AI-ECG be deployed and studied even earlier in the clinical pathway, perhaps in emergency medical services and prehospital systems. “There would be a lot of excitement there,” Nallamothu said.
Lastly, he commented, while the sensitivity value reported for ARISE seems promising, “getting more clarity around that will be important. Missing one out of 10 ST-elevation MIs can still be considered a big deal, and so we need to know if this is happening in particular types of patients, for example, women versus men or other groups.” As false activations of the cath lab also are a major drain on the system, Nallamothu added, the high positive predictive value seen with ARISE “is really exciting and . . . can make real inroads.”
Some Cite Limitations
While enticing, the findings are only a “proof of concept” that an AI-guided approach might be able to reduce time to STEMI treatment and ultimately improve outcomes, Khera said. This study was single center, randomized by day of the week, and broke down the accepted endpoint of door-to-balloon time “into elements that may be harder to interpret,” he said.
Harriette Van Spall, MD, MPH (McMaster University, Hamilton, Canada), who discussed the findings during the late-breaking session, agreed.
“There was a large sample randomized but very few events analyzed, which speaks to perhaps the suboptimal trial efficiency,” she said. “There was the possibility of contamination because the same 20 physicians provided care to both groups and their decision-making could override the AI-interpreted ECG.”
Van Spall also questioned the relevance of the trial’s primary outcome. “Time to balloon was not mentioned, and appropriateness of care was not evaluated,” she said. “Furthermore, clinical safety endpoints that are important when we initiate or implement care driven by AI algorithms were not discussed. The analysis was not intention to treat. It was limited to those patients who underwent urgent cardiac catheterization and had STEMI confirmed.”
Because of this, the researchers were not able to present any data on inappropriate cath lab activation or the patients who needed catheterization but never received it, she said, “potentially favoring the intervention group in the analytic path.”
The results, nonetheless, are “hypothesis generating” and “highlighted the potential benefits of AI in STEMI care,” she concluded. “There remains a critical need for well-designed trials to test the effect of AI algorithms and inform policy and practice.”
Khera, too, said he would like to see multicenter trials “assess the performance of such a strategy and not just at one really engaged center that is trying to do everything perfectly.” The AI algorithm also needs to be studied outside of Taiwan to show generalizability, he said. “But kudos to them for doing the study. You have to start somewhere.”
Yael L. Maxwell is Senior Medical Journalist for TCTMD and Section Editor of TCTMD's Fellows Forum. She served as the inaugural…
Read Full BioSources
Lin C-S. Artificial intelligence enabled rapid identification of ST-elevation myocardial infarction using electrocardiogram: a pragmatic randomized controlled trial. Presented at: AHA 2023. November 13, 2023. Philadelphia, PA.
Disclosures
- Lin reports no relevant conflicts of interest.
- Khera is an Associate Editor of JAMA. He receives support from the National Heart, Lung, and Blood Institute of the National Institutes of Health and the Doris Duke Charitable Foundation. He also receives research support, through Yale, from Bristol-Myers Squibb and Novo Nordisk. He is a coinventor of U.S. Provisional Patent Applications 63/177,117, 63/428,569, 63/346,610, 63/484,426, and 63/508,315. He is a co-founder of Ensight-AI and Evidence2Health, health platforms to improve cardiovascular diagnosis and evidence-based cardiovascular care.





Comments