COVID-19: TCTMD’s Daily Dispatch for September
We’re curating a list of COVID-19 research and other useful content, and updating it daily.

TCTMD reporter Todd Neale is keeping up on breaking news and peer-reviewed research related to COVID-19 and will update daily. If you have something to share, tell us. All of our COVID-19 coverage can be found on our COVID-19 Hub.
September 30, 2020
As the rate of positive COVID-19 tests in New York City rose above 3% for the first time in months, Mayor Bill de Blasio said the city will fine people up to $1,000 if they refuse to wear a mask in public, Reuters reports. Offenders will be offered a mask before being fined.
 Hydroxychloroquine had no clinical benefit when administered daily for 8 weeks as pre-exposure prophylaxis to hospital-based healthcare workers exposed to COVID-19 patients, according to the results of a prematurely terminated placebo-controlled trial. The PATCH results were published in JAMA Internal Medicine.
Hydroxychloroquine had no clinical benefit when administered daily for 8 weeks as pre-exposure prophylaxis to hospital-based healthcare workers exposed to COVID-19 patients, according to the results of a prematurely terminated placebo-controlled trial. The PATCH results were published in JAMA Internal Medicine.
An experimental COVID-19 vaccine called mRNA-1273, jointly developed by Moderna and the US National Institute of Allergy and Infectious Diseases (NIAID), is well tolerated and induces an immune response in older adults, according to phase I results published in the New England Journal of Medicine.
If and when a COVID-19 vaccine were to become available, the US public would support prioritized allocation based on age, risk of dying, and employment type, survey results published in JAMA Network Open show. More than 90% of respondents identified medical workers as high priority.
 Another survey in JAMA Network Open confirmed that people started drinking more alcohol during the pandemic, with an overall increase of 14% compared with baseline. Among women, heavy drinking rose by 41%, and there were indications that alcohol-related problems independent of consumption level increased for nearly one in every 10 women. “These results suggest that examination of whether increases in alcohol use persist as the pandemic continues and whether psychological and physical well-being are subsequently affected may be warranted,” the authors say.
Another survey in JAMA Network Open confirmed that people started drinking more alcohol during the pandemic, with an overall increase of 14% compared with baseline. Among women, heavy drinking rose by 41%, and there were indications that alcohol-related problems independent of consumption level increased for nearly one in every 10 women. “These results suggest that examination of whether increases in alcohol use persist as the pandemic continues and whether psychological and physical well-being are subsequently affected may be warranted,” the authors say.
Regeneron announced Tuesday that preliminary data showed that its investigational antibody cocktail called REGN-COV2 “reduced viral load and the time to alleviate symptoms in nonhospitalized patients with COVID-19.” There is an ongoing randomized, double-blind trial comparing the cocktail plus standard care with standard care alone.
According to STAT, starting tomorrow, October 1, “several private health insurers will no longer fully pay for virtual visits under certain circumstances—effectively reinstituting costs for patients reliant on the virtual care that has been heralded as a lifeline at a time when COVID-19 is still killing more than 700 Americans each day.”
 In the Mayo Clinic Proceedings, Maria Clarissa Tio, MD, and colleagues highlight the importance of the international biomedical workforce when it comes to the US response to COVID-19. “The rippling effects of the COVID-19 pandemic extend beyond their devastating health and socioeconomic impacts,” they write. “Consequent effects on evolving travel restrictions, visa sponsorships, and immigration policies can potentially add more strain to the already overburdened biomedical workforce. Since the current complexity of the immigration process is now superimposed upon a global pandemic, it is of utmost importance to ensure our international biomedical workforce is preserved.”
In the Mayo Clinic Proceedings, Maria Clarissa Tio, MD, and colleagues highlight the importance of the international biomedical workforce when it comes to the US response to COVID-19. “The rippling effects of the COVID-19 pandemic extend beyond their devastating health and socioeconomic impacts,” they write. “Consequent effects on evolving travel restrictions, visa sponsorships, and immigration policies can potentially add more strain to the already overburdened biomedical workforce. Since the current complexity of the immigration process is now superimposed upon a global pandemic, it is of utmost importance to ensure our international biomedical workforce is preserved.”
The CHA2DS2-VASc score may be useful for risk stratification in patients hospitalized with COVID-19, according to a study in the American Journal of Cardiology. Rates of in-hospital death and a composite of in-hospital death or invasive ventilation both increased across worsening tertiles of CHA2DS2-VASc score.
Creating “work bubbles” may be the way forward for businesses to reopen while limiting the risk of SARS-CoV-2 spread, according to a paper in CMAJ: “One way to balance physical distancing and the need to be at the workplace is for an employer to structure its workforce into cohorts, such that employees within a cohort interact with one another but interactions between cohorts are essentially nonexistent.”
 From August 2 to September 5, weekly COVID-19 cases among US college-age people—ages 18 to 22—increased by 55%, with the biggest jumps seen in the Northeast and Midwest, data in Morbidity and Mortality Weekly Report show. Another MMWR study describes multiple COVID-19 clusters that emerged on a North Carolina university campus within 2 weeks of opening. The issue of preventing and responding to COVID-19 on college campuses is addressed in a JAMA viewpoint by researchers from the Centers for Disease Control & Prevention (CDC), who write, “The increase in COVID-19 cases among college-age individuals underscores the urgent need to implement effective mitigation strategies, including continuing prevention efforts and robust testing paired with rapid isolation and quarantine.”
From August 2 to September 5, weekly COVID-19 cases among US college-age people—ages 18 to 22—increased by 55%, with the biggest jumps seen in the Northeast and Midwest, data in Morbidity and Mortality Weekly Report show. Another MMWR study describes multiple COVID-19 clusters that emerged on a North Carolina university campus within 2 weeks of opening. The issue of preventing and responding to COVID-19 on college campuses is addressed in a JAMA viewpoint by researchers from the Centers for Disease Control & Prevention (CDC), who write, “The increase in COVID-19 cases among college-age individuals underscores the urgent need to implement effective mitigation strategies, including continuing prevention efforts and robust testing paired with rapid isolation and quarantine.”
September 29, 2020

Two studies in JAMA Network Open examine how race is playing into the COVID-19 pandemic. One showed an association between Black race and COVID-19 positivity and need for hospitalization (but not ICU admission), and the other showed that among patients who presented for care, non-Hispanic Black and Hispanic patients did not have worse risk-adjusted outcomes compared with their white counterparts. Both “concur with other recent studies that population-level disparities in COVID-19 mortality are best explained by differential disease incidence, prevalence of comorbid conditions, and socioeconomic marginalization among Black and Hispanic individuals,” the authors of an invited commentary write.
 About 85% to 90% of Americans remain susceptible to COVID-19, signaling that the pandemic is not close to its end, according to a story in the New York Times. At the request of the newspaper, “three epidemiological teams last week calculated the percentage of the country that is infected. What they found runs strongly counter to a theory being promoted in influential circles that the United States has either already achieved herd immunity or is close to doing so, and that the pandemic is all but over.”
About 85% to 90% of Americans remain susceptible to COVID-19, signaling that the pandemic is not close to its end, according to a story in the New York Times. At the request of the newspaper, “three epidemiological teams last week calculated the percentage of the country that is infected. What they found runs strongly counter to a theory being promoted in influential circles that the United States has either already achieved herd immunity or is close to doing so, and that the pandemic is all but over.”
Children and adolescents are less susceptible to SARS-CoV-2 infection and appear to play a lesser role in spreading the virus compared with adults, according to preliminary evidence in JAMA Pediatrics. “How to interpret these data is still not clear as one fundamental question has not yet been answered,” editorialists write. “So far, the direction of spread has been difficult to elucidate in that it has been impossible to determine the relative proportion of teacher (adult)-to-child spread compared with child-to-child spread.”
Sleep patterns for kids and teens have been affected by the pandemic, and a Patient Page in JAMA Pediatrics provides guidance on how to reset sleep times as schedules get back to normal with the return of school (virtual or not): “Adjusting sleep schedules can be challenging at first and will take time to implement. Sleep is a critical part of health for children and adolescents, so make sleep a consistent priority and your child will benefit from this for years to come.
Data in Morbidity and Mortality Weekly Report show that COVID-19 incidence is about twice as high in adolescents ages 12 to 17 that it is in children ages 5 to 11. School-age children with severe outcomes from the disease more frequently had underlying conditions. “It is important for schools and communities to monitor multiple indicators of COVID-19 among school-aged children and layer prevention strategies to reduce COVID-19 disease risk for students, teachers, school staff, and families,” the authors write.
 In Pediatrics, researchers report based on US state health department data that there were 549,432 pediatric COVID-19 cases as of September 10, a rate of 729 cases per 100,000. A press release states that the number has risen to 624,890 cases as of September 24. Children are accounting for a growing proportion of COVID-19 cases as the pandemic progresses, with the percentage rising from 2.2% to 10.0% between April and September.
In Pediatrics, researchers report based on US state health department data that there were 549,432 pediatric COVID-19 cases as of September 10, a rate of 729 cases per 100,000. A press release states that the number has risen to 624,890 cases as of September 24. Children are accounting for a growing proportion of COVID-19 cases as the pandemic progresses, with the percentage rising from 2.2% to 10.0% between April and September.
Chronic use of ACE inhibitors and early introduction of low-molecular-weight heparin were associated with a reduction in in-hospital mortality among patients with COVID-19, according to data out of Italy published in the International Journal of Cardiology. Older age and the presence of cardiovascular comorbidities were tied to increased odds of dying.
Also in the International Journal of Cardiology, investigators review the pathophysiology of the prothrombotic state triggered by SARS-CoV-2 infection, the studies investigating the use of antithrombotic therapy in other viral illnesses, and the possible protective mechanisms of antithrombotics in the setting of COVID-19.
September 28, 2020
 Another paper is highlighting the severity of cardiac arrest in the COVID-19 setting. Prior to the pandemic, the proportion of patients admitted to Beaumont Health in Royal Oak, MI, who developed nonshockable rhythm in-hospital was approximately 81%, but one out of every four ultimately survived to discharge. Between March 15 and April 3, 2020, however, of the 1,309 COVID-19-positive patients admitted to the same health system who developed cardiac arrest in-hospital—with the same proportion having nonshockable rhythms—100% died. “These outcomes warrant further investigation into the risks and benefits of performing prolonged CPR in this subset of patients, especially because the resuscitation process generates aerosols that may place health care personnel at a higher risk of contracting the virus,” note the authors of the research letter, published in JAMA Internal Medicine.
Another paper is highlighting the severity of cardiac arrest in the COVID-19 setting. Prior to the pandemic, the proportion of patients admitted to Beaumont Health in Royal Oak, MI, who developed nonshockable rhythm in-hospital was approximately 81%, but one out of every four ultimately survived to discharge. Between March 15 and April 3, 2020, however, of the 1,309 COVID-19-positive patients admitted to the same health system who developed cardiac arrest in-hospital—with the same proportion having nonshockable rhythms—100% died. “These outcomes warrant further investigation into the risks and benefits of performing prolonged CPR in this subset of patients, especially because the resuscitation process generates aerosols that may place health care personnel at a higher risk of contracting the virus,” note the authors of the research letter, published in JAMA Internal Medicine.
Proning has become a cornerstone of care in severely ill COVID-19 patients with refractory hypoxemia secondary to acute respiratory distress syndrome and as a means of avoiding intubation. But ECG readings, which are particularly important with therapies known to increase the risk of rhythm disturbances, don’t look the same if ECG leads are placed on patients’ backs, researchers warn. “It is critically important to discern a prone ECG from a supine ECG to avoid misinterpretations that could lead to potentially costly and fruitless investigations,” write Henry D. Huang, MD, and colleagues in JAMA Internal Medicine.
Also writing in JAMA Internal Medicine, Benjamin K. I. Helfand, MSc, and colleagues raise alarm bells about the exclusion of older adults from COVID-19 treatment and vaccine trials. In their analysis of 232 active phase III treatment trials, 50% of the studies were “high risk” for excluding older adults. Of 18 vaccine trials analyzed, most had age cutoffs and the remainder had broad, nonspecified exclusion criteria that would effectively exclude any older adults from being enrolled. “If the older age group is excluded from vaccine trials, efforts to ensure effectiveness, titrate dosage or frequency, and assess adverse effects in the group most vulnerable to COVID-19 will not be possible,” Helfand et al conclude.
 A STAT story explores a similar theme: if people of color or from disadvantaged backgrounds volunteer for vaccine trials, what guarantee do they have that they’ll be able to get (and afford) a successful vaccine? As the article notes, “That the communities hardest hit by COVID-19 have also been woefully underrepresented in clinical trials is no coincidence, and in racing to find 30,000 participants who could represent an even broader population, pharma companies have found themselves face to face with healthcare’s deepest fault lines.”
A STAT story explores a similar theme: if people of color or from disadvantaged backgrounds volunteer for vaccine trials, what guarantee do they have that they’ll be able to get (and afford) a successful vaccine? As the article notes, “That the communities hardest hit by COVID-19 have also been woefully underrepresented in clinical trials is no coincidence, and in racing to find 30,000 participants who could represent an even broader population, pharma companies have found themselves face to face with healthcare’s deepest fault lines.”
At least 3.5% of patients with severe COVID-19 analyzed as part of the worldwide COVID Human Genetic Effort appear to have mutations in genes involved in antiviral defense, specifically the Type I interferon pathway, two papers in Science conclude (here and here). The finding may help explain why some people develop only mild symptoms, while in others the infection proves to be more serious or lethal. “It’s an unprecedented finding,” said study co-author Isabelle Meyts, MD, PhD. By testing for the presence of these antibodies, “you can almost predict who will become severely ill.”
Extracorporeal membrane oxygenation (ECMO) has been widely used in the setting of COVID-19-related acute respiratory failure, despite a dearth of evidence to support its use. Now results for 1,035 patients from 213 hospitals in 36 countries demonstrate that the use of ECMO for circulatory support is independently associated with 90-day mortality below 40% for patients with COVID-19 as well as for the subset of patients who receive respiratory (venovenous) ECMO for acute respiratory distress syndrome. Those rates are “consistent with previously reported survival rates in acute hypoxemic respiratory failure,” Ryan P. Barbaro, MD, et al write in the Lancet. “These results from hospitals experienced in providing ECMO are similar to past reports of ECMO-supported patients, with other forms of acute respiratory distress syndrome or viral pneumonia,” Barbaro is quoted in a press release. “These results support recommendations to consider ECMO in COVID-19 if the ventilator is failing.”
 Reopening universities and colleges for in-person instruction could lead to “significant” increases in COVID-19 cases in the counties where the schools are located, warn the authors of a new study. The paper, not yet peer-reviewed and published on the preprint server medRxiv, sampled 1,409 colleges—886 were conducting classes primarily in person, while 483 were primarily offering online instruction. Infection rates in the surrounding counties were then compared, both in the weeks prior to classes resuming and during the 2 weeks afterwards. “We are able to predict between 1,000 and 5,000 additional cases per day due to colleges reopening for face-to-face instruction, with our best estimate being somewhere around 3,000 cases per day or around 21,000 cases per week,” study co-author and health economist Anirban Basu, PhD, is quoted in a press release.
Reopening universities and colleges for in-person instruction could lead to “significant” increases in COVID-19 cases in the counties where the schools are located, warn the authors of a new study. The paper, not yet peer-reviewed and published on the preprint server medRxiv, sampled 1,409 colleges—886 were conducting classes primarily in person, while 483 were primarily offering online instruction. Infection rates in the surrounding counties were then compared, both in the weeks prior to classes resuming and during the 2 weeks afterwards. “We are able to predict between 1,000 and 5,000 additional cases per day due to colleges reopening for face-to-face instruction, with our best estimate being somewhere around 3,000 cases per day or around 21,000 cases per week,” study co-author and health economist Anirban Basu, PhD, is quoted in a press release.
A study of remainder plasma from more than 28,500 randomly selected patients who underwent dialysis at one of 1,300 US facilities in July uncovered a seroprevalence rate of 8%. Standardized to the US adult population, this rate rose to 9.3% overall and was lowest in the west at 3.5% but as high as 27.2% in the northeast. Many patients receiving dialysis in the United States “share the socioeconomic characteristics of underserved communities,” say the authors, explaining the importance of this sample source. Limiting the spread of SARS-CoV-2 should include efforts to especially target racial and ethnic minority and densely populated communities, they conclude, noting that their results suggest that fewer than 10% of the US adult population formed antibodies against the virus and fewer than 10% of those with antibodies were diagnosed. The paper was published in the Lancet last week.
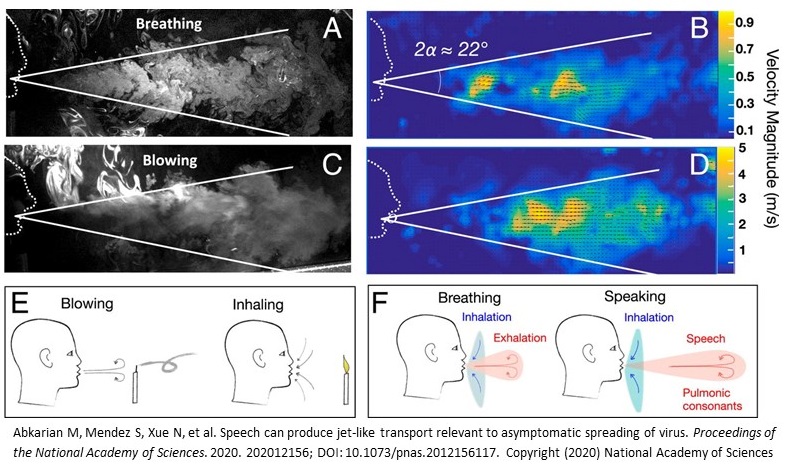
Researchers writing in PNAS have analyzed the aerodynamic flow of droplets during breathing and speaking according to phonetic features. Certain sounds and letters produce different airflow that would carry different risks. For example, “plosive sounds like ‘P’ lead to significantly enhanced directed transport, including jet-like flows that entrain the surrounding air,” they write. “With social situations in mind, in hindsight, it should perhaps not be surprising that droplet and aerosol generation and possible virus transmission are enhanced during rapid and excited speech during parties, singing events, etc.” A series of mesmerizing videos shows the different airflow patterns as a person breathes, blows, then speaks the sentences: “We will beat the corona virus,” “Sing a song of six pence,” and “Peter Piper picked a peck.”
Today’s Dispatch was contributed by Shelley Wood.
September 25, 2020
 Patients who have an in-hospital cardiac arrest during the COVID-19 pandemic have worse survival compared with those who had an in-hospital cardiac arrest last year (3% vs 13%), data from a single hospital in New York City suggest. In-hospital arrests during the pandemic also occurred more often on general medicine wards than in ICUs, were shorter in duration, and led to fewer endotracheal intubations, according to a study published in Circulation: Cardiovascular Quality and Outcomes.
Patients who have an in-hospital cardiac arrest during the COVID-19 pandemic have worse survival compared with those who had an in-hospital cardiac arrest last year (3% vs 13%), data from a single hospital in New York City suggest. In-hospital arrests during the pandemic also occurred more often on general medicine wards than in ICUs, were shorter in duration, and led to fewer endotracheal intubations, according to a study published in Circulation: Cardiovascular Quality and Outcomes.
GI complications, including mesenteric ischemia, are more common in critically ill patients with versus without COVID-19, researchers report in JAMA. “High expression of angiotensin-converting enzyme 2 receptors along the epithelial lining of the gut that act as host-cell receptors for SARS-CoV-2 could explain involvement of abdominal organs,” the authors say. “Higher opioid requirements and COVID-19–induced coagulopathy may also explain the disproportionately high rate of ileus and ischemic bowel disease.”
A study in Scientific Reports provides insights into the efficacy of various types of masks and face coverings in controlling emission of aerosols. “These observations directly demonstrate that wearing of surgical masks or KN95 respirators, even without fit-testing, substantially reduce the number of particles emitted from breathing, talking, and coughing,” the researchers write. “While the efficacy of cloth and paper masks is not as clear and confounded by shedding of mask fibers, the observations indicate it is likely that they provide some reductions in emitted expiratory particles, in particular the larger particles (> 0.5 μm).”
 Head-to-head comparisons of 10 commercial antibody kits for determining previous infection with SARS-CoV-2 showed “a broad range of performance among the tests, but all gave the best results when used 20 days or more after the start of symptoms,” researchers report in PLOS Pathogens. “Furthermore, antibody levels were higher in individuals with severe illness compared to those with asymptomatic or mild disease.”
Head-to-head comparisons of 10 commercial antibody kits for determining previous infection with SARS-CoV-2 showed “a broad range of performance among the tests, but all gave the best results when used 20 days or more after the start of symptoms,” researchers report in PLOS Pathogens. “Furthermore, antibody levels were higher in individuals with severe illness compared to those with asymptomatic or mild disease.”
The phase II HESACOVID trial, which included 20 COVID-19 patients requiring mechanical ventilation, showed that therapeutic enoxaparin improved gas exchange relative to standard anticoagulant thromboprophylaxis and reduced the need for mechanical ventilation, according to findings published in Thrombosis Research.
A study of 1,392 patients with COVID-19 admitted to a tertiary teaching hospital in China, published in the Clinical Journal of the American Society of Nephrology, shows that 7% developed acute kidney injury (AKI) during the hospitalization. The odds of dying in the hospital were higher in those with AKI (OR 5.12). The in-hospital mortality rates were 62%, 77%, and 80% in patients with AKI stages 1, 2, and 3, respectively.
 “Black and Hispanic individuals are experiencing an excess burden of SARS-CoV-2 infection not entirely explained by underlying medical conditions or where they live or receive care,” according to a recent study in PLOS Medicine based on data from the US Department of Veterans Affairs. Thirty-day mortality did not differ by race/ethnicity, however. “Understanding what is driving these disparities is vital so that strategies can be tailored to curb the disproportionate epidemics in minority communities,” the lead author said in a press release.
“Black and Hispanic individuals are experiencing an excess burden of SARS-CoV-2 infection not entirely explained by underlying medical conditions or where they live or receive care,” according to a recent study in PLOS Medicine based on data from the US Department of Veterans Affairs. Thirty-day mortality did not differ by race/ethnicity, however. “Understanding what is driving these disparities is vital so that strategies can be tailored to curb the disproportionate epidemics in minority communities,” the lead author said in a press release.
Researchers in Seattle found a higher burden of SARS-CoV-2 infection among non-English-speaking patients there, according to a study in JAMA Network Open. Despite the availability of interpreter services across locations, people in these groups were less likely to be tested for COVID-19 compared with English speakers.
Hydroxychloroquine is safe from an arrhythmia perspective for short-term treatment of patients with COVID-19, irrespective of clinical setting, researchers report in EP Europace. In the study, the drug caused “only modest QT prolongation” and no arrhythmic deaths.
 A perspective in the New England Journal of Medicine highlights the role community health works can play during the pandemic. “Investing in community health workers and community-based organizations can help address the social determinants of poor health that disproportionately affect low-income, minority populations and that are magnified during times of crisis,” the authors say.
A perspective in the New England Journal of Medicine highlights the role community health works can play during the pandemic. “Investing in community health workers and community-based organizations can help address the social determinants of poor health that disproportionately affect low-income, minority populations and that are magnified during times of crisis,” the authors say.
September 24, 2020
AstraZeneca is still waiting for the FDA to allow the company’s COVID-19 vaccine trial to resume after being halted for 3 weeks due to safety concerns, Reuters reports. One participant developed a serious adverse event, believed to be a spinal inflammatory disorder called transverse myelitis, and regulators are continuing to investigate the issue.
 Due to disruptions related to COVID-19, the Centers for Medicare & Medicaid Services (CMS) will not hold hospitals and physicians responsible for meeting volume requirements mandated for reimbursement for TAVR, transcatheter mitral valve repair, percutaneous left atrial appendage closure, and ventricular assist devices as long as the standards were being met prior to the pandemic. “I think they’re being quite reasonable,” John Carroll, MD, told TCTMD.
Due to disruptions related to COVID-19, the Centers for Medicare & Medicaid Services (CMS) will not hold hospitals and physicians responsible for meeting volume requirements mandated for reimbursement for TAVR, transcatheter mitral valve repair, percutaneous left atrial appendage closure, and ventricular assist devices as long as the standards were being met prior to the pandemic. “I think they’re being quite reasonable,” John Carroll, MD, told TCTMD.
Eric Topol, MD, goes over the cardiovascular impact of COVID-19 in a perspective in Science. “Clearly, it is more common than anticipated, but the true incidence is unknown,” Topol writes. “It is vital to determine what drives this pathogenesis. Whether it represents an individual’s inflammatory response, an autoimmune phenomenon, or some other explanation needs to be clarified.”
Myocardial injury is common in patients with COVID-19 pneumonia, a study in the International Journal of Cardiology affirms, occurring in 50% of nonsurvivors and just 6% of survivors. Predictors of mortality included elevated D-dimer, CK-MB, troponin I, and C-reactive protein levels.
 The age distribution of COVID-19 cases is changing as the pandemic progresses, according to a study in Morbidity and Mortality Weekly Report. Although incidence early on was highest in older adults, between June and August incidence was highest in people in their 20s, who accounted for more than 20% of confirmed cases.
The age distribution of COVID-19 cases is changing as the pandemic progresses, according to a study in Morbidity and Mortality Weekly Report. Although incidence early on was highest in older adults, between June and August incidence was highest in people in their 20s, who accounted for more than 20% of confirmed cases.
The design paper for the INSPIRATION and INSPIRATION-S trials evaluating prophylactic anticoagulation and statins in critically ill patients with COVID-19, published in Thrombosis Research, provides a summary of several additional ongoing randomized studies of those interventions. “Although others have sparsely discussed them, to the best of my knowledge, a systematic summary of those studies has not been provided elsewhere,” the lead author of the paper told TCTMD.
In a socioeconomically deprived, urban population in the United Kingdom, diagnoses of common mental health problems dropped by 50.0% between March and May 2020, with similar declines seen in diagnoses for circulatory system diseases (43.3%) and type 2 diabetes (49.0%). The number of first prescriptions for associated medications fell, too. The findings were presented at the ESCMID Conference on Coronavirus Diseases (ECCVID) and published in the Lancet Public Health.
 A study in JAMA Network Open shows that elevated red blood cell distribution width (RDW) and an increase in RDW during hospitalization are associated with a heightened mortality risk in patients with SARS-CoV-2 infection. Measuring RDW may be useful for risk stratification, the authors say.
A study in JAMA Network Open shows that elevated red blood cell distribution width (RDW) and an increase in RDW during hospitalization are associated with a heightened mortality risk in patients with SARS-CoV-2 infection. Measuring RDW may be useful for risk stratification, the authors say.
Another study in that journal, based on US Department of Veterans Affairs data, showed that most SARS-CoV-2 deaths were associated with older age, male sex, and comorbidities. “Many factors previously reported to be associated with mortality in smaller studies were not confirmed, such as obesity, Black race, Hispanic ethnicity, chronic obstructive pulmonary disease, hypertension, and smoking,” the researchers note.
The US Food and Drug Administration issued an emergency use authorization (EUA) for the first antibody test for COVID-19 that can be used at the point of care (the Assure COVID-19 IgG/IgM Rapid Test Device), posted a document that provides updated evidence supporting the emergency use of convalescent plasma to treat COVID-19, and revoked the umbrella EUA for infusion pumps. “The FDA has determined that circumstances support revocation, and that individual EUAs will allow for tailored indications and scopes of authorization,” the agency said.
In addition, FDA Commissioner Stephen Hahn, MD, along with other senior public health officials, testified before the Senate Committee on Health, Education, Labor, and Pensions to provide an update on the federal response to the pandemic (video here).
 Among pregnant women, a positive SARS-CoV-2 result was associated with a higher prevalence of preeclampsia and a lower prevalence of induced labor, researchers report in JAMA. There were no relationships between the infection and preterm delivery or various infant outcomes.
Among pregnant women, a positive SARS-CoV-2 result was associated with a higher prevalence of preeclampsia and a lower prevalence of induced labor, researchers report in JAMA. There were no relationships between the infection and preterm delivery or various infant outcomes.
September 23, 2020
The COVID-19 death toll has reached 200,000 in the United States, as reported by Reuters and others. According to the Johns Hopkins COVID-19 Dashboard, 200,818 Americans have died, with the global tally approaching 1 million (971,915).
JAMA is looking back on the COVID-19 literature that has accumulated since the beginning of the pandemic in a series of 13 viewpoints covering various fields of medicine. In the one discussing cardiology, Robert Bonow, MD, Patrick O’Gara, MD, and Clyde Yancy, MD, say that “the generation of rigorous evidence to inform best practices for diagnosis and management of COVID-19–related cardiovascular disease is a global imperative.”
 Applications to medical school are up during the COVID-19 era, according to a story in the Wall Street Journal: “Through the end of August, the number of applicants rose nearly 17% from a year earlier, marking an interest not seen in more than a decade, according to the Association of American Medical Colleges.”
Applications to medical school are up during the COVID-19 era, according to a story in the Wall Street Journal: “Through the end of August, the number of applicants rose nearly 17% from a year earlier, marking an interest not seen in more than a decade, according to the Association of American Medical Colleges.”
A fourth large-scale COVID-19 vaccine trial, evaluating Janssen’s candidate, has begun enrolling adult volunteers, the US National Institutes of Health (NIH) announced. The study will include up to 60,000 participants from up to 215 research sites in the US and elsewhere.
The NIH also announced that two randomized trials evaluating convalescent plasma for the treatment of COVID-19 are expanding enrollment.
Asymptomatic patients with SARS-CoV-2 infection carry a viral load similar to that seen in symptomatic patients, according to research in Thorax. They “may thus act as a meaningful driving force for the community spread of COVID-19,” the authors say.
A “living systematic review” published in PLOS Medicine suggests that most people who become infected (80%) will not remain asymptomatic throughout the course of the infection. “The contribution of presymptomatic and asymptomatic infections to overall SARS-CoV-2 transmission means that combination prevention measures, with enhanced hand hygiene, masks, testing tracing, and isolation strategies and social distancing, will continue to be needed,” the researchers conclude.
 A Brazilian trial showed that adding azithromycin to standard treatment, which included hydroxychloroquine, did not improve clinical status at day 15 compared with standard treatment alone in patients hospitalized with severe COVID-19. The findings were presented at the ESCMID Conference on Coronavirus Diseases (ECCVID) and published in the Lancet.
A Brazilian trial showed that adding azithromycin to standard treatment, which included hydroxychloroquine, did not improve clinical status at day 15 compared with standard treatment alone in patients hospitalized with severe COVID-19. The findings were presented at the ESCMID Conference on Coronavirus Diseases (ECCVID) and published in the Lancet.
In a JAMA viewpoint, three former editors in chief for Morbidity and Mortality Weekly Report (MMWR), published by the Centers for Disease Control & Prevention (CDC), argue that the editorial independence of the publication must be protected from political meddling. This comes in response to reports that “political appointees within the US Department of Health and Human Services (HHS) have demanded the ability to review and revise scientific reports” on COVID-19.
Improvements are needed in contact tracing, a MMWR report indicates. In two counties in North Carolina, 35% to 48% of COVID-19 patients reported no contacts and 25% to 48% of contacts could not be reached.
The US Food and Drug Administration (FDA) is expected to toughen standards for any emergency authorization of a COVID-19 vaccine in order to boost public trust, according to a story in the Washington Post: “Public health experts are increasingly worried that President Trump’s repeated predictions of a coronavirus vaccine by Nov. 3, coupled with the administration’s interference in federal science agencies, may prompt Americans to reject any vaccine as rushed and potentially tainted.”
 If it were up to the CDC, you wouldn’t go trick-or-treating on Halloween this year, Reuters reports. The agency has updated its guidance on holiday celebrations during the pandemic, listing door-to-door candy gathering and indoor costume parties—among other things—as higher-risk activities.
If it were up to the CDC, you wouldn’t go trick-or-treating on Halloween this year, Reuters reports. The agency has updated its guidance on holiday celebrations during the pandemic, listing door-to-door candy gathering and indoor costume parties—among other things—as higher-risk activities.
September 22, 2020
 The United Kingdom’s COVID-19 alert level is being upgraded from 3 to 4, which means that transmission of SARS-CoV-2 is “high or rising exponentially,” BBC reports. UK Health and Social Care Secretary Matt Hancock said, “This country now faces a tipping point in its response and it is vital everybody plays their part now to stop the spread of the virus and protect lives.”
The United Kingdom’s COVID-19 alert level is being upgraded from 3 to 4, which means that transmission of SARS-CoV-2 is “high or rising exponentially,” BBC reports. UK Health and Social Care Secretary Matt Hancock said, “This country now faces a tipping point in its response and it is vital everybody plays their part now to stop the spread of the virus and protect lives.”
Countries encompassing nearly two-thirds of the world population have signed on to a COVID-19 vaccine initiative led by the World Health Organization, called COVAX, STAT reports. The WHO aims to buy 2 billion doses of potential COVID-19 vaccines by the end of next year for use by all countries. Notably absent from the list of participants, which includes 64 high-income countries, are the United States, Russia, and China.
In a blog post, US National Institutes of Health (NIH) Director Francis Collins, MD, PhD, discusses recent research exploring the origins of the SARS-CoV-2 outbreaks in Europe and North America. The findings “show that the chain of transmission from China to Italy to New York City sparked outbreaks on the East Coast slightly later in February than those that spread from China directly to Washington state,” he writes. “It confirms that the Seattle outbreak was indeed the first, predating others on the East Coast and in California.”
Days after adding it, the US Centers for Disease Control and Prevention (CDC) removed guidance highlighting the role of airborne transmission from its website, saying a draft version of the proposed changes was posted in error. “Experts with knowledge of the incident said on Monday that the latest reversal appeared to be a genuine mistake in the agency’s scientific review process, rather than the result of political meddling. Officials said the agency would soon publish revised guidance,” according to a story in the New York Times.
 The immune responses to SARS-CoV-2 infection differ between hospitalized pediatric and adult patients, according to a study in Science Translational Medicine, and that might explain why children and adolescents fare better. “The suggestion is that kids have a more robust, earlier innate immune response to the virus, which may protect them from progressing to severe pulmonary disease,” the senior author said in a press release.
The immune responses to SARS-CoV-2 infection differ between hospitalized pediatric and adult patients, according to a study in Science Translational Medicine, and that might explain why children and adolescents fare better. “The suggestion is that kids have a more robust, earlier innate immune response to the virus, which may protect them from progressing to severe pulmonary disease,” the senior author said in a press release.
Cardiac manifestations are prevalent in previously healthy children who develop the multisystem inflammatory syndrome (MIS-C) associated with SARS-CoV-2 infection, data on 55 patients from an international cohort indicate. Published in the Journal of the American Heart Association, the results show that 64% had decreased LV function, 31% had valvulitis, 22% had pericardial effusion, and 20% had coronary abnormalities. Nearly half (49%) required ICU admission and 44% had evidence of shock.
The US Food and Drug Administration (FDA) has updated the question-and-answer section of its guidance on conducting clinical trials during the COVID-19 public health emergency, providing new information on “a clinical trial investigator's responsibility to review all investigational new drug application safety reports, including reports that will not result in a change to the investigator brochure, informed consent, or protocol.”

Researchers underscore the need to ensure adequate palliative and hospice care during spikes in COVID-19 activity in a JAMA viewpoint, saying that “surges in demand for end-of-life care have exposed and exacerbated underlying gaps in access to specialty-trained physicians and teams, palliative care medications, and bereavement support for patients and families.”
The COVID-19 pandemic is worsening the impact of human trafficking, researchers say in a JAMA Pediatrics viewpoint: “The virus has disrupted [survivors’] lives and support networks while increasing financial stress, food insecurity, interpersonal violence, and grief over the loss of loved ones.”
A public affairs officer from the National Institute of Allergy and Infectious Diseases (NIAID) will be allowed to retire after it was discovered that he had been attacking NIAID Director Anthony Fauci, MD, while writing under a pseudonym for RedState, a conservative website. The story was broken by the Daily Beast.
September 21, 2020
The US Centers for Disease Control and Prevention (CDC) updated its guidance on how SARS-CoV-2 spreads last week, underscoring that the virus is airborne and is thought to be mainly spread by aerosols produced when a person coughs, sneezes, sings, talks, or breathes. Risk of spread is higher in indoor environments without good ventilation, the agency says.
 The CDC also reversed its controversial changes to testing guidance, which indicated that people who had been within 6 feet of someone with COVID-19 for at least 15 minutes did not necessarily need to be tested for infection if they didn’t have symptoms. In an update posted Friday, the agency now says: “Due to the significance of asymptomatic and presymptomatic transmission, this guidance further reinforces the need to test asymptomatic persons, including close contacts of a person with documented SARS-CoV-2 infection.”
The CDC also reversed its controversial changes to testing guidance, which indicated that people who had been within 6 feet of someone with COVID-19 for at least 15 minutes did not necessarily need to be tested for infection if they didn’t have symptoms. In an update posted Friday, the agency now says: “Due to the significance of asymptomatic and presymptomatic transmission, this guidance further reinforces the need to test asymptomatic persons, including close contacts of a person with documented SARS-CoV-2 infection.”
Within the large Mayo Clinic health system, the pandemic was associated with a 50% drop in emergency department visits, with declines in the numbers of patients diagnosed with MI, stroke, appendicitis, and cholecystitis, according to data in the Mayo Clinic Proceedings. The proportion of visits for mental health complaints increased, as did the number of deaths, driven by out-of-hospital mortality.
A nationally representative study in Science Advances shows that between March 18 and April 18, 2020, when COVID-19 activity was ramping up in the United States, acute stress and depressive symptoms increased significantly. Preexisting mental and physical health diagnoses, daily hours of COVID-19-related media exposure, exposure to conflicting COVID-19 information in the media, and secondary stressors were associated with these symptoms.
 The National Medical Association (NMA), a group created in the late 19th century to represent African-American physicians and their patients, has created a task force to scrutinize government decisions around COVID-19 treatments and vaccines and recommendations for managing the pandemic, STAT reports. “It’s necessary to provide a trusted messenger of vetted information to the African-American community,” NMA President Leon McDougle, MD, said. “There is a concern that some of the recent decisions by the Food and Drug Administration have been unduly influenced by politicians.”
The National Medical Association (NMA), a group created in the late 19th century to represent African-American physicians and their patients, has created a task force to scrutinize government decisions around COVID-19 treatments and vaccines and recommendations for managing the pandemic, STAT reports. “It’s necessary to provide a trusted messenger of vetted information to the African-American community,” NMA President Leon McDougle, MD, said. “There is a concern that some of the recent decisions by the Food and Drug Administration have been unduly influenced by politicians.”
The FDA has reissued the emergency use authorization for the Abbott ID Now COVID-19 test. Among other changes, the update specifies that testing is for specimens collected from individuals with suspected COVID-19 within the first 7 days of symptom onset.
COVID-19 patients with an elevated D-dimer level have a heightened risk of a composite of all-cause mortality, ICU admission, and acute respiratory distress syndrome, according to a meta-analysis in Heart & Lung. “Further studies are required to assess if the serial measurement of D-dimer plays any role in predicting evolution towards a more critical form of disease,” the authors say.
Two studies in JAMA—one looking at urine drug test positivity and the other at nonfatal opioid overdoses at an urban emergency department—“are consistent with the hypothesis that the US COVID-19 epidemic has been accompanied by an increase in substance use with important consequences (nonfatal overdose), with a signal of greater effect among people who are Black,” according to an accompanying editorial.
 An editorial in JAMA Internal Medicine tackles what is known so far—and what questions remain—regarding severe COVID-19 cases involving acute respiratory distress syndrome. “Uncertainty remains about the reasons that some patients develop respiratory failure and others have no to minimal symptoms, as well as about the optimal management of patients with severe COVID-19 disease,” the authors say.
An editorial in JAMA Internal Medicine tackles what is known so far—and what questions remain—regarding severe COVID-19 cases involving acute respiratory distress syndrome. “Uncertainty remains about the reasons that some patients develop respiratory failure and others have no to minimal symptoms, as well as about the optimal management of patients with severe COVID-19 disease,” the authors say.
September 18, 2020
Dexamethasone can be considered a treatment option for COVID-19 patients who require any type of oxygen therapy ranging from supplemental oxygen to mechanical ventilation, the European Medicines Agency (EMA) has concluded, based on its review of the RECOVERY study results. The recommended dose in adolescents and adults is 6 mg/day for up to 10 days.
 US catheterization laboratories saw an “unprecedented” drop in cardiovascular interventions at the height of the COVID-19 pandemic and those deferred procedures tracked with regional COVID-19 burden, according to the results of a nationwide survey published in Catheterization & Cardiovascular Interventions. “What concerns me most about our findings is that patients may inappropriately be deferring lifesaving procedures, out of fear of the COVID-19, to the point that it's a detriment to their health,” the lead author told TCTMD Managing Editor Shelley Wood.
US catheterization laboratories saw an “unprecedented” drop in cardiovascular interventions at the height of the COVID-19 pandemic and those deferred procedures tracked with regional COVID-19 burden, according to the results of a nationwide survey published in Catheterization & Cardiovascular Interventions. “What concerns me most about our findings is that patients may inappropriately be deferring lifesaving procedures, out of fear of the COVID-19, to the point that it's a detriment to their health,” the lead author told TCTMD Managing Editor Shelley Wood.
A JAMA research letter shows that levels of anti-SARS-CoV-2 antibodies to the spike protein, which have been associated with neutralizing antibodies, declined over a period of 60 days among healthcare workers recovering from the infection. Over that time, 58% of seropositive individuals became seronegative. “Implications for healthcare personnel with antibodies assigned to care for infected patients depend on whether decline in these antibodies increases risk of reinfection and disease, which remains unknown, especially given the lack of data on memory B-cell and T-cell responses,” the authors say.
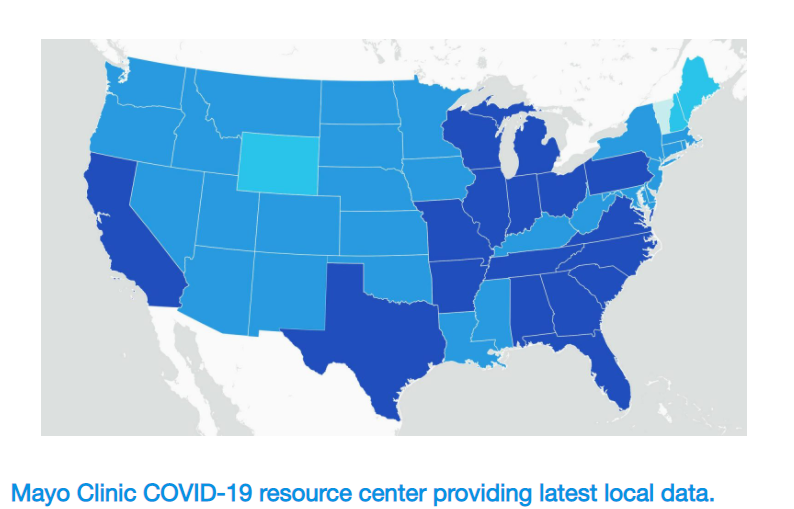 The Mayo Clinic has launched a COVID-19 tracking tool that provides county-level data for the United States. “This map presents key data and trends in an easy-to-use format. Data include the total number of cases by county and state, new cases per day, [and] positive test rate and fatality rate, presented with trends over time and Mayo Clinic guidance on how to take action,” according to a press release.
The Mayo Clinic has launched a COVID-19 tracking tool that provides county-level data for the United States. “This map presents key data and trends in an easy-to-use format. Data include the total number of cases by county and state, new cases per day, [and] positive test rate and fatality rate, presented with trends over time and Mayo Clinic guidance on how to take action,” according to a press release.
A consortium called Reliable Response Data Discovery (R2D2), encompassing 202 hospitals across 12 health systems in California, Colorado, Texas, and Germany, has launched COVID19questions.org. The website invites clinicians, researchers, patients, and the general public to submit questions that can be answered by COVID-19 patient record data from the participating health systems. After the analyses are performed, the answers are posted on the site.
Carotid CT angiography for the evaluation of acute stroke may also provide information about COVID-19, according to a study in the American Journal of Neuroradiology. Such imaging covers the lung apices, and the presence of apical ground-glass opacification had good diagnostic performance for COVID-19. The finding was also independently associated with increased 30-day mortality. “Our findings have important implications in the management of patients presenting with suspected stroke through early identification of COVID-19 and the subsequent limitation of disease transmission,” the authors say.

A review in the Annals of Internal Medicine covers what is known about the transmission of SARS-CoV-2, and states, “Strong evidence from case and cluster reports indicates that respiratory transmission is dominant, with proximity and ventilation being key determinants of transmission risk.” There is little evidence to support a major contribution from coming into contact with contaminated surfaces.
Measures to control SARS-CoV-2 transmission are likely to cut influenza activity as well, a study in Morbidity and Mortality Weekly Report indicates. Following adoption of such measures, the percentage of US respiratory specimens submitted for influenza testing that tested positive dropped from more than 20% to 2.3% and has since remained at “historically low” levels. Similar findings came from Australia, Chile, and South Africa.
The COVID-19 pandemic has been associated with a decline in the proportion of female corresponding authors in preprint research, researchers report in JAMA Network Open. In medRxiv, the preprint server for health sciences, the gender gap—with women accounting for a lower percentage of corresponding authors—increased this year from 23% in January to 55% in April. No such change was seen in bioRxiv, the preprint service for life sciences, although the gender gap remained large at 47%.
A JAMA viewpoint explores whether a “medical malpractice crisis” may be brewing as the COVID-19 pandemic continues. “The history of medical malpractice suggests that a much larger medical liability problem may be on the horizon, if shifts in global insurance markets compound financial stresses among purchasers of malpractice coverage,” the authors write.
Findings presented during the virtual European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Conference on Coronavirus Disease indicated that more than half of patients who recovered from COVID-19 had persistent fatigue a median of 10 weeks following clinical recovery, regardless of the severity of the initial infection.
 Another study presented during that meeting suggests that a substantial proportion of cats and dogs are infected with SARS-CoV-2 by their owners. “All cats with an indeterminate PCR or positive antibody result were reported to have had respiratory and/or other illness by their owners around the time of the owner's COVID-19 infection,” the researcher said in a press release. “Two (20%) of dogs had positive IgG antibody results, indicating past infection, and one of these was reported to have had an episode of respiratory disease. No dogs had positive IgM results, which would have indicated more recent infection.”
Another study presented during that meeting suggests that a substantial proportion of cats and dogs are infected with SARS-CoV-2 by their owners. “All cats with an indeterminate PCR or positive antibody result were reported to have had respiratory and/or other illness by their owners around the time of the owner's COVID-19 infection,” the researcher said in a press release. “Two (20%) of dogs had positive IgG antibody results, indicating past infection, and one of these was reported to have had an episode of respiratory disease. No dogs had positive IgM results, which would have indicated more recent infection.”
September 17, 2020
Robert Redfield, MD, director of the Centers for Disease Control and Prevention (CDC), told US lawmakers yesterday that wearing a mask may provide more protection than would a potential COVID-19 vaccine, CNBC reports. After receiving criticism from President Donald Trump, however, Redfield posted on Twitter that “I 100% believe in the importance of vaccines and the importance in particular of a COVID-19 vaccine. A COVID-19 vaccine is the thing that will get Americans back to normal everyday life.”
I 100% believe in the importance of vaccines and the importance in particular of a #COVID19 vaccine. A COVID-19 vaccine is the thing that will get Americans back to normal everyday life.
— Dr. Robert R. Redfield (@CDCDirector) September 16, 2020
In an interview on CNBC’s “Squawk Box”, Modern’s CEO said that as of November, the company should have enough data to know whether its COVID-19 vaccine works. “If the infection rate in the country were to slow down in the next weeks, it could potentially be pushed out in a worst-case scenario in December,” he added.
Researchers argue in a JAMA viewpoint that the US Occupational Safety and Health Administration (OSHA) can be doing more to protect workers, their families, and the community against COVID-19. “The most important action the federal government could take is for OSHA to issue an Emergency Temporary Standard (ETS) that would require every employer to develop and implement an infection control plan,” they say.
Two studies in Morbidity and Mortality Weekly Report provide insights into how COVID-19 affects hospitalized pregnant women. One showed that severe illness could occur in symptomatic women, including the need for ICU care (16%), mechanical ventilation (8%), and death (1%). The other showed that 30% of women admitted for COVID-19 required ICU care, and one died. “Antenatal counseling emphasizing preventive measures, including use of masks, frequent hand washing, and social distancing, might help prevent COVID-19 among pregnant women, especially those with prepregnancy obesity and gestational diabetes,” the authors of the latter report say.
 Another JAMA viewpoint tackles why the United States has offered a “suboptimal” response to COVID-19 despite having ample resources at its disposal. “During the years to come, the US undoubtedly will undergo national-level reviews to understand how its strong capabilities were squandered when the country needed them the most,” the authors write.
Another JAMA viewpoint tackles why the United States has offered a “suboptimal” response to COVID-19 despite having ample resources at its disposal. “During the years to come, the US undoubtedly will undergo national-level reviews to understand how its strong capabilities were squandered when the country needed them the most,” the authors write.
On Wednesday, the US National Institutes of Health (NIH) announced a $12 million award to RTI International, a nonprofit research institution, for outreach and engagement efforts in racial/ethnic minority communities, which have been particularly hard hit by the COVID-19 pandemic.
Three rapid Cochrane reviews indicate that quarantine is key to reducing incidence and mortality during the pandemic, travel-related control measures may have had a positive impact, and screening of healthy people may miss some who are infected or falsely identify others as positive. “Given the poor sensitivity of existing approaches, our findings point to the need for greater emphasis on other ways that may prevent transmission such as face coverings, physical distancing, quarantine, and adequate personal protective equipment for frontline workers,” the authors of the screening review state.
 Data out of China, published in JAMA Ophthalmology, suggest that daily wearers of eyeglasses may be less susceptible to COVID-19. “Although it is tempting to conclude from this study that everyone should wear eyeglasses, goggles, or a face shield in public to protect their eyes and themselves from COVID-19, from an epidemiological perspective, we must be careful to avoid inferring a causal relationship from a single observational study,” Lisa Maragakis, MD, cautions in an invited commentary.
Data out of China, published in JAMA Ophthalmology, suggest that daily wearers of eyeglasses may be less susceptible to COVID-19. “Although it is tempting to conclude from this study that everyone should wear eyeglasses, goggles, or a face shield in public to protect their eyes and themselves from COVID-19, from an epidemiological perspective, we must be careful to avoid inferring a causal relationship from a single observational study,” Lisa Maragakis, MD, cautions in an invited commentary.
September 16, 2020
 In response to research showing that cardiac magnetic resonance (CMR) imaging picks up signs of cardiac damage and myocarditis in athletes and others infected with COVID-19, an international group of physicians has signed on to an ‘open letter’ sent to cardiovascular societies in the United States and Europe calling for “clear guidance discouraging CMR screening for COVID-19-related heart abnormalities in asymptomatic members of the general public.” To TCTMD Managing Editor Shelley Wood, Venkatesh Murthy, MD, PhD, explained that the letter was motivated by the fact that he and others “have begun to receive requests to perform CMR in asymptomatic individuals post-COVID.” The Society for Cardiovascular Magnetic Resonance and the American College of Cardiology have provided responses to the letter to TCTMD.
In response to research showing that cardiac magnetic resonance (CMR) imaging picks up signs of cardiac damage and myocarditis in athletes and others infected with COVID-19, an international group of physicians has signed on to an ‘open letter’ sent to cardiovascular societies in the United States and Europe calling for “clear guidance discouraging CMR screening for COVID-19-related heart abnormalities in asymptomatic members of the general public.” To TCTMD Managing Editor Shelley Wood, Venkatesh Murthy, MD, PhD, explained that the letter was motivated by the fact that he and others “have begun to receive requests to perform CMR in asymptomatic individuals post-COVID.” The Society for Cardiovascular Magnetic Resonance and the American College of Cardiology have provided responses to the letter to TCTMD.
A news story in Science details the effort underway to understand how COVID-19 affects the heart and further explore the preliminary CMR data.
Data in Morbidity and Mortality Weekly Report provide insights into SARS-CoV-2-related deaths in people younger than 21. Of 121 such cases, 10% were infants and 70% were people ages 10 to 20. Most of the deaths (78%) occurred in Hispanic, non-Hispanic Black, and non-Hispanic American Indian/Alaskan Native individuals.
The US Food and Drug Administration (FDA) has published comparative performance data for COVID-19 molecular diagnostic tests, providing information on the limit of detection for more than 55 authorized products.
 Statin use in the 30 days prior to hospitalization is associated with a reduced risk of severe COVID-19 and faster time to recovery among those without severe disease, suggests a retrospective study in the American Journal of Cardiology.
Statin use in the 30 days prior to hospitalization is associated with a reduced risk of severe COVID-19 and faster time to recovery among those without severe disease, suggests a retrospective study in the American Journal of Cardiology.
A meta-analysis in Resuscitation using data from France, Italy, and the United States affirms that the odds of out-of-hospital cardiac arrest—as well as related mortality—increased during the pandemic. “COVID-19 related hyperinflammatory state leading to the high propensity of fatal arrhythmia, atherosclerotic plaque destabilization, thromboembolic state, and myocardial injury could be a leading factor for OHCA in these patients,” the authors write.
A review in the European Heart Journal – Cardiovascular Pharmacotherapy describes the safety of drug treatment for COVID-19 in pregnant women treated with antihypertensive therapy. The conclusion? “The current indications for the management of hypertension-related disorders in pregnancy maintain their validity, while the risk of pharmacological interaction with the currently tested anti-SARS-CoV-2 medications is relatively low.”
 A perspective in the New England Journal of Medicine discusses how the pharmaceutical industry’s caution is bumping up against the US government’s efforts to accelerate development of COVID-19 vaccines. That represents something of a reversal of roles compared with normal times, when regulators have been accused of acting too slowly and demanding too much evidence before approving new products.
A perspective in the New England Journal of Medicine discusses how the pharmaceutical industry’s caution is bumping up against the US government’s efforts to accelerate development of COVID-19 vaccines. That represents something of a reversal of roles compared with normal times, when regulators have been accused of acting too slowly and demanding too much evidence before approving new products.
In a separate NEJM perspective, researchers involved in Operation Warp Speed, the effort of the US Department of Health and Human Services (HHS) and Department of Defense (DoD)—in partnership with the private sector—to accelerate the development of COVID-19 vaccines and treatments, say that “sound science is essential.”
September 15, 2020
 AstraZeneca has resumed its COVID-19 vaccine trial in the United Kingdom, but the study remains on hold in the United States as the investigation into the cause of a serious adverse event—believed to be a spinal inflammatory disorder called transverse myelitis—continues, Reuters reports. “Sources told Reuters that enrollment of new patients and other trial procedures for the pivotal US trial were being rescheduled until at least midweek and that it was not clear how long it would take for the FDA to complete its probe.” A story from Kaiser Health News indicates that officials from the US National Institutes of Health (NIH) are “very concerned.”
AstraZeneca has resumed its COVID-19 vaccine trial in the United Kingdom, but the study remains on hold in the United States as the investigation into the cause of a serious adverse event—believed to be a spinal inflammatory disorder called transverse myelitis—continues, Reuters reports. “Sources told Reuters that enrollment of new patients and other trial procedures for the pivotal US trial were being rescheduled until at least midweek and that it was not clear how long it would take for the FDA to complete its probe.” A story from Kaiser Health News indicates that officials from the US National Institutes of Health (NIH) are “very concerned.”
Another story from Kaiser Health News delves into the risk of becoming infected with SARS-CoV-2 on an airplane: “According to experts, the risk of catching the coronavirus on a plane is relatively low if the airline is following the procedures laid out by public health experts: enforcing mask compliance, spacing out available seats, and screening for sick passengers.”
 An international collective of cardiology societies released a practice update regarding telehealth and arrhythmia monitoring during and after a pandemic in EP Europace. “The crisis precipitated by the pandemic has catalyzed the adoption of remote patient management across many specialties and for heart rhythm professionals, in particular,” the authors write. “This practice is here to stay—it will persist even if other less arrhythmogenic treatment strategies evolve for COVID-19 and after the pandemic has passed.”
An international collective of cardiology societies released a practice update regarding telehealth and arrhythmia monitoring during and after a pandemic in EP Europace. “The crisis precipitated by the pandemic has catalyzed the adoption of remote patient management across many specialties and for heart rhythm professionals, in particular,” the authors write. “This practice is here to stay—it will persist even if other less arrhythmogenic treatment strategies evolve for COVID-19 and after the pandemic has passed.”
In a blog post, NIH Director Francis Collins, MD, PhD, discusses recent research showing that COVID-19 survivors often have persistent lung problems. “Moving forward, it will be important to conduct larger and longer-term studies of COVID-19 recovery in people of diverse backgrounds to continue to learn more about what it means to survive COVID-19,” he writes. “The new findings certainly indicate that for many people who’ve been hospitalized with COVID-19, regaining normal lung function may take a while.”
In the European Heart Journal: Case Reports, researchers detail three cases of pericardial effusion in patients with COVID-19; two of them were associated with myocarditis. The patients were treated with colchicine and their conditions improved rapidly.
 A study in Molecular Psychiatry shows that people with a recent diagnosis of substance use disorder are at increased risk for COVID-19. Relationships were strongest for disorders related to opioid and tobacco use. Among COVID-19 patients, those with substance use disorders had significantly heightened risks of death and hospitalization.
A study in Molecular Psychiatry shows that people with a recent diagnosis of substance use disorder are at increased risk for COVID-19. Relationships were strongest for disorders related to opioid and tobacco use. Among COVID-19 patients, those with substance use disorders had significantly heightened risks of death and hospitalization.
The interplay between COVID-19 and endocrine/metabolic diseases was a major topic at the recent 2020 European Congress of Endocrinology. “One thing that is clear from the beginning of the pandemic is that patients with underlying endocrine diseases, like diabetes, obesity, or the lack of vitamin D, were more at risk of developing severe COVID-19,” the president of the European Society of Endocrinology said in a press release. “Therefore, disciplines that work in the [field of] prevention, such as endocrinology, can focus on creating a healthier population, which can be important in the preparation for pandemics like COVID-19.”
September 14, 2020
 Dining out at indoor restaurants or bars may be an important risk factor for acquiring COVID-19, suggests new research in Morbidity and Mortality Weekly Report. Among 314 adults who developed COVID-19 symptoms and went for a test, nearly half tested positive and while similar proportions in both groups said they wore face coverings in public, had gone to hair salons, shops, or in-home gatherings, people who tested positive were almost twice as likely to have dined out at a restaurant in the 2 weeks preceding their illness.
Dining out at indoor restaurants or bars may be an important risk factor for acquiring COVID-19, suggests new research in Morbidity and Mortality Weekly Report. Among 314 adults who developed COVID-19 symptoms and went for a test, nearly half tested positive and while similar proportions in both groups said they wore face coverings in public, had gone to hair salons, shops, or in-home gatherings, people who tested positive were almost twice as likely to have dined out at a restaurant in the 2 weeks preceding their illness.
US confirmed cases have passed 6.45 million, according to the Johns Hopkins COVID-19 Tracker.
A small study published online in Circulation last week is calling into question the usefulness of cardiac biomarkers for COVID-19 prognosis beyond what’s obtained by clinical characteristics and national early warning scores (based on admission respiratory rate, oxygen saturation, supplemental oxygen, systolic blood pressure, pulse rate, temperature and level of consciousness). At least among consecutive patients enrolled in the COVID-19 Mechanisms Study in Norway, “findings do not support routine measurements of cardiovascular and inflammatory biomarkers on admission for prognostic purposes in patients hospitalized for COVID-19,” authors conclude.
 A blood donation analysis published today in JAMA found that just under 2% of blood donations in the first 2 weeks after antibody testing was introduced were found to contain SARS-CoV-2 antibodies. The number of first-time blood donors also increased during the COVID-19 period, likely due to the fact that “many blood collection organizations have implemented and publicized routine testing of donations for SARS-CoV-2 antibodies,” with donors being notified electronically if their blood was found to be reactive to assays, Roger Y. Dodd, PhD, and colleagues write.
A blood donation analysis published today in JAMA found that just under 2% of blood donations in the first 2 weeks after antibody testing was introduced were found to contain SARS-CoV-2 antibodies. The number of first-time blood donors also increased during the COVID-19 period, likely due to the fact that “many blood collection organizations have implemented and publicized routine testing of donations for SARS-CoV-2 antibodies,” with donors being notified electronically if their blood was found to be reactive to assays, Roger Y. Dodd, PhD, and colleagues write.
Stephen M. Hahn, MD, commissioner of the US Food and Drug Administration, and Peter Marks, MD, PhD, director of the US Center for Biologics Evaluation and Research, are reassuring the public that the process of reviewing and approving any COVID-19 vaccines will be rigorous but expeditious. “We are committed to expediting the development of COVID-19 vaccines, but not at the expense of sound science and decision making,” they write in the latest FDA Voices. “We will not jeopardize the public’s trust in our science-based, independent review of these or any vaccines.” A key milestone will be the October 22 meeting of the Vaccines and Related Biological Products Advisory Committee meeting. No vaccine candidate is currently slated for review, but the agency is “prepared to rapidly schedule” any additional meetings when an application is ready for review, they write.
 In Milan, Italy, “one of the cities with the highest SARS-CoV-2 burden in the world,” researchers found that just 1% of children presenting with no COVID-1 symptoms to hospital emergency rooms tested positive for SARS-CoV-2. By contrast, 9% of asymptomatic adults tested positive. “In this study, children without symptoms and signs of COVID-19 carried the virus less frequently than adults, suggesting that their role as facilitators of the spreading of SARS-CoV-2 infection could be reconsidered,” the authors write in a research letter in JAMA Pediatrics. In particular, they say, “these data do not support the hypothesis that children are at higher risk of carrying SARS-CoV-2 asymptomatically than adults.”
In Milan, Italy, “one of the cities with the highest SARS-CoV-2 burden in the world,” researchers found that just 1% of children presenting with no COVID-1 symptoms to hospital emergency rooms tested positive for SARS-CoV-2. By contrast, 9% of asymptomatic adults tested positive. “In this study, children without symptoms and signs of COVID-19 carried the virus less frequently than adults, suggesting that their role as facilitators of the spreading of SARS-CoV-2 infection could be reconsidered,” the authors write in a research letter in JAMA Pediatrics. In particular, they say, “these data do not support the hypothesis that children are at higher risk of carrying SARS-CoV-2 asymptomatically than adults.”
Also in JAMA Pediatrics, an expert viewpoint tackles the thorny question of whether SARS-CoV-2 vaccination, when it comes, should be mandatory for children attending schools. Authors propose four criteria for consideration but conclude—for the time being—"we currently know too little about the performance of any of the candidate COVID-19 vaccines or the epidemiology of SARS-CoV-2 in children to make any firm judgments about whether a COVID-19 vaccine should be mandatory in children.”
 Air quality from wildfires in California and the Pacific Northwest is now the worst in the world for Portland, OR, Seattle, WA, and Vancouver, Canada, such that people may be confused as to whether their respiratory symptoms are due to the toxic smoke or to COVID-19, says a senior environmental health scientist at the British Columbia Centre for Disease Control.
Air quality from wildfires in California and the Pacific Northwest is now the worst in the world for Portland, OR, Seattle, WA, and Vancouver, Canada, such that people may be confused as to whether their respiratory symptoms are due to the toxic smoke or to COVID-19, says a senior environmental health scientist at the British Columbia Centre for Disease Control.
Meanwhile, a modelling study published in Environmental Research Letters, suggests that every increase in the hazardous air pollutant exposure respiratory hazard index is associated with a 9% increase in COVID-19 mortality. “These findings help us to understand variation in US-based COVID-19 mortality rates, reinforce existing research linking air pollution to mortality, and emphasize the importance of regulatory efforts to limit air pollution exposure risk,” authors say.
Shelley Wood contributed today's COVID-19 Dispatch.
September 11, 2020
 Another study, this time in athletes who tested positive for COVID-19, has picked up evidence of myocarditis on cardiac MRI. The 26-subject series, published in JAMA Cardiology, is likely to spark fresh debate about when athletes can safely return to sport, as well as fueling questions about what lasting cardiac imprint the virus may leave even after asymptomatic or mild infections. My story is here on TCTMD.
Another study, this time in athletes who tested positive for COVID-19, has picked up evidence of myocarditis on cardiac MRI. The 26-subject series, published in JAMA Cardiology, is likely to spark fresh debate about when athletes can safely return to sport, as well as fueling questions about what lasting cardiac imprint the virus may leave even after asymptomatic or mild infections. My story is here on TCTMD.
France is considering a return to new lockdowns to curb the spread of COVID-19 after recording its highest ever single-day total of new infections: almost 10,000, Reuters reports. “Since the beginning of the month, new cases have gone up by 7,292 each day on average, a figure that blows away the previous record daily average of 3,003 seen in August.”
Just as children in many northern hemisphere countries are heading back to school, new research in Morbidity and Mortality Weekly Report confirms that while COVID-19 is less severe in children, transmissions from infected kids to adults “play a role,” authors say. By tracing the pattern of infections at three childcare facilities, authors determined that 12 children acquired COVID-19 there, with transmission from them to at least 12 of 46 nonfacility contacts (26%), including one parent who needed to be hospitalized. Asymptomatic children in two cases likely transmitted SARS-CoV-2 to their parents and possibly to their teachers. “Having SARS-CoV-2 testing available, timely results, and testing of contacts of patients in child care settings regardless of symptoms can help prevent transmission and provide a better understanding of the role played by children in transmission,” according to the investigators.
Indeed, school children and staff are one of the five high-risk groups singled out in an article in CMAJ that makes the case for “active testing strategies” for SARS-CoV-2 in people most at risk of infection. Also included are hospital employees, community health care workers and people in long-term care facilities, as well as essential business employees. Active testing, the authors argue, is affordable and would help support the safe reopening of schools and businesses more broadly.
Authors of a hydroxychloroquine/azithromycin paper published in the New England Journal of Medicine have today published corrections to their original article. “The report as published did not provide accurate and complete information on the frequency and duration of previous use of hydroxychloroquine or azithromycin among the trial participants,” they write. Their correction provides some specifics and rephrasing; the paper has been updated online.
 Analysis of 453 SARS-CoV-2 genomes collected from infected patients in Washington State between February 20 and March 15, 2020, suggests that “most SARS-CoV-2 infections sampled during this time derive from a single introduction in late January or early February 2020, which subsequently spread locally before active community surveillance was implemented,” investigators write in Science. Like others, they conclude that the virus was likely circulating undetected for several weeks before being picked up by health authorities.
Analysis of 453 SARS-CoV-2 genomes collected from infected patients in Washington State between February 20 and March 15, 2020, suggests that “most SARS-CoV-2 infections sampled during this time derive from a single introduction in late January or early February 2020, which subsequently spread locally before active community surveillance was implemented,” investigators write in Science. Like others, they conclude that the virus was likely circulating undetected for several weeks before being picked up by health authorities.
The US National Institutes of Health has launched two phase III trials evaluating the safety and effectiveness of various blood thinners to treat COVID-19, according to a press release issued yesterday. The trials make up two of the three studies within the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) initiative, to be conducted at more than 100 sites around the world. The aim is to enroll a range of patients: nonhospitalized, currently hospitalized, and discharged from hospital a moderate to severe disease course.
Results from a “vaccine confidence” study published in the Lancet using data from 290 nationally representative surveys suggests that sentiments are all over the map. While some countries, like France and the UK, have seen rising confidence in vaccines, Afghanistan, Azerbaijan, Indonesia, Nigeria, Pakistan, and Serbia have seen their already low confidence in vaccines erode still further, “mirroring trends in political instability and religious extremism,” a press release notes. “The public seem to generally understand the value of vaccines, but the scientific and public health community needs to do much better at building public trust in the safety of vaccination, particularly with the hope of a COVID-19 vaccine,” says co-lead author Clarissa Simas, MSc.
Continuous monitoring of SARS-CoV-2-specific antibody responses in 19 nonsevere and seven severe COVID-19 patients suggests that the neutralizing activity of antibodies from most recovered patients is relatively weak and declines sharply within a month of hospital discharge. Writing in PLOS Pathogens, Chao Wu, MD, PhD, and colleagues stress that their findings have implications for serological testing and vaccine development, and they hint that recovered COVID-19 patients may be susceptible to reinfection.
Using the last week of June as a snapshot of larger trends, an estimated 41% of American adults in a nationwide sample experienced delayed or avoided medical care due to COVID-19-related concerns, Mark É. Czeisler and colleagues write in Morbidity and Mortality Weekly Report. This included 12% who had delays or avoided urgent or emergency care (a particularly common phenomenon among unpaid caregivers for adults), persons with underlying medical conditions, Black adults, Hispanic adults, young adults, and people with disabilities. Delayed or avoided routine care was also relatively common, at 32%.
 Out-of-hospital cardiac arrests across 24 regional emergency medical services agencies, located in an area of Pennsylvania with low COVID-19 prevalence, were not higher than historic levels, according to a new letter to the editor in Resuscitation. Moreover, the proportion of cases deemed dead on arrival, as well as provision of layperson CPR, use of automated external defibrillators, and prehospital return of spontaneous circulation did not differ, although there were delays to use of epinephrine.
Out-of-hospital cardiac arrests across 24 regional emergency medical services agencies, located in an area of Pennsylvania with low COVID-19 prevalence, were not higher than historic levels, according to a new letter to the editor in Resuscitation. Moreover, the proportion of cases deemed dead on arrival, as well as provision of layperson CPR, use of automated external defibrillators, and prehospital return of spontaneous circulation did not differ, although there were delays to use of epinephrine.
Shelley Wood contributed today's COVID-19 Dispatch.
September 10, 2020
Newsrooms around the world led yesterday with the news that AstraZeneca had voluntarily paused its vaccine trial after a trial participant developed unexplained neurological symptoms. On a conference call with investors, CEO Pascal Soriot noted that the patient has not been formally diagnosed but her symptoms, “consistent with a rare but serious spinal inflammatory disorder called transverse myelitis,” are improving, STAT reported today. “Soriot also confirmed that the clinical trial was halted once previously in July after a participant experienced neurological symptoms. Upon further examination, that participant was diagnosed with multiple sclerosis, deemed to be unrelated to the Covid-19 vaccine treatment,“ he said.
 Not only did the number of STEMI patients decrease by 27% during the COVID-19 outbreak in Spain, but also ischemic times were longer and patients experienced a twofold increase in in-hospital mortality, nationwide registry data suggest. According to researchers writing in Revista Española de Cardiología, the official publication of the Spanish Society of Cardiology, these trends were seen despite the “infrequent” coexistence of both STEMI and confirmed SARS-CoV-2 infection (6.3%).
Not only did the number of STEMI patients decrease by 27% during the COVID-19 outbreak in Spain, but also ischemic times were longer and patients experienced a twofold increase in in-hospital mortality, nationwide registry data suggest. According to researchers writing in Revista Española de Cardiología, the official publication of the Spanish Society of Cardiology, these trends were seen despite the “infrequent” coexistence of both STEMI and confirmed SARS-CoV-2 infection (6.3%).
Given that hospital avoidance in the COVID-19 era is believed to be a key contributor to delays in seeking help for acute MI and stroke, a new analysis of nosocomial infections offers some reassurance. In a cohort study of more than 9,000 patients admitted to a large US academic hospital, only two cases of hospital-acquired COVID-19 could be identified. And one of these patients “was likely infected by a presymptomatic spouse before visitor restrictions were implemented,” its authors write in JAMA Network Open.
A survey-based study of social-distancing practices conducted by researchers at the Johns Hopkins Bloomberg School of Public Health has identified some key behaviors that appear to increase the risk of infection. “Using public transportation, visiting a place of worship, or otherwise traveling from the home is associated with a significantly higher likelihood of testing positive with the coronavirus SARS-CoV-2, while practicing strict social distancing is associated with a markedly lower likelihood,” reads a press release issued today. Fully survey results were published last week in Clinical Infectious Diseases.
 Offering a hint that COVID-19 may have been circulating earlier than expected, an analysis of electronic health records for patients presenting to UCLA hospitals and clinics shows a sharp rise in symptoms indicative of the disease as early as last December, researchers write in the Journal of Medical Internet Research. “This sudden spike in patients with these symptoms, which continued through February 2020, represents an unexpected 50% increase in such cases when compared with the same time period in each of the previous 5 years,” a press release states. “We may never truly know if these excess patients represented early and undetected COVID-19 cases in our area," lead author Joann Elmore, MD, MPH, is quoted in the release.
Offering a hint that COVID-19 may have been circulating earlier than expected, an analysis of electronic health records for patients presenting to UCLA hospitals and clinics shows a sharp rise in symptoms indicative of the disease as early as last December, researchers write in the Journal of Medical Internet Research. “This sudden spike in patients with these symptoms, which continued through February 2020, represents an unexpected 50% increase in such cases when compared with the same time period in each of the previous 5 years,” a press release states. “We may never truly know if these excess patients represented early and undetected COVID-19 cases in our area," lead author Joann Elmore, MD, MPH, is quoted in the release.
The prothrombotic state seen in patients infected with SARS-CoV-2 has been well-documented. Now researchers writing in the International Journal of Cardiology are warning that arterial thromboses “could be underestimated.” In their series—a retrospective review of patients at three hospitals in France and Italy in March and April 2020—arterial thrombotic events were seen in 209 patients, nearly one in 10 of those admitted to hospital. “At the time of the event, 10/20 (50%) of patients received thromboprophylaxis, 2/20 (10%) were receiving treatment dose anticoagulation, and 5/20 (25%) were receiving antiplatelet therapy,” they write. TCTMD has previously covered reports of this phenomenon in hospitalized patients and in patients who develop symptomatic arterial thrombosis in the legs.
An analysis of people with no preexisting comorbidities diagnosed with COVID-19 indicates that even healthy patients can suffer dire consequences, including mechanical ventilation or death. As described in Arteriosclerosis, Thrombosis, and Vascular Biology, investigators conducted a retrospective analysis of consecutive patients, excluding any with comorbidities. They report that while age remains the most important predictor of adverse hospital outcomes, “thromboinflammatory interactions are also associated with worse clinical outcomes regardless of age in healthy patients.”
 Correcting misconceptions about COVID-19 may mean addressing an individual’s underlying “moral values,” according to a paper in Educational Researcher. “Compounding the public health challenges posed by the COVID-19 pandemic is an infodemic of misinformation regarding risks, prevention, and treatments, which may lead to serious and irreversible harm to individuals and communities,” write Greg Trevors, PhD, and Melissa C. Duffy, PhD. Correcting misconceptions, however, is a minefield that must address how individual moral priorities conflict with recommendations from health authorities.
Correcting misconceptions about COVID-19 may mean addressing an individual’s underlying “moral values,” according to a paper in Educational Researcher. “Compounding the public health challenges posed by the COVID-19 pandemic is an infodemic of misinformation regarding risks, prevention, and treatments, which may lead to serious and irreversible harm to individuals and communities,” write Greg Trevors, PhD, and Melissa C. Duffy, PhD. Correcting misconceptions, however, is a minefield that must address how individual moral priorities conflict with recommendations from health authorities.
A viewpoint in JAMA Health Forum lays out critical policy considerations for people who are incarcerated with COVID-19 in US prisons. “Because Black American individuals and other people of color are overrepresented in correctional facility populations, COVID-19 outbreaks in this setting are likely to magnify existing structural racism and health inequities that have resulted in members of racial minority groups being disproportionately affected by the pandemic,” Emily Abdoler, MD, MAEd, and colleagues write.
Shelley Wood contributed today's COVID-19 Dispatch.
September 9, 2020
 AstraZeneca has paused late-stage trials of its COVID-19 vaccine candidate, developed in collaboration with the University of Oxford, after an unexplained illness developed in a participant, Reuters reports. The pause will allow an independent committee to review safety data. The vaccine is considered to be one of the leading candidates under evaluation right now, and AstraZeneca has already entered into agreements with various governments to provide around 3 billions doses if it is proven safe and effective.
AstraZeneca has paused late-stage trials of its COVID-19 vaccine candidate, developed in collaboration with the University of Oxford, after an unexplained illness developed in a participant, Reuters reports. The pause will allow an independent committee to review safety data. The vaccine is considered to be one of the leading candidates under evaluation right now, and AstraZeneca has already entered into agreements with various governments to provide around 3 billions doses if it is proven safe and effective.
Meanwhile, in a move to assuage concerns about rushing a vaccine to market without adequate testing, the leaders of nine biopharmaceutical companies—including AstraZeneca—signed a pledge “outlining a united commitment to uphold the integrity of the scientific process as they work towards potential global regulatory filings and approvals of the first COVID-19 vaccines.”
 Younger people with COVID-19 are less likely than those who are older to be hospitalized or need intensive care, but a new study published in JAMA Internal Medicine, which set the age cutoff at 35 years, suggests that the same risk factors that portend poor outcomes in older patients pertain to younger ones as well. “Although certainly the risk of severe outcomes is lower in younger people, those risks were still significant or meaningful, with 20% having to go to the ICU, 10% requiring a breathing tube, and 2.5% to 3% dying in the hospital,” the lead author told TCTMD’s L.A. McKeown.
Younger people with COVID-19 are less likely than those who are older to be hospitalized or need intensive care, but a new study published in JAMA Internal Medicine, which set the age cutoff at 35 years, suggests that the same risk factors that portend poor outcomes in older patients pertain to younger ones as well. “Although certainly the risk of severe outcomes is lower in younger people, those risks were still significant or meaningful, with 20% having to go to the ICU, 10% requiring a breathing tube, and 2.5% to 3% dying in the hospital,” the lead author told TCTMD’s L.A. McKeown.
In response to rising COVID-19 case numbers, social gatherings both indoors and outdoors will be capped at just six people in England starting Monday, September 14, BBC reports. Exceptions will include schools, workplaces, and weddings, funerals, and team sports adhering to COVID-19 protective measures.
A news story in the BMJ, citing leaked documents, reveals that the UK government plans invest about £100bn ($130 billion) to expand its COVID-19 testing to up to 10 million per day by early next year.
The American Medical Association (AMA) announced two new Current Procedural Terminology (CPT) codes for reporting medical services related to the COVID-19 response. Code 99072 deals with the additional supplies and staff needed to perform safety protocols during a public health emergency, and code 86413 addresses the reporting of quantitative antibody detection of SARS-CoV-2.
Patients who were already taking oral anticoagulation before being hospitalized for COVID-19 were not more likely to survive to hospital discharge than those who were not on oral anticoagulation, according to a study in the International Journal of Cardiology. Use of heparin in the hospital, though, was associated with lower odds of dying, particularly in patients with acute hypoxemic respiratory failure.
 A perspective in the New England Journal of Medicine explores the idea that wearing a mask might serve to inoculate the population against SARS-CoV-2 infection by exposing people to small amounts of the virus. “If this hypothesis is borne out, universal masking could become a form of ‘variolation’ that would generate immunity and thereby slow the spread of the virus in the United States and elsewhere, as we await a vaccine,” the authors propose.
A perspective in the New England Journal of Medicine explores the idea that wearing a mask might serve to inoculate the population against SARS-CoV-2 infection by exposing people to small amounts of the virus. “If this hypothesis is borne out, universal masking could become a form of ‘variolation’ that would generate immunity and thereby slow the spread of the virus in the United States and elsewhere, as we await a vaccine,” the authors propose.
The motorcycle rally drawing more than 460,000 people to Sturgis, SD, in early August has been labeled a “superspreader” event in a new paper published by IZA – Institute of Labor Economics, a German think tank. Yahoo News provides some details, including the estimated public health costs stemming from the event—$12.2 billion.
Third-party tracking is pervasive among COVID-19-related websites, even those from the government or academia, according to a study in JAMA. “Amid debate and legislative activity focused on the privacy implications of COVID-19 contact-tracing apps, these findings suggest that attention should also be paid to privacy risks of online information seeking,” the authors conclude.
September 8, 2020
 A deep dive into cardiovascular risks among patients hospitalized with COVID-19, presented during the virtual European Society of Cardiology (ESC) Congress 2020, indicates that disentangling COVID-19 from preexisting CV risk factors when cardiac events occur is tricky. “It’s really easy to make the mistake of solely focusing on the virus and attributing all symptoms and signs that these patients may develop to a severe COVID-19 course,” Manan Pareek, MD, PhD, told TCTMD Managing Editor Shelley Wood. “These very high cardiovascular complication rates suggest that we have to be more vigilant in detecting and possibly treating these complications and that’s actually not easy in this population.”
A deep dive into cardiovascular risks among patients hospitalized with COVID-19, presented during the virtual European Society of Cardiology (ESC) Congress 2020, indicates that disentangling COVID-19 from preexisting CV risk factors when cardiac events occur is tricky. “It’s really easy to make the mistake of solely focusing on the virus and attributing all symptoms and signs that these patients may develop to a severe COVID-19 course,” Manan Pareek, MD, PhD, told TCTMD Managing Editor Shelley Wood. “These very high cardiovascular complication rates suggest that we have to be more vigilant in detecting and possibly treating these complications and that’s actually not easy in this population.”
A feature story in Nature delves into how much it matters that SARS-CoV-2 is mutating as it continues to spread around the world. “Researchers still have more questions than answers about coronavirus mutations, and no one has yet found any change in SARS-CoV-2 that should raise public-health concerns,” according to the story. “But studying mutations in detail could be important for controlling the pandemic. It might also help to preempt the most worrying of mutations: those that could help the virus to evade immune systems, vaccines, or antibody therapies.”
 In a blog post, US National Institutes of Health (NIH) Director Francis Collins, MD, PhD, discusses how genome data were used to help track the impact of a superspreading event—a Boston, MA, biotech conference held in February. The analysis showed that “more than one-third of Boston-area cases without any known link to the conference could indeed be traced back to the event,” Collins writes. That works out to nearly 20,000 COVID-19 cases in the Boston area.
In a blog post, US National Institutes of Health (NIH) Director Francis Collins, MD, PhD, discusses how genome data were used to help track the impact of a superspreading event—a Boston, MA, biotech conference held in February. The analysis showed that “more than one-third of Boston-area cases without any known link to the conference could indeed be traced back to the event,” Collins writes. That works out to nearly 20,000 COVID-19 cases in the Boston area.
Since COVID-19 blazed its way across the globe, there has been “unprecedented scientific production” from the research community, with thousands of papers published in the first 4 months of 2020 alone, but their overall quality has been less impressive, according to an analysis presented recently during ESC 2020. “The lines of evidence that have become available need to be interpreted with caution because we all know that studies published in major medical journals, particularly during an emergency such as COVID-19, are translated into clinical practice within a couple of days,” Giulio Stefanini, MD, PhD, said.
Among children, rates of hospitalization, ICU admission, and mechanical ventilator use did not differ between those with seasonal influenza and those with COVID-19, researchers report in JAMA Network Open. Pediatric patients hospitalized with COVID-19 were more likely to have symptoms like fever, diarrhea or vomiting, headache, body ache or myalgia, and chest pain.
Also in JAMA Network Open, an analysis of mobile phone data shows that Americans traveled less and stayed at home more after implementation of stay-at-home orders, with some geographic variation. The lockdown orders were associated with slowed spread of SARS-CoV-2.
A modeling study in PNAS suggests that more-focused, local lockdowns are as effective as a far-reaching global lockdown at controlling the spread of SARS-CoV-2, at least in the Canadian province of Ontario. The analysis “shows that the county-by-county approach causes fewer days of closure and impacts fewer people than a strategy that opens or closes the entire province together,” the authors write. “This is true even if individuals begin traveling to reopened counties with higher frequency.”
 Consistent with prior studies, data out of China presented during ESC 2020 affirm that COVID-19 is associated with a greater risk of thromboembolic events and that anticoagulation seems to protect against these adverse outcomes. TCTMD’s Caitlin Cox reports on the findings.
Consistent with prior studies, data out of China presented during ESC 2020 affirm that COVID-19 is associated with a greater risk of thromboembolic events and that anticoagulation seems to protect against these adverse outcomes. TCTMD’s Caitlin Cox reports on the findings.
COVID-19 can lead to long-term lung and heart damage that can, however, improve over time, according to a study presented during the European Respiratory Society International Congress. At 6 weeks after discharge from the initial hospitalization, 88% of patients had lung damage on CT. That proportion dropped to 56% by 12 weeks. Also at the 6-week visit, 58.5% of patients had LV dysfunction on echocardiography.
September 4, 2020
 Results from phase I/II studies of the COVID-19 vaccine licensed last month by Russia—dubbed Sputnik V—have been published in the Lancet. Among 76 healthy adult volunteers, the most common adverse events were pain at the injection site (58%), hyperthermia (50%), headache (42%), asthenia (28%), and muscle and joint pain (24%). There were no serious adverse events. All participants produced antibodies to SARS-CoV-2 glycoprotein. The studies are “encouraging but small,” according to authors of an accompanying editorial, which delves into the strengths and weaknesses of the studies.
Results from phase I/II studies of the COVID-19 vaccine licensed last month by Russia—dubbed Sputnik V—have been published in the Lancet. Among 76 healthy adult volunteers, the most common adverse events were pain at the injection site (58%), hyperthermia (50%), headache (42%), asthenia (28%), and muscle and joint pain (24%). There were no serious adverse events. All participants produced antibodies to SARS-CoV-2 glycoprotein. The studies are “encouraging but small,” according to authors of an accompanying editorial, which delves into the strengths and weaknesses of the studies.
Ahead of the long Labor Day weekend in the United States, Anthony Fauci, MD, director of the US National Institute of Allergy and Infectious Diseases (NIAID), warned that there are several states at risk for a surge in COVID-19 cases—specifically, North Dakota, South Dakota, Iowa, Arkansas, Missouri, Indiana, and Illinois—during an interview on the “Today” show, HuffPost reports. “If we’re careless about it, then we could wind up with a surge following Labor Day,” Fauci said.
In a perspective in PNAS, researchers explore possible reasons for milder COVID-19 in children, including reduced ACE2 in the respiratory tract; cross-protection from exposure to common colds caused by other coronaviruses; potential protection from T helper 2 immune responses and eosinophilia; reduced levels of inflammatory cytokines; and social factors. “Understanding the basis for why children have generally done better than adults provides important insights into the pathogenesis of COVID-19, which may guide our understanding of susceptibility to infection and may provide further clues for therapeutics,” the authors write.
 Penn State University’s director of athletic medicine, Wayne Sebastianelli, MD, caused a stir earlier this week when he said that roughly one-third of athletes in the Big Ten conference who had tested positive for COVID-19 may have had myocarditis. But the university has since clarified that the figure was shared with Sebastianelli verbally and that when the research was submitted for publication, the rate was 15%, according to a story in the Centre Daily Times.
Penn State University’s director of athletic medicine, Wayne Sebastianelli, MD, caused a stir earlier this week when he said that roughly one-third of athletes in the Big Ten conference who had tested positive for COVID-19 may have had myocarditis. But the university has since clarified that the figure was shared with Sebastianelli verbally and that when the research was submitted for publication, the rate was 15%, according to a story in the Centre Daily Times.
Mandatory stay-at-home orders successfully reduced population movement in the United States, according to a study based on mobile-device data published in Morbidity and Mortality Weekly Report. Movement increased as the orders were relaxed. “Further studies are needed to assess the timing and conditions under which stay-at-home orders might be best used to protect health, minimize negative impacts, and ensure equitable enforcement of community mitigation policies,” the authors write.
In a blog post, US National Institutes of Health (NIH) Director Francis Collins, MD, PhD, details how “citizen scientists” are tackling the problem of “long-haul COVID-19” that results in health problems for weeks or months after recovering from even mild cases.
 Another study in MMWR details how hydroxychloroquine and chloroquine prescribing patterns varied in the first half of the year as the understanding of the risks and benefits of the drugs evolved. Prescriptions in March represented a 7.2-fold year-over-year increase, and those in April represented a 3.3-fold increase. Nonroutine prescribers accounted for largest spikes in new prescriptions. “Although dispensing of hydroxychloroquine or chloroquine prescriptions has been declining since March 2020, continued attention to updated clinical guidance, especially by nonroutine prescribers, will help safeguard supplies and ensure safe use of these medications for patients with approved indications,” according to the researchers.
Another study in MMWR details how hydroxychloroquine and chloroquine prescribing patterns varied in the first half of the year as the understanding of the risks and benefits of the drugs evolved. Prescriptions in March represented a 7.2-fold year-over-year increase, and those in April represented a 3.3-fold increase. Nonroutine prescribers accounted for largest spikes in new prescriptions. “Although dispensing of hydroxychloroquine or chloroquine prescriptions has been declining since March 2020, continued attention to updated clinical guidance, especially by nonroutine prescribers, will help safeguard supplies and ensure safe use of these medications for patients with approved indications,” according to the researchers.
Patients with COVID-19 and acute respiratory distress syndrome (ARDS) have circulating cytokine levels that are lower compared with those in patients with bacterial sepsis and similar compared with those in other critically ill patients, researchers report in JAMA. “The findings of this preliminary analysis suggest COVID-19 may not be characterized by cytokine storm,” they say.
 Canada’s Chief Public Health Officer Theresa Tam, BMBS, offered some tips around sexual activity in the time of COVID-19, including advice to consider wearing a mask during the act. Limiting use of alcohol and other substances that might cloud your judgement, as well as skipping kissing are also recommended. “Remember as with all social interactions, try to keep your number of close contacts low if possible,” she wrote in a statement. “The lowest risk sexual activity during COVID-19 involves yourself alone.”
Canada’s Chief Public Health Officer Theresa Tam, BMBS, offered some tips around sexual activity in the time of COVID-19, including advice to consider wearing a mask during the act. Limiting use of alcohol and other substances that might cloud your judgement, as well as skipping kissing are also recommended. “Remember as with all social interactions, try to keep your number of close contacts low if possible,” she wrote in a statement. “The lowest risk sexual activity during COVID-19 involves yourself alone.”
September 3, 2020
In a phase I-II placebo-controlled study in healthy adults, a recombinant SARS-CoV-2 vaccine developed by Novavax “elicited immune responses that exceeded levels in COVID-19 convalescent serum” and appeared safe. The findings were reported in the New England Journal of Medicine.
 A study out of Italy, published in BMJ Open, suggests that COVID-19 patients should be retested much later than currently recommended to minimize the risk of SARS-CoV-2 transmission. The median time to viral clearance was 30 days from diagnosis and 36 days from symptom onset. “Our data indicate that testing at 14 days from diagnosis, as many regional surveillance protocols recommend, will result in most cases still being positive,” the authors say. “So that at least half of these tests are negative, testing should be done after more than 4 weeks once patients are symptom-free.”
A study out of Italy, published in BMJ Open, suggests that COVID-19 patients should be retested much later than currently recommended to minimize the risk of SARS-CoV-2 transmission. The median time to viral clearance was 30 days from diagnosis and 36 days from symptom onset. “Our data indicate that testing at 14 days from diagnosis, as many regional surveillance protocols recommend, will result in most cases still being positive,” the authors say. “So that at least half of these tests are negative, testing should be done after more than 4 weeks once patients are symptom-free.”
In a commentary in Circulation, Charles Lowenstein, MD, and Scott Solomon, MD, “propose that severe COVID-19 is a microvascular disease in which coronavirus infection activates endothelial cells, triggering exocytosis, a rapid vascular response that drives microvascular inflammation and thrombosis.”
To increase the chances of having an in-person meeting, the American College of Cardiology has pushed back its planned 2021 Scientific Session in Atlanta, GA—originally slated for the end of March—to May 15 to 17. That pushes it right up against EuroPCR 2021 (scheduled for May 18 to 21).
Acute heart failure was diagnosed in 2.5% of patients with confirmed COVID-19, and the majority of those patients (77.9%) did not have a history of heart failure, according to a study in the European Journal of Heart Failure. Acute heart failure was associated with a much higher mortality risk (46.8% vs 19.7%).
 The US Centers for Disease Control and Prevention (CDC) has told states to get ready to distribute COVID-19 vaccine to high-risk groups as early as late October, Reuters reports based on documents published by the agency. “For the purpose of initial planning, CDC provided states with certain planning assumptions as they work on state specific plans for vaccine distribution, including possibly having limited quantities of vaccines in October and November,” a CDC spokeswoman told Reuters. Health officials are worried about the expedited timeline, according to a story in the Los Angeles Times.
The US Centers for Disease Control and Prevention (CDC) has told states to get ready to distribute COVID-19 vaccine to high-risk groups as early as late October, Reuters reports based on documents published by the agency. “For the purpose of initial planning, CDC provided states with certain planning assumptions as they work on state specific plans for vaccine distribution, including possibly having limited quantities of vaccines in October and November,” a CDC spokeswoman told Reuters. Health officials are worried about the expedited timeline, according to a story in the Los Angeles Times.
The US Food and Drug Administration (FDA) has updated its guidance on use of convalescent plasma in COVID-19, providing additional information related to its recently issued emergency use authorization.
A study in the Journal of the American College of Cardiology explores echocardiographic findings in the multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19. “Unlike classic Kawasaki disease, coronary arteries may be spared in early MIS-C; however, myocardial injury is common,” the authors report.
 COVID-19 death risk varies by age, race, ethnicity, and sex, according to a study in the Annals of Internal Medicine. Based on data from Indiana, the highest “infection fatality ratios” were seen in people ages 60 and older and in non-whites.
COVID-19 death risk varies by age, race, ethnicity, and sex, according to a study in the Annals of Internal Medicine. Based on data from Indiana, the highest “infection fatality ratios” were seen in people ages 60 and older and in non-whites.
September 2, 2020
 Results of three randomized, controlled trials of corticosteroids—CAPE COVID from France and the international REMAP-CAP, which both evaluated hydrocortisone, as well as CoDEX from Brazil, which evaluated dexamethasone—were published today in JAMA. All three trials were stopped early after the release of the positive RECOVERY trial results with dexamethasone, leaving the analyses underpowered to show a clear win or loss for corticosteroids for a range of endpoints. All three studies, however, along with four more, were included in a meta-analysis also published in JAMA today. Here, “28-day mortality was lower in patients randomized to corticosteroids: 222 deaths among 678 patients randomized to corticosteroids compared with 425 deaths among 1,025 patients randomized to usual care or placebo,” authors with the World Health Organization’s REACT working group conclude. An editorial aims to put all of these data in perspective.
Results of three randomized, controlled trials of corticosteroids—CAPE COVID from France and the international REMAP-CAP, which both evaluated hydrocortisone, as well as CoDEX from Brazil, which evaluated dexamethasone—were published today in JAMA. All three trials were stopped early after the release of the positive RECOVERY trial results with dexamethasone, leaving the analyses underpowered to show a clear win or loss for corticosteroids for a range of endpoints. All three studies, however, along with four more, were included in a meta-analysis also published in JAMA today. Here, “28-day mortality was lower in patients randomized to corticosteroids: 222 deaths among 678 patients randomized to corticosteroids compared with 425 deaths among 1,025 patients randomized to usual care or placebo,” authors with the World Health Organization’s REACT working group conclude. An editorial aims to put all of these data in perspective.
A committee of experts established by the National Academies of Sciences, Engineering, and Medicine, at the behest of Francis Collins, MD, PhD, director of the US National Institutes of Health (NIH), and Robert Redfield, MD, director of the Centers for Disease Control and Prevention (CDC), is trying to lay the groundwork for which populations should have priority access to a COVID-19 vaccine, STAT reports. In the story, Bill Foege, MD, a former director of the CDC who is co-chair of the committee, said he expects pushback on some of the report’s recommendations during a virtual public meeting that is taking place all afternoon today.
Serum samples from over 30,500 Icelanders suggests that the best way to measure seropositivity to SARS-CoV-2 antibodies is to use two pan-immunoglobulin (pan-Ig) assays, researchers report in the New England Journal of Medicine. Using this approach to test samples from 1,237 COVID-19 survivors up to 4 months after their diagnoses, investigators concluded that antiviral antibodies do not decline within 4 months, that risk of dying is just 0.3%, and that 44% of infected people were never diagnosed by quantitative PCR.
 A study of bus riders in eastern China has implications for commuters everywhere as workplaces reopen. Among 128 individuals travelling in two different buses, those who travelled in a bus with air recirculation had increased risk of infection compared with travelers on the other bus, that didn’t have recirculated air. Find the full paper in JAMA Internal Medicine.
A study of bus riders in eastern China has implications for commuters everywhere as workplaces reopen. Among 128 individuals travelling in two different buses, those who travelled in a bus with air recirculation had increased risk of infection compared with travelers on the other bus, that didn’t have recirculated air. Find the full paper in JAMA Internal Medicine.
Clearing the backlog of surgical cases postponed at the height of the pandemic in the Canadian province of Ontario will take 84 weeks, physicians writing in CMAJ estimate. For the most time-sensitive surgeries—cardiac, vascular, and cancer surgeries—authors hope 14 weeks will be enough, but that’s at the expense of other surgeries, including pediatric cases. “The magnitude of the surgical backlog from COVID-19 raises important implications for planning for the recovery phase and for possible second waves of the pandemic,” senior author Jonathan Irish, MD, warned in a press release.
Catherine Ettman, BA, and colleagues, writing in JAMA Network Open, conducted a survey of US adults, finding that depression burden has been more than threefold higher during the pandemic compared with previous time periods. Lower household income, lower savings, and exposure to more stressors increased the risk of depression symptoms during COVID-19.
Halfway around the globe, falling household incomes, rising food insecurity, and higher depression and anxiety were also the hallmark effects of stay-at-home orders in Bangladesh, according to a study based on interviews with mothers that was published in the Lancet Global Health. Among those who experienced emotional or physical domestic violence prior to the pandemic, over half said it increased during lockdown.
 Sheltering in place is also likely having a negative impact on patients with chronic coronary syndromes, French researchers report in the International Journal of Cardiology. From their cross-sectional population-based study, investigators gleaned that “mainly driven by media influence or family members,” adherence to medical therapy remained high. On the other hand, lifestyle habits declined. More than one-quarter reduced their amount of physical activity, one-quarter increased the amount they smoked, and roughly the same proportion said they’d gained at least 2 kg.
Sheltering in place is also likely having a negative impact on patients with chronic coronary syndromes, French researchers report in the International Journal of Cardiology. From their cross-sectional population-based study, investigators gleaned that “mainly driven by media influence or family members,” adherence to medical therapy remained high. On the other hand, lifestyle habits declined. More than one-quarter reduced their amount of physical activity, one-quarter increased the amount they smoked, and roughly the same proportion said they’d gained at least 2 kg.
Just when you thought COVID-19 news couldn’t get any more foul, a research team in Hong Kong is concluding that fecal aerosols, caused by flushing toilets, are the likely source of virus transmission in a high-rise building in Guangzhou, China. The analysis, published in the Annals of Internal Medicine, was based on throat swabs from infected patients, other building residents, and building staff; surface and air samples from flats, public areas, and drainage systems; and tracer gas released into bathrooms.
Shelley Wood contributed today's COVID-19 Dispatch.
September 1, 2020
 The only Hot Line trial dealing with COVID-19 was released at the virtual European Society of Cardiology (ESC) Congress 2020 earlier today. BRACE CORONA, presented by Renato D. Lopes, MD, tackled the controversy over ACE inhibitors and ARBs in patients with SARS-CoV-2 infection. Investigators concluded: “There is no clinical benefit from routinely suspending these medications in hospitalized patients with mild to moderate COVID-19 [and] they should be generally continued for those with an indication.” TCTMD’s Michael O’Riordan has the full story.
The only Hot Line trial dealing with COVID-19 was released at the virtual European Society of Cardiology (ESC) Congress 2020 earlier today. BRACE CORONA, presented by Renato D. Lopes, MD, tackled the controversy over ACE inhibitors and ARBs in patients with SARS-CoV-2 infection. Investigators concluded: “There is no clinical benefit from routinely suspending these medications in hospitalized patients with mild to moderate COVID-19 [and] they should be generally continued for those with an indication.” TCTMD’s Michael O’Riordan has the full story.
Also at ESC 2020, a special late-breaking session dedicated to COVID-19 and the heart is now available for replay with free registration. Presentations include an analysis of COVID-19 in women, an update from the cardiac complications registry, thromboembolism risks, and an analysis of “scientific pressure” on COVID-19 manuscript quality.
On the same theme, a letter to the editor in Mayo Clinic Proceedings reports that review times for COVID-19-related studies by medical journals are radically shorter than for non-COVID-19 studies (11.3 days as opposed to 106.3 days, P <0.00). Moreover, thousands of research papers published to preprint servers have never undergone peer review and the sheer volume makes it difficult for journals to identify whether the same cases and patients are being reported across different papers. “Our data highlight important threats to the validity of the evolving COVID-19 literature, which may be particularly acute in the current climate. While our response to this crisis should be swift, it must also be scientifically rigorous,” Michael S. Putman, MD, and colleagues conclude.
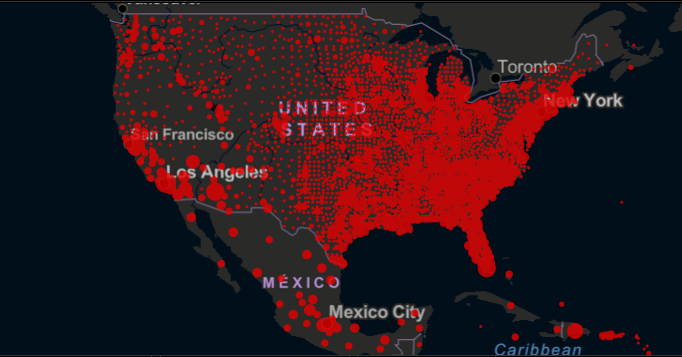
A viewpoint in JAMA ponders lessons from the hydroxychloroquine debacle and what can be learned for future emergency use authorizations (EUAs) of unapproved medications during pandemics. In the case of hydroxychloroquine, as reported by TCTMD, the US Food and Drug Administration issued a rapid EUA that was revoked within weeks. The experience has implications for the rapid development of vaccines, caution Kyle Thomson, JD, MPH, and Herschel Nachlis, PhD—a point also argued in a separate JAMA Viewpoint by Jerry Avorn, MD, and Aaron Kesselheim, MD, JD, MPH.
In a hint of good news, investigators writing in PNAS say that their genetic analysis of more than 18,000 SARS-CoV-2 sequences suggests that “neutral evolution,” as opposed to adaptive selection, can explain the rare mutations seen across SARS-CoV-2 genomes. That finding implies that “to date, the limited diversity seen in SARS-CoV-2 should not preclude a single vaccine from providing global protection.”
A multicenter study out of Denmark gets credit for having one of the canniest trial names to date. In ECHOVID-19, investigators used echocardiography with 2-D speckle tracking in all laboratory-confirmed cases of COVID-19 and concluded that myocardial impairment is “common” among hospitalized COVID-19 patients and predicts a higher risk of acute respiratory distress syndrome. However, “we do not propose that impaired systolic function due to COVID-19 infection is a causal agent of ARDS development,” the investigators conclude in JACC: Cardiovascular Imaging.
 A seroprevalence study of 3,248 healthcare personnel from around the United States found that 6% had antibody evidence of prior SARS-CoV-2 infection, but almost one-third had been asymptomatic and 69% had never had a diagnosis of infection. According to the paper in Morbidity and Mortality Weekly Report, “Prevalence of SARS-CoV-2 antibodies was lower among personnel who reported always wearing a face covering while caring for patients (6%), compared with those who did not (9%).”
A seroprevalence study of 3,248 healthcare personnel from around the United States found that 6% had antibody evidence of prior SARS-CoV-2 infection, but almost one-third had been asymptomatic and 69% had never had a diagnosis of infection. According to the paper in Morbidity and Mortality Weekly Report, “Prevalence of SARS-CoV-2 antibodies was lower among personnel who reported always wearing a face covering while caring for patients (6%), compared with those who did not (9%).”
The American Heart Association is once again inviting researchers to submit proposals for analyses of its COVID-19 registry, which includes patient clinical characteristics, medications, treatments, labs, vitals, biomarkers, and outcomes for more than 15,000 adult patients hospitalized with COVID-19 at more than 150 US sites. The deadline for proposals is September 15, 2020.
Shelley Wood contributed today's COVID-19 Dispatch.
COVID-19: TCTMD'S Daily Dispatch for October
COVID-19: TCTMD's Daily Dispatch for August
COVID-19: TCTMD’s Daily Dispatch for July
COVID-19: TCTMD’s Daily Dispatch for June
COVID-19: TCTMD’s Daily Dispatch for May
COVID-19: TCTMD’s Daily Dispatch for April
COVID-19: TCTMD’s Daily Dispatch for March
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full Bio

Comments