COVID-19: TCTMD’s Daily Dispatch for May
We’re curating a list of COVID-19 research and other useful content, and updating it daily.

TCTMD reporter Todd Neale is keeping up on breaking news and peer-reviewed research related to COVID-19 and will update daily. If you have something to share, tell us.
May 29, 2020
A national survey by the Society for Cardiovascular Angiography and Interventions (SCAI) confirms that many Americans are not going to the hospital for serious medical emergencies like MI and stroke because they’re afraid of getting COVID-19, a phenomenon believed to be a major driver of the fall in presentations for these events during the pandemic. Half of respondents said they were more afraid of contracting COVID-19 than of having an MI or stroke. “The data that we are seeing from this survey is not just disturbing, it is a clear sign that Americans may be in for a dangerous third wave of complications, and even fatalities, from delaying cardiac care during the time of this pandemic,” said SCAI President Cindy Grines, MD.
 Distilling several recent studies, a story in the New York Times indicates that the world is far from reaching the herd immunity needed to keep spread of SARS-CoV-2 in check: “Official case counts often substantially underestimate the number of coronavirus infections. But in new studies that test the population more broadly, the percentage of people who have been infected so far is still in the single digits . . . The precise herd immunity threshold for the novel coronavirus is not yet clear; but several experts said they believed it would be higher than 60%.”
Distilling several recent studies, a story in the New York Times indicates that the world is far from reaching the herd immunity needed to keep spread of SARS-CoV-2 in check: “Official case counts often substantially underestimate the number of coronavirus infections. But in new studies that test the population more broadly, the percentage of people who have been infected so far is still in the single digits . . . The precise herd immunity threshold for the novel coronavirus is not yet clear; but several experts said they believed it would be higher than 60%.”
Some hospitalized patients who recover from COVID-19 will test positive for the infection again after discharge, according to a study of 69 patients released from a hospital in Guizhou Province, China. Eleven patients (15.9%) had positive RT-PCR results after discharge but no symptoms, “which suggests that some recovered patients may still be virus carriers even after they reach the basic discharge criteria,” the researchers report in JAMA Network Open.
As negative data accumulate, the European Medicines Agency (EMA) is reminding healthcare professionals about the need to closely monitor COVID-19 patients who are being treated with hydroxychloroquine and chloroquine, which have established side effects but no proven benefits in this setting. “When prescribing these medicines, healthcare professionals should take into account preexisting heart conditions, uncorrected potassium or magnesium imbalance, and concomitant use with medicines that prolong the QT interval as these factors may make patients more prone to heart rhythm disorders,” the agency said.
But questions are being raised about at least one of the recent negative hydroxychloroquine studies, which prompted the World Health Organization to stop enrolling patients into the hydroxychloroquine arm of a major trial. More than 100 researchers have written an open letter to Mandeep Mehra, MD, and colleagues, who authored the study in question, as well as Richard Horton, MBChB, editor-in-chief of the Lancet, to request additional details about the data used for the study, independent validation of the results, open access to data sharing agreements, and access to peer review comments.
 A research letter in JAMA, by Muthiah Vaduganathan, MD, and colleagues found that US prescriptions for hydroxychloroquine and chloroquine soared by nearly 2000% during one week in March, whereas prescriptions for ACE inhibitors and ARBs remained relatively stable, TCTMD's Shelley Wood reports.
A research letter in JAMA, by Muthiah Vaduganathan, MD, and colleagues found that US prescriptions for hydroxychloroquine and chloroquine soared by nearly 2000% during one week in March, whereas prescriptions for ACE inhibitors and ARBs remained relatively stable, TCTMD's Shelley Wood reports.
Consistent with data from China, researchers report in JAMA Network Open that mental health issues are common during the pandemic among healthcare workers in Italy, particularly among young women and those on the front lines. Post-traumatic stress symptoms were reported in about half, symptoms of depression in 24.7%, symptoms of anxiety in 19.8%, insomnia in 8.3%, and high perceived stress in 21.9%.
Acute kidney injury (AKI) may be more common among patients with COVID-19 than initially thought, according to a study in the BMJ. Among 1,000 patients treated at NewYork-Presbyterian/Columbia University Irving Medical Center, AKI was seen in 33.9%. That rate reached 78% in the patients admitted to the ICUs. “These findings might help inform frontline providers and provide anticipatory guidance for the international community during this pandemic,” the authors say.
 The US Food and Drug Administration (FDA) has issued an emergency use authorization (EUA) for Stryker Sustainability Solutions VHP N95 Respirator Decontamination System, which uses vapor hydrogen peroxide for cleaning.
The US Food and Drug Administration (FDA) has issued an emergency use authorization (EUA) for Stryker Sustainability Solutions VHP N95 Respirator Decontamination System, which uses vapor hydrogen peroxide for cleaning.
Based on studies out of Spain and China, Diana Aguiar de Sousa, MD, and colleagues tackle the “curious case of the missing strokes during the COVID-19 pandemic” in an editorial in Stroke. “Taken together, observations from these two studies show the ability to provide guideline-concordant stroke care in a pandemic with appropriate support from hospital administration and protected stroke pathways,” they write. “While this is reassuring, it is concerning that during the COVID-19 pandemic some missing stroke patients who would otherwise have been treated could have died or become disabled due to a failure to seek medical attention, as discussed in these reports.”
Two viewpoints in JAMA address different aspects of research during the COVID-19 pandemic. One, by Paul Starr, PhD, details how controlled trials can help untangle the impacts of different public health policies around lockdowns and reopening strategies. The other, by Thomas Fleming, PhD, and colleagues, discusses how to protect the scientific integrity of clinical research.
 The prevalence of COVID-19 on affected cruise ships “is likely to be significantly underestimated, and strategies are needed to assess and monitor all passengers to prevent community transmission after disembarkation,” researchers conclude in a brief communication in Thorax. Of all 217 passengers and crew on an isolated cruise ship, 59% tested positive for SARS-CoV-2 and most of those people (81%) were asymptomatic.
The prevalence of COVID-19 on affected cruise ships “is likely to be significantly underestimated, and strategies are needed to assess and monitor all passengers to prevent community transmission after disembarkation,” researchers conclude in a brief communication in Thorax. Of all 217 passengers and crew on an isolated cruise ship, 59% tested positive for SARS-CoV-2 and most of those people (81%) were asymptomatic.
A cohort study from Beijing, China, published in BMJ Global Health, indicates that wearing face masks in the home, before the initially infected person develops symptoms, can help cut SARS-CoV-2 transmission among family members. Mask use after the onset of symptoms was not shown to be effective.
There are new autopsy data out of New Orleans, LA, on 10 African-Americans who died from COVID-19. “Important findings include the presence of thrombosis and microangiopathy in the small vessels and capillaries of the lungs, with associated hemorrhage, that significantly contributed to death,” the researchers report in the Lancet Respiratory Medicine. “Cardiac findings included individual cell necrosis without lymphocytic myocarditis.”
May 28, 2020
 The number of COVID-19 deaths in the United States has topped 100,000, according to the Johns Hopkins Coronavirus Resource Center. Worldwide, COVID-19 has killed more than 350,000 out of about 5.7 million confirmed cases.
The number of COVID-19 deaths in the United States has topped 100,000, according to the Johns Hopkins Coronavirus Resource Center. Worldwide, COVID-19 has killed more than 350,000 out of about 5.7 million confirmed cases.
In response to the ongoing pandemic, TCT 2020, initially planned for September 23 to 27, has been converted into a virtual event called TCT Connect, which will take place online October 14 to 18.
An early look at the RASTAVI trial, which is randomizing patients to ramipril or conventional treatment after successful TAVR, provides additional evidence that renin-angiotensin-aldosterone system (RAAS) inhibitors do not impact COVID-19 risk. In the Journal of the American College of Cardiology, researchers report that ramipril did not influence either the incidence or severity of the disease, although patient numbers are small. “This analysis supports the maintenance of RAAS inhibitor treatment during COVID-19 crisis,” the authors conclude.
Also in JACC, Emilia Bagiella, PhD, and colleagues discuss the far-reaching effects the pandemic has had on non-COVID-19-related clinical trials. “The consequences of this disruption of trial activity are unprecedented and likely to affect the evidence generated in the next few to several years,” they write. TCTMD’s Michael O’Riordan delved into the potential impacts in an earlier feature story.
A research letter in JAMA suggests that stay-at-home orders suppressed COVID-19 hospitalizations in four US states. The methodology of the study was met with some criticism on social media.
A case series in JAMA Network Open provides insights into differences between the clinical characteristics of patients with asymptomatic versus symptomatic COVID-19 in Wuhan, China. Asymptomatic patients appeared to have less damage to their immune systems, had a shorter duration of viral shedding, and had a lower risk of a recurring positive test result.
In the Ochsner Health system, black patients accounted for 77% of those hospitalized with COVID-19 and 71% of those who died, despite making up only 31% of overall patient population, according to a study in the New England Journal of Medicine. Black race was not, however, associated with a higher risk of in-hospital mortality.
In a perspective in Science, researchers argue that “masks and testing are necessary to combat asymptomatic spread in aerosols and droplets.”
 There has been some resistance to wearing face masks in public, but there are three ways to get people to wear masks to help fight COVID-19, University of Pennsylvania researchers write in an opinion piece in the New York Times. “The story of face masks in this country is still being written. We may lack the wisdom Hong Kong earned weathering prior epidemics, but it’s not too late to apply three basic principles from behavioral science: make it easy, understood, and expected, and we’ll soon see face masks everywhere, saving lives,” they write.
There has been some resistance to wearing face masks in public, but there are three ways to get people to wear masks to help fight COVID-19, University of Pennsylvania researchers write in an opinion piece in the New York Times. “The story of face masks in this country is still being written. We may lack the wisdom Hong Kong earned weathering prior epidemics, but it’s not too late to apply three basic principles from behavioral science: make it easy, understood, and expected, and we’ll soon see face masks everywhere, saving lives,” they write.
In a perspective in JAMA Internal Medicine, David Asch, MD, MBA, talks about how to make hospitals safe for patients during the pandemic and how to make them feel safe. “Perhaps the biggest challenge in helping patients feel safe is doing so in a way that is not itself scary,” he write. “Many of us have learned to find reassuring the image of an operating room staffed with gowned and gloved personnel. The same image with people in hazmat suits might be terrifying. For each context, there may be a fine line between signaling safety and signaling danger.”
The US Food and Drug Administration (FDA) has revised its enforcement policy for face masks and respirators during the COVID-19 public health emergency and issued new guidance for sponsors requesting emergency use authorizations (EUAs) for decontamination and bioburden reduction systems for face masks and respirators: “These guidances help to address potential shortages by facilitating the safe reuse and conservation of surgical masks and respirators for medical purposes through the use of decontamination and bioburden reduction systems and providing recommendations of alternatives and updated options for when FDA-cleared or NIOSH-approved N95 respirators are not available.” The agency also sent a letter to users of certain models of STERRAD sterilization systems about the need to use the correct decontamination cycle and to only decontaminate compatible N95 or equivalent respirators during the pandemic.
The FDA also has released answers to frequently asked questions about the regulatory impact of COVID-19, covering topics like “sponsor requests for formal meetings with industry, user fee applications goals and timelines, and prioritization of drug and biological application reviews during the public health emergency.” In addition, the agency announced that it has provided a SARS-CoV-2 reference panel as “an independent performance validation step for diagnostic tests . . . that are being used for clinical, not research, purposes.”
 Results of the study comparing 5- and 10-day courses of remdesivir (Gilead Sciences) for patients with severe COVID-19 not requiring mechanical ventilation have been published in NEJM. There was no difference between the two groups in terms of the clinical status of patients at day 14, but the study lacked a placebo control.
Results of the study comparing 5- and 10-day courses of remdesivir (Gilead Sciences) for patients with severe COVID-19 not requiring mechanical ventilation have been published in NEJM. There was no difference between the two groups in terms of the clinical status of patients at day 14, but the study lacked a placebo control.
May 27, 2020
 Two new papers, representing the largest number of patients studied to date, reinforce the view that the use of hydroxychloroquine and chloroquine is toxic to the heart and likely does more harm than good as a treatment for COVID-19, TCTMD’s Michael O’Riordan reports. One of the studies, published in the Lancet, showed that using the drugs was associated with greater risks of in-hospital mortality and new ventricular arrhythmias during hospitalization.
Two new papers, representing the largest number of patients studied to date, reinforce the view that the use of hydroxychloroquine and chloroquine is toxic to the heart and likely does more harm than good as a treatment for COVID-19, TCTMD’s Michael O’Riordan reports. One of the studies, published in the Lancet, showed that using the drugs was associated with greater risks of in-hospital mortality and new ventricular arrhythmias during hospitalization.
Health authorities in France greeted the news by moving to restrict the use of hydroxychloroquine for COVID-19, even in clinical trials, Politico reports.
In JACC: Basic to Translational Science, Jessica Mozersky, PhD, and colleagues argue that the decision by the National Institute of Allergy and Infectious Diseases (NIAID) to stop the ACCT-1 trial of remdesivir (Gilead Sciences) for COVID-19 was both ethically and scientifically justifiable. “Many aspects of evidence-based medicine are based on less than perfect evidence, and we must never forget that the participants enrolling in a clinical trial during a deadly pandemic are first and foremost patients who trust their physicians to do what is best for them,” they say.
Don’t rush a SARS-CoV-2 vaccine, Brit Trogen, MD, and colleagues caution in a JAMA viewpoint, because the scientific community has only one shot at getting the public to accept it based on evidence of safety and efficacy: “What cannot and must not be allowed is for desperation to result in the suspension of scientific principles and ethical research values. Physicians should not administer inadequately vetted vaccines; researchers should not endorse them without sufficient data.”
A news story in Science provides details on how COVID-19 spread through a South African hospital after a symptomatic patient presented to the emergency department on March 9. Within 8 weeks, 39 patients and 80 members of the hospital staff had been infected and 15 patients had died. An analysis of the outbreak “suggests all of the cases originated from a single introduction, and that patients rarely infected other patients. Instead, the virus was mostly carried around the hospital by staff and on the surfaces of medical equipment,” according to the story.
A screening program at three Yale New Haven Health hospitals in Connecticut found that 2.9% of asymptomatic pregnant women arriving to give birth in April tested positive for SARS-CoV-2, with the rate increasing from 0.6% in the first 2 weeks to 5.0% in the second half of the month, a research letter in JAMA shows. “These findings suggest a low (< 3%) prevalence of positive SARS-CoV-2 test results among asymptomatic patients in a pregnant population outside of the highly endemic region of New York City,” the authors conclude. Back in early April, an analysis of obstetric admissions at two New York hospitals found that more than 15% of pregnant women giving birth between March 22 and April 4, 2020, tested positive for SARS-CoV-2, of whom 88% were asymptomatic.
Researchers go over the advantages and limitations of digital contact tracing for COVID-19 in a paper in CMAJ. “The success of digital contact tracing will depend on access to diagnostic testing, widespread adoption, and the ability of the underlying technologies to identify exposures,” they say. “Combining traditional and digital contact tracing may leverage the advantages, and mitigate the limitations, of each approach.”
Consistent with anecdotal reports, SARS-CoV-2 infection is associated with changes in taste and loss of smell, including “the complete loss of perception of odors such as coffee and garbage,” according to a case-control study in CMAJ. “These symptoms should be considered as common and distinctive features of SARS-CoV-2 infection and should serve as an indication for testing and possible retesting of people whose first test result is negative,” the authors say.
In the New England Journal of Medicine, Marc Larochelle, MD, proposes a framework that clinicians can use to counsel patients about continuing to work during the pandemic. It incorporates both their occupational risk of contracting SARS-CoV-2 and their risk of death if they become infected. “Persons with high risk in both domains should consider stopping work, and those with high risk in one domain and medium risk in the other should discuss risk with their clinician,” Larochelle suggests. “Physicians should also inquire and counsel about risks to household or to other contacts who may be at high risk for poor outcomes.”
In the hopes that manufacturers can step up production of protective apparel during the pandemic, the US Food and Drug Administration has issued an Emergency Use Authorization (EUA) to address the shortages by waiving certain manufacturing requirements. The EUA covers “gowns and other apparel, such as operating-room shoe covers, for use by health care personnel as personal protective equipment (PPE) for use in health care settings.”
May 26, 2020
 More autopsy reports on COVID-19 patients, some from the United States, are helping researchers piece together a picture of a virus that damages endothelial cells, causing a clotting disorder that can lead to deep vein thrombosis and pulmonary emboli, TCTMD’s L.A. McKeown reports. In an autopsy study of patients from five centers in the United States, researchers report major pulmonary thromboemboli with pulmonary infarcts and/or hemorrhage in five of 23 patients and a pattern of cardiac comorbidity similar to what was seen in a recent German study.
More autopsy reports on COVID-19 patients, some from the United States, are helping researchers piece together a picture of a virus that damages endothelial cells, causing a clotting disorder that can lead to deep vein thrombosis and pulmonary emboli, TCTMD’s L.A. McKeown reports. In an autopsy study of patients from five centers in the United States, researchers report major pulmonary thromboemboli with pulmonary infarcts and/or hemorrhage in five of 23 patients and a pattern of cardiac comorbidity similar to what was seen in a recent German study.
Observational data show that patients diagnosed with COVID-19 have a “relatively low” rate of imaging-confirmed stroke—lower than seen in historical controls—but a far greater rate of cryptogenic stroke than that seen both historically and in a contemporary cohort not known to be infected, according to a story by TCTMD’s Yael Maxwell. The findings speak to the complex interplay between disease mechanisms and patient behavior: hypercoagulability is emerging as a hallmark of this disease at the same time that patients, fearing infection, are not heading to the hospital with acute symptoms.
Coming out of Memorial Day weekend in the United States, former US Food and Drug Administration (FDA) Commissioner Scott Gottlieb, MD, said on CNBC’s “Squawk Box” that states that have begun loosening restrictions in recent weeks are starting to see an uptick in COVID-19 hospitalizations. “It’s a small uptick, but it is an uptick and it’s unmistakable and it is probably a result of reopening,” he said. “We are going to have to watch it.”
There’s been a steady flow of negative data on hydroxychloroquine as a treatment for COVID-19 of late, prompting the World Health Organization (WHO) to temporarily pause the hydroxychloroquine arm of the Solidarity trial. The Indian Council of Medical Research (ICMR), on the other hand, has concluded that the drug is effective as prophylaxis against SARS-CoV-2 infection in healthcare workers based on three observational studies it conducted. In an updated advisory, the ICMR recommends prophylactic hydroxychloroquine for an expanded group of asymptomatic healthcare workers, frontline workers, and household contacts of laboratory-confirmed cases. “The drug has to be given under strict medical supervision with an informed consent,” the advisory states.
 More than one-third of COVID-19 deaths in the United States (37%) have occurred in residents and staff in long-term care facilities, according to a story in the New York Times. In 15 states, that proportion exceeded 50%. “The sheer numbers are horrifying. The underlying factors that have contributed are no surprise; they’ve been issues of concern for a long time,” one advocate said in the article, which contains a discussion about what needs to be done to address the issue.
More than one-third of COVID-19 deaths in the United States (37%) have occurred in residents and staff in long-term care facilities, according to a story in the New York Times. In 15 states, that proportion exceeded 50%. “The sheer numbers are horrifying. The underlying factors that have contributed are no surprise; they’ve been issues of concern for a long time,” one advocate said in the article, which contains a discussion about what needs to be done to address the issue.
A new paper in Morbidity and Mortality Weekly Report describes how universal and serial testing for SARS-CoV-2 successfully contained an outbreak at a long-term care skilled nursing facility for military veterans in Los Angeles, CA. After two symptomatic residents tested positive, all staff and residents were tested. All infected residents were isolated and serial testing was performed until all were negative.
In the Journal of the American Society of Echocardiography, researchers review the use of critical care transesophageal echocardiography during the COVID-19 pandemic. “Despite plausibility as an aerosol-generating procedure, based on the available evidence and experience in the front lines, our group of interdisciplinary experts from across North America support the use of TEE as an invaluable tool for managing the critically ill patient with COVID-19,” the authors write.
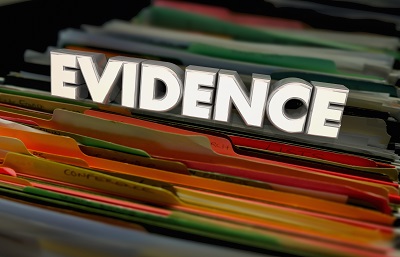 The need for high-quality observational research to complement randomized trials during the COVID-19 crisis has been underscored by the European Medicines Agency (EMA). “To generate evidence upon which decisions can be based, observational studies of real-world data must be well designed and adequately powered (ie, based on large populations),” the agency writes, pointing to a recent paper that laid out recommendations for performing high-quality research during the pandemic.
The need for high-quality observational research to complement randomized trials during the COVID-19 crisis has been underscored by the European Medicines Agency (EMA). “To generate evidence upon which decisions can be based, observational studies of real-world data must be well designed and adequately powered (ie, based on large populations),” the agency writes, pointing to a recent paper that laid out recommendations for performing high-quality research during the pandemic.
May 25, 2020

Roughly one out of every 100 healthcare workers employed at hospitals treating COVID-19 patients tests positive for SARS-CoV-2, the virus responsible for the disease, according to two new studies published this week in JAMA Network Open. In China, the virus was largely contracted from within the hospital, while community acquisition was more likely in Holland, TCTMD’s Michael O’Riordan reports.
Reports of plunging hospitalizations for myocardial infarction during the COVID-19 pandemic continue to mount, with nationwide data from Italy showing that acute MI admissions were almost halved during one week at the peak of the pandemic there. That drop mirrors one seen Northern California between March 4 and April 14, 2020, across the Kaiser Permanente health system covering more than 4.4 million residents, TCTMD Managing Editor Shelley Wood reports.
Meanwhile in Hartford, CT, STEMI cath lab activations were actually up 38% in February 2020 as compared with historical periods but fell by 16% and 21% in March and April. For NSTE-ACS, activations dropped by 21%, 37%, and 80%, respectively, for all three months. That data was published in the American Journal of Cardiology over the weekend. Likewise, hospitals in upstate New York saw a 40.7% drop in total ACS cases during March and April, researchers write in the American Heart Journal. That’s despite the fact that upstate New York “was not significantly affected by the number of COVID-19 patient admissions,” as compared with New York City and other hard-hit centers, the authors write.
An analysis of the World Health Organization’s pharmacovigilance database (“VigiBase”) comprised of 21 million reports from over 130 countries concludes that hydroxychloroquine and azithromycin are “a potentially lethal combination,” according to a press release from the American Heart Association. Published in Circulation, the study found statistically higher reports of prolonged-QT and ventricular tachycardia for each medicine alone (with greater reporting for both types of adverse events with azithromycin), while hydroxychloroquine was significantly linked with the development of conduction disorders and heart failure.
 On Friday the US Food and Drug Administration and the Department of Agriculture released new recommendations to address shortages of personal protective equipment (PPE) as well as cloth face coverings, disinfectants, and sanitation supplies in the food and agriculture industry. “The current constraints on these supplies are causing concerns about the potential for interruptions in the food supply chain,” an FDA statement reads. “These supplies are critical for worker safety, the continuity of the food supply, food safety, and employee/consumer confidence.”
On Friday the US Food and Drug Administration and the Department of Agriculture released new recommendations to address shortages of personal protective equipment (PPE) as well as cloth face coverings, disinfectants, and sanitation supplies in the food and agriculture industry. “The current constraints on these supplies are causing concerns about the potential for interruptions in the food supply chain,” an FDA statement reads. “These supplies are critical for worker safety, the continuity of the food supply, food safety, and employee/consumer confidence.”
Full results for the Adaptive COVID-19 Treatment Trial of remdesivir have now been published in the New England Journal of Medicine. Investigators led by John Beigel, MD, found that remdesivir was superior to placebo in shortening the time to recovery in hospitalized adults who also have lower respiratory tract involvement. Topline results released in late April led to the FDA’s emergency use authorization of the antiviral medication as a treatment for COVID-19.
Also in the NEJM, Michael Argenziano, MD, and colleagues describe their experience scheduling surgeries in a crisis. In a letter published as part of the rapid COVID-19 Notes series, the authors detail the “unprecedented decision” at New York-Presbyterian Columbia University Irving Medical Center to suspend all elective surgeries to protect workers in the face of restricted PPE, while expanding critical care facilities, and the steps taken to ensure that the most urgent surgeries could still happen, and how.
 Writing in the European Heart Journal, Ali R. Wahadat, MD, and colleagues offer some suggestions for how to hold multidisciplinary heart team meetings in the midst of a pandemic when meeting in person is not an option. All have different advantages and drawbacks, the authors note.
Writing in the European Heart Journal, Ali R. Wahadat, MD, and colleagues offer some suggestions for how to hold multidisciplinary heart team meetings in the midst of a pandemic when meeting in person is not an option. All have different advantages and drawbacks, the authors note.
May 22, 2020
A new vaccine looks safe and can produce virus-specific antibodies and T cells in 14 days, according to a small, phase I clinical trial published in the Lancet. The 28-day results with the adenovirus type-5 vectored COVID-19 (Ad5-nCoV) vaccine was tested in three doses in 108 health volunteers aged 18 to 60 years in Wuhan, China. “Analyses showed that 28 days after vaccination, the majority of recipients showed either a positive T-cell response or had detectable neutralizing antibodies against SARS-CoV-2,” the authors write. Volunteers will be followed for 6 months and a phase II trial is in the works.
Also in the Lancet, a large observational study has found no benefit to chloroquine or hydroxychloroquine, with or without an antibiotic (azithromycin or clarithromycin), among in nearly 15,000 COVID-19 positive patients compared with 81,000 controls. All four agents were associated with worse survival, and 8% of patients taking both hydroxychloroquine and an antibiotic developed heart arrhythmias. “This is the first large-scale study to find statistically robust evidence that treatment with chloroquine or hydroxychloroquine does not benefit patients with COVID-19,” lead author Mandeep Mehra, MD (Brigham and Women’s Hospital, Boston, MA), said in a press statement. “Instead, our findings suggest it may be associated with an increased risk of serious heart problems and increased risk of death.”
 In what authors led by Annemarie B. Docherty, PhD, say is the largest cohort study to date worldwide—involving 20,133 patients with COVID-19 admitted to 208 acute care hospitals in England, Wales, and Scotland—the key risk factors for severe illness or death in COVID-19 are age over 50, male sex, obesity, and underlying heart, lung, liver and kidney disease. The study, published in the BMJ, represents one-third of all patients in the United Kingdom admitted to the hospital, a press release notes, and the number of cases included in the registry has more than doubled since the paper was submitted. Chillingly, at the time of reporting, 34% of patients were still in the hospital and 26% of all hospitalized patients had died.
In what authors led by Annemarie B. Docherty, PhD, say is the largest cohort study to date worldwide—involving 20,133 patients with COVID-19 admitted to 208 acute care hospitals in England, Wales, and Scotland—the key risk factors for severe illness or death in COVID-19 are age over 50, male sex, obesity, and underlying heart, lung, liver and kidney disease. The study, published in the BMJ, represents one-third of all patients in the United Kingdom admitted to the hospital, a press release notes, and the number of cases included in the registry has more than doubled since the paper was submitted. Chillingly, at the time of reporting, 34% of patients were still in the hospital and 26% of all hospitalized patients had died.
Authors writing in Circulation: Cardiovascular Quality and Outcomes, make the case for attempting cardiopulmonary resuscitation (CPR) among cardiac arrest patients with COVID-19, arguing that blanket DNR policies are inappropriate. The modelling study draws on Get With The Guidelines registry data for patients who required CPR for in-hospital cardiac arrest while in the ICU for pneumonia or sepsis and receiving mechanical ventilation. The “large variation in survival rates suggests that a blanket prescription of do-not-resuscitate orders in patients with COVID-19 may be unwarranted,” they conclude.
The US Food and Drug Administration has posted a list of antibody tests that the agency has removed from its list of those available under the Policy for Coronavirus Disease-2019 Tests During the Public Health Emergency. These include tests voluntarily withdrawn from the notification list as well as those for which an Emergency Use Authorization (EUA) has not been issued or request.
 Chinese researchers writing in JAMA Network Open report that 10 of 60 patients previously admitted to the hospital tested positive again on RT-PCR assays 4 to 24 days after being discharged. Investigators concluded that, rather than being new infections, these are presumed to reflect persistent viral shedding and the extent to which patients remain infectious is unclear.
Chinese researchers writing in JAMA Network Open report that 10 of 60 patients previously admitted to the hospital tested positive again on RT-PCR assays 4 to 24 days after being discharged. Investigators concluded that, rather than being new infections, these are presumed to reflect persistent viral shedding and the extent to which patients remain infectious is unclear.
In the Journal of Medical Ethics, Udo Schuklenk, PhD, argues that democratically elected political leaders, by failing adequately equip healthcare delivery systems with the resources to protect their workers, now bear the responsibility for the high infection and death rates in this group. “After discussing and discounting various ethical arguments in support of a professional obligation to treat, even without or with suboptimal personal protective equipment, I conclude that these policy decisions were sufficiently grave that they provide a sound ethical rationale to justify healthcare workers’ refusal to provide care to infected patients.” Schuklenk writes.
 The COVID-19 pandemic is having a tangible effect on interventional cardiology training, according to a new survey of fellows and program directors in the New York City area. As Yael Maxwell reports for TCTMD, half of program directors said their fellows had been deployed to other clinical areas since the start of the pandemic, and 21% said they expected their fellows to finish the year below the ACGME-mandated threshold of 250 PCIs on average.
The COVID-19 pandemic is having a tangible effect on interventional cardiology training, according to a new survey of fellows and program directors in the New York City area. As Yael Maxwell reports for TCTMD, half of program directors said their fellows had been deployed to other clinical areas since the start of the pandemic, and 21% said they expected their fellows to finish the year below the ACGME-mandated threshold of 250 PCIs on average.
May 21, 2020
 How will COVID-19 change the practice of cardiology in the months and years to come? TCTMD’s Yael Maxwell spoke with 10 physicians across the spectrum of cardiovascular care to hear their predictions, hopes, and fears.
How will COVID-19 change the practice of cardiology in the months and years to come? TCTMD’s Yael Maxwell spoke with 10 physicians across the spectrum of cardiovascular care to hear their predictions, hopes, and fears.
Two new published studies out of Wuhan, China, confirm that elevations and changes in troponin I may be an early warning sign of poor long-term prognosis. Reviewing the papers with TCTMD’s Laura McKeown, Mohammad Madjid, MD, admitted it’s “kind of scary” how much the risk of death from this virus appears to track with cardiac injury.
Even very sick children who develop what is now being called multisystem inflammatory syndrome after infection with the SARS-CoV-2 virus appear to recover well when treated with therapies commonly used in the setting of Kawasaki disease, Todd Neale reports.
 The US Commander in Chief has trumpeted hydroxychloroquine for preventing COVID-19 infection and announced this week that he’s been taking it daily: a deep dive into some recently published studies and the first peer-reviewed clinical trial suggests the drug likely isn’t helping and is probably causing harm. “This is unlikely to be of net benefit to [President Trump] or any other patient population at this point,” said Timothy F. Simpson, MD, PharmD.
The US Commander in Chief has trumpeted hydroxychloroquine for preventing COVID-19 infection and announced this week that he’s been taking it daily: a deep dive into some recently published studies and the first peer-reviewed clinical trial suggests the drug likely isn’t helping and is probably causing harm. “This is unlikely to be of net benefit to [President Trump] or any other patient population at this point,” said Timothy F. Simpson, MD, PharmD.
That hasn’t stopped Brazil from issuing written guidance encouraging doctors to give the antimalarial drug to all patients with COVID-19, regardless of symptom severity. Two health ministers have resigned or been fired over their refusal to support President Jair Bolsonaro’s enthusiastic support for the therapy, the New York Times reports. Meanwhile in India, 10,000 policemen over age 40 have been given hydroxychloroquine in the hopes it will halt the number of deaths in the city’s force, the Times of India reports.
Also on the chloroquine/ hydroxychloroquine front, Ohad Oren, MD, and colleagues writing in Circulation: Arrhythmia and Electrophysiology, propose a new framework for understanding safety signals with these agents in order to improve clinical trial design and interpretation. In the same journal, Stephanie M. Kochav, MD, and colleagues review the range of cardiac rhythm abnormalities seen with this infection.
In an interview with Yael Maxwell, Devan Kansagara, MD, explains plans for a “living review” of RAAS inhibitors in the setting of COVID-19: what’s been established with confidence and what remains unclear. Details are reported in Annals of Internal Medicine.
 In its daily roundup, the US Food and Drug Administration says it has signed a Memorandum of Understanding with the US Department of Agriculture to bolster access to a “safe and robust food supply” during the pandemic. They’ve also issued an Emergency Use Authorization for the COVID-19 Airway Management Isolation Chamber (CAMIC) for use by healthcare providers within the US Army and Military Health System. “The CAMIC system is a barrier device constructed by draping a large clear plastic bag over a box-like frame that is placed over the head, neck, and shoulders of the patient to isolate (i.e., capture and remove) airborne particulates,” an FDA statement reads.
In its daily roundup, the US Food and Drug Administration says it has signed a Memorandum of Understanding with the US Department of Agriculture to bolster access to a “safe and robust food supply” during the pandemic. They’ve also issued an Emergency Use Authorization for the COVID-19 Airway Management Isolation Chamber (CAMIC) for use by healthcare providers within the US Army and Military Health System. “The CAMIC system is a barrier device constructed by draping a large clear plastic bag over a box-like frame that is placed over the head, neck, and shoulders of the patient to isolate (i.e., capture and remove) airborne particulates,” an FDA statement reads.
The incidence of imaging-confirmed ischemic stroke among patients hospitalized with COVID-19 in a large New York health system is “low,” write Shadi Yaghi, MD, and colleagues in Stroke. But compared with historical controls, the strokes that occur are more severe and more lethal and they are affecting younger patients, investigators say.
Why aren’t people living with HIV at higher risk for developing severe COVID-19? Jeffrey Laurence, MD, explores this “profound enigma” and proposes some possible answers in AIDS Patient Care and STDs.
Loss of smell and taste are a hallmark of COVID-19: now a Clinical Update in JAMA reviews the diagnosis and management of olfactory dysfunction. “This symptom should prompt self-isolation and testing for SARS-CoV-2 when possible,” write Katherine Lisa Whitcroft, MBChB, and colleagues.

May 20, 2020
 New prospective evidence from New York City confirms a preponderance of cardiometabolic risk factors, a high incidence of critical illness among ethnic minorities, and bleak outcomes for the sickest COVID-19 patients, as TCTMD’s Michael O’Riordan reports. Of 257 COVID-19 patients who became critically ill with acute hypoxemic respiratory failure, 101 had died and 94 remained in the hospital as of April 28, 2020. Nearly 80% of these patients required mechanical ventilation.
New prospective evidence from New York City confirms a preponderance of cardiometabolic risk factors, a high incidence of critical illness among ethnic minorities, and bleak outcomes for the sickest COVID-19 patients, as TCTMD’s Michael O’Riordan reports. Of 257 COVID-19 patients who became critically ill with acute hypoxemic respiratory failure, 101 had died and 94 remained in the hospital as of April 28, 2020. Nearly 80% of these patients required mechanical ventilation.
Some hospitals in New York state will allow visitors to start returning under a pilot program that will begin on May 26, the New York Times reports. The program involves 16 hospitals, including nine in NYC. New York Governor Andrew Cuomo said visitors will be required to wear personal protective equipment like masks and have their temperature checked.
Data from Kaiser Permanente Northern California published in a letter in the New England Journal of Medicine confirm the drop in the incidence of hospitalization for acute MI during the COVID-19 pandemic that has been reported worldwide. Weekly rates fell by up to 48% during the COVID-19 period.
The American Stroke Association (ASA) has released a four-episode podcast series that explores the potential impact of COVID-19 on stroke survivors and their families and caregivers, addressing health risks, emotional well-being, how to stay active at home, and how to deal with financial difficulties.
In a viewpoint in JAMA Internal Medicine, researchers are calling for transparency and reliable evidence when it comes to emergency use authorizations (EUAs) for COVID-19 therapies. Specifically for hydroxychloroquine and chloroquine, “neither the EUA documentation nor the fact sheet for clinicians cites specific trials used in FDA decision-making, rendering it difficult to ascertain the totality of scientific evidence the FDA considered,” they argue, adding that “there is a great risk of damage from issuing an EUA based on insufficient data.”
“Lung ultrasound is a skill that can be acquired by cardiologists to enhance their physical and echocardiographic examination,” researchers say in a Canadian Journal of Cardiology paper meant as a practical overview for their colleagues in cardiology. They provide guidance specific to COVID-19.
 A cautionary note as states start to reopen amidst the COVID-19 pandemic: new research in Morbidity and Mortality Weekly Report shows a high infection rate among attendees of a church in Arkansas. Of 92 people who attended church activities over a 6-day period in March, 38% developed lab-confirmed COVID-19, with three deaths. The highest rates were seen in those ages 19 to 64 (59%) and 65 and older (50%). An additional 26 cases linked to the church occurred in the community, with one death. “Faith-based organizations that are operating or planning to resume in-person operations, including regular services, funerals, or other events, should be aware of the potential for high rates of transmission of SARS-CoV-2,” the authors say.
A cautionary note as states start to reopen amidst the COVID-19 pandemic: new research in Morbidity and Mortality Weekly Report shows a high infection rate among attendees of a church in Arkansas. Of 92 people who attended church activities over a 6-day period in March, 38% developed lab-confirmed COVID-19, with three deaths. The highest rates were seen in those ages 19 to 64 (59%) and 65 and older (50%). An additional 26 cases linked to the church occurred in the community, with one death. “Faith-based organizations that are operating or planning to resume in-person operations, including regular services, funerals, or other events, should be aware of the potential for high rates of transmission of SARS-CoV-2,” the authors say.
An NEJM video shows a procedure for donning and doffing one type of personal protective equipment recommended by the US Centers for Disease Control and Prevention (CDC) to minimize risk during the care of patients with COVID-19. The accompanying text gives additional detail about effective protection.
Two perspectives in NEJM tackle disability rights in the context of critical care crisis triage protocols during the COVID-19 era. Mildred Solomon, EdD, and colleagues say: “To ensure the trustworthiness of the health system, disability rights advocates and healthcare leaders should work together to finalize crisis triage plans that save the most lives, protect the equal worth of all persons, and enhance communities’ capacity to heal in the wake of a once-in-a-century pandemic.” Michelle Mello, JD, PhD, and colleagues provide “six guideposts that states and hospitals should follow to respect disability rights.”
Serological testing for SARS-CoV-2 is key to the pandemic response, but it’s more useful for population-level assessments rather than for the prediction of individual immunity, researchers say in Science Immunology. “We stress that investing now in a fundamental and operational research agenda will allow us to rapidly develop serosurveillance as a powerful tool for population-level public health; however, the complexity of using serological assays within low prevalence settings to inform individual-based risk assessments—ie, to inform decisions regarding return to work—is dangerously premature,” they say.
May 19, 2020
Researchers describe an unusual ACS presentation in a SARS-CoV-2-positive patient in the European Heart Journal: Cardiovascular Imaging. ECG showed no evidence of acute ischemia, and high-sensitivity troponin T and C-reactive protein were elevated. Coronary angiography revealed a focal and moderate stenosis in the proximal right coronary artery. Optical coherence tomography suggested intraplaque hemorrhage, with no disruption of the intima or thrombus. A DES was placed. “The systemic inflammatory response of SARS-CoV-2 infection could trigger a focal inflammatory response in the coronary wall and be responsible for the instability of an atherosclerotic plaque,” the authors conclude.

The rate of deep vein thrombosis is very high in patients hospitalized with severe COVID-19, two studies out of China show. In a look at 48 patients, lower-extremity DVT was detected in 85.4%. And in an analysis of 143 patients, the rate was 46.1%. The death rate was higher in patients with versus without DVT in both studies, which were published in Circulation.
Those hoping for a major drop in COVID-19 activity in the warmer weather might be disappointed, a modeling study in Science suggests. “Our findings suggest, without effective control measures, strong outbreaks are likely in more humid climates, and summer weather will not substantially limit pandemic growth,” the authors say.
 Child vaccination coverage has declined during the COVID-19 pandemic, a study published in Morbidity and Mortality Weekly Report shows. “The observed declines in vaccination coverage might leave young children and communities vulnerable to vaccine-preventable diseases such as measles,” the authors write.
Child vaccination coverage has declined during the COVID-19 pandemic, a study published in Morbidity and Mortality Weekly Report shows. “The observed declines in vaccination coverage might leave young children and communities vulnerable to vaccine-preventable diseases such as measles,” the authors write.
The US Centers for Disease Control and Prevention (CDC) will conduct a large COVID-19 antibody study in 25 metropolitan areas in the United States, Reuters reports. The study will include up to 325,000 people with the aim of tracking how SARS-CoV-2 is spreading across the country.
COVID-19 might cause delirium in the acute stage and additional psychiatric and neuropsychiatric disorders over the longer term if data from prior coronavirus outbreaks—including SARS and MERS—are any indication, according to a study in the Lancet. Indeed, initial data on patients with COVID-19 who were in the ICU indicated that confusion and agitation were experienced by 65% and 69%, respectively.
Several JAMA viewpoints tackle issues relevant to responses to the COVID-19 pandemic, including regulation and privacy as they pertain to the expansion of telehealth; creation of the ACTIV public-private partnership aimed at speeding the creation of treatments and vaccines; planning for a large-scale vaccination program; and the need for a national health information technology infrastructure in the United States.
The US National Institutes of Health (NIH) has launched a study to examine the effects of COVID-19 during and after pregnancy. “Researchers will analyze the medical records of up to 21,000 women to evaluate whether changes to healthcare delivery that were implemented as a result of the pandemic have led to higher rates of pregnancy-related complications and cesarean delivery,” according to a press release. The study will also examine the risk of women transmitting the virus to their fetus and outcomes among pregnant women with confirmed COVID-19.
May 18, 2020
In the European Heart Journal, Italian researchers dig into the reduction in hospitalizations for acute MI during the COVID-19 pandemic that has been reported around the world. Compared with an equivalent week from the pre-COVID era, cardiac care units saw a 48.4% drop in admissions for acute MI in a recent week during the outbreak. The decrease was greater in women than in men. STEMI case-fatality rate and complications spiked.
Also in that journal, the European Association of Percutaneous Coronary Interventions (EAPCI) released a position statement on the invasive management of ACS during the COVID-19 pandemic. The document includes clinical scenarios and management algorithms, as well as advice regarding protection of healthcare workers and reorganization of ACS networks, in-hospital units, and cath labs.
 The Society for Cardiovascular Angiography and Interventions (SCAI), the Canadian Association of Interventional Cardiology (CAIC), and the American College of Cardiology (ACC) Interventional Council have created a multicenter North American COVID-19 STEMI (NACMI) registry.
The Society for Cardiovascular Angiography and Interventions (SCAI), the Canadian Association of Interventional Cardiology (CAIC), and the American College of Cardiology (ACC) Interventional Council have created a multicenter North American COVID-19 STEMI (NACMI) registry.
A research letter in the Journal of the American College of Cardiology shows that the number of surgical repairs of acute type A aortic dissections fell in New York City after the start of the COVID-19 pandemic. Average monthly case volume dropped from 12.8 pre-COVID to 3.0 after March 1. “While no causal relationship can be firmly established between the drop in type A aortic dissections, the COVID-19 outbreak in NYC, and the increase in at-home deaths since the last week of March 2020, this gives pause for thought,” the researchers say.
Children with the Kawasaki-like disease associated with SARS-CoV-2 infection—called the multisystem inflammatory syndrome in children (MIS-C)—may develop acute cardiac decompensation, according to a study in Circulation. “Treatment with immune globulin appears to be associated with recovery of left ventricular systolic function,” the authors report.
A new review on COVID-19 and heart failure has been published in the European Journal of Heart Failure, with the recent literature on about cardiac damage associated with the disease summarized in user-friendly tables and figures.
RV dilation on echocardiography is significantly associated with in-hospital mortality in patients hospitalized with COVID-19, a study out of New York City shows. “The mechanism of right ventricular dilation is likely multifactorial and includes thrombotic events, hypoxemic vasoconstriction, cytokine milieu, and direct viral damage,” the researchers say in JACC: Cardiovascular Imaging.
Of 53 patients hospitalized with COVID-19 who were treated with remdesivir (Gilead Sciences) on a compassionate-use basis, clinical improvement was seen in 36 (68%), according to a study in the New England Journal of Medicine. “Measurement of efficacy will require ongoing randomized, placebo-controlled trials of remdesivir therapy,” the authors note.
The US Food and Drug Administration (FDA) has issued an emergency use authorization for the G Medical VSMS ECG Patch to be used in the hospital for remote monitoring in adult patients with COVID-19 who are receiving drugs known to be associated with QT interval prolongation, such as hydroxychloroquine and chloroquine. The patch should not be used in critical care patients.
Moderna announced promising early-stage results for its experimental COVID-19 vaccine, with eight patients who received the vaccine developing antibody levels similar to those seen in patients who have recovered from the disease, Reuters reports. A larger trial is expected to start in July.
In NEJM, physicians describe a case of severe COVID-19 before expanding on strategies for how to manage those with severe disease and describing areas of remaining uncertainty. “Given the uncertainties regarding effective treatment, clinicians should discuss available clinical trials with patients. In addition, clinicians should discuss the value of autopsies with the families of patients who do not survive,” the authors recommend.
Stay-at-home orders seem to be slowing the spread of SARS-CoV-2, according to data in JAMA Network Open. Compared with seven Illinois counties subject to a stay-at-home order, eight bordering Iowa counties not subject to such an order had an increased rate of COVID-19 cases.
May 15, 2020
 Investigators in Bergamo province, Italy, say that the number of children who have tested positive for the virus and presented with severe “Kawasaki-like” symptoms continues to climb, amounting to more than a 30-fold increase over the number of Kawasaki patients seen in prior years, as reported by TCTMD’s Managing Editor Shelley Wood.
Investigators in Bergamo province, Italy, say that the number of children who have tested positive for the virus and presented with severe “Kawasaki-like” symptoms continues to climb, amounting to more than a 30-fold increase over the number of Kawasaki patients seen in prior years, as reported by TCTMD’s Managing Editor Shelley Wood.
Underscoring the growing concern about the issue, the Centers for Disease Control & Prevention (CDC) on Thursday issued a health advisory on the Kawasaki-like disease that has been associated with COVID-19 in children and is the subject of increasing reports around the world. The advisory provides background on the multisystem inflammatory syndrome in children (MIS-C), along with a case definition. “Healthcare providers who have cared or are caring for patients younger than 21 years of age meeting MIS-C criteria should report suspected cases to their local, state, or territorial health department,” CDC stated.
 The US Food and Drug Administration (FDA) has alerted the public about potentially inaccurate—specifically, false-negative—results with the Abbott ID NOW point-of-care test for COVID-19 based on early data. “This test can still be used and can correctly identify many positive cases in minutes. Negative results may need to be confirmed with a high-sensitivity authorized molecular test,” said Tim Stenzel, MD, PhD, of the FDA’s Center for Devices and Radiological Health.
The US Food and Drug Administration (FDA) has alerted the public about potentially inaccurate—specifically, false-negative—results with the Abbott ID NOW point-of-care test for COVID-19 based on early data. “This test can still be used and can correctly identify many positive cases in minutes. Negative results may need to be confirmed with a high-sensitivity authorized molecular test,” said Tim Stenzel, MD, PhD, of the FDA’s Center for Devices and Radiological Health.
When comparing the health impacts of COVID-19 and the seasonal flu, use “apples-to-apples” comparisons to better reflect the threat of the novel coronavirus, Jeremy Samuel Faust, MD, and Carlos del Rio, MD, argue in a viewpoint in JAMA Internal Medicine. “From our analysis, we infer that either the CDC’s annual estimates substantially overstate the actual number of deaths caused by influenza or that the current number of COVID-19 counted deaths substantially understates the actual number of deaths caused by SARS-CoV-2, or both,” they write.
Italian researchers report in the BMJ, in fact, that only considering COVID-19 death counts will substantially underestimate the lethal impact of the pandemic. “The study findings show how COVID-19 can have a considerable impact on the health of a small community,” the authors write. “Furthermore, the results suggest that the full implications of the COVID-19 pandemic can only be completely understood if, in addition to confirmed deaths related to COVID-19, consideration is also given to all-cause mortality in a given region and time frame.”
Across 13 hospitals in the metropolitan New York area, acute kidney injury developed in 36.6% of patients hospitalized with COVID-19, according to a study in Kidney International. In that group, 35% died, 26% were discharged, and 39% remained hospitalized.
The response to COVID-19 in the United Kingdom has been “too little, too late, too flawed,” public health experts argue in the BMJ. “With over 30,000 hospital and community deaths by 12 May, where did the plan go wrong? What was the role of public health in the biggest public health crisis since the Spanish flu of 1918? And what now needs to be done?” they ask. “What is clear is that the UK’s response so far has neither been well prepared nor remotely adequate.”
In CMAJ, researchers report on a probable case of perinatal SARS-CoV-2 transmission between a mother and her newborn. “Neonates born to women with confirmed or suspected [SARS-CoV-2] infection should have testing of the nasopharynx, placenta, and cord blood as soon as possible after birth, after thorough cleaning of the neonate,” the authors say.
 A National Institute of Allergy and Infectious Diseases (NIAID)-sponsored trial of hydroxychloroquine and azithromycin for the treatment of COVID-19 has begun. The phase IIb trial aims to enroll about 2,000 adults. Teva Pharmaceuticals is donating study medications.
A National Institute of Allergy and Infectious Diseases (NIAID)-sponsored trial of hydroxychloroquine and azithromycin for the treatment of COVID-19 has begun. The phase IIb trial aims to enroll about 2,000 adults. Teva Pharmaceuticals is donating study medications.
Two new studies in the BMJ provide some insight into whether hydroxychloroquine, which has already been used extensively during the pandemic, is making an impact—and the results aren’t promising. A randomized study out of China in patients with mostly mild-to-moderate disease showed that adding the drug to standard care did not increase the probability of having negative seroconversion by 28 days. And an observational study of patients with COVID-19 pneumonia who required oxygen but not intensive care showed hydroxychloroquine was not associated with improved survival without transfer to the ICU compared with standard care alone.
National Institutes of Health (NIH) Director Francis Collins, MD, PhD, sat down (virtually) with Eliseo Pérez-Stable, MD, director of the NIH’s National Institute on Minority Health and Health Disparities, to talk about how the COVID-19 pandemic has highlighted pre-existing health disparities in the United States. “In analyzing health outcomes, researchers often think about responses related to a metabolic pathway or to a gene or to a response to a particular drug. But as we use the power of science to understand and contain the COVID-19 pandemic, I’d like to re-emphasize the importance of considering race, ethnicity, socioeconomic status, the built environment, the social environment, and systems. Much of the time these factors may only play secondary roles, but, as in all science related to humans, I think they have to be considered. This experience should be a lesson for us to learn more about that,” Pérez-Stable said.
 Researchers are predicting that nearly 250 million people across the African continent will become infected with SARS-CoV-2 in the first year of the pandemic and up to 190,000 could die from COVID-19, according to a study accepted for publication in BMJ Global Health. “Their estimates indicate that the pandemic may spread more slowly in Africa, with fewer severe cases and deaths than in other parts of the world, such as the US and Europe, but it is likely to linger for longer, and possibly for several years,” a press release states.
Researchers are predicting that nearly 250 million people across the African continent will become infected with SARS-CoV-2 in the first year of the pandemic and up to 190,000 could die from COVID-19, according to a study accepted for publication in BMJ Global Health. “Their estimates indicate that the pandemic may spread more slowly in Africa, with fewer severe cases and deaths than in other parts of the world, such as the US and Europe, but it is likely to linger for longer, and possibly for several years,” a press release states.
May 14, 2020
How competitive athletes and highly active people who’ve recovered from COVID-19 can safely resume exercise may not seem like a high priority for centers still dealing with the acute phase of this pandemic. But the authors of a new consensus document say answering this question is increasingly pressing and may help prevent late complications, as reported by TCTMD’s Caitlin Cox.
 Researchers in the Bergamo province of Italy are reporting a 30-fold increased incidence of Kawasaki-like disease in children during the pandemic. Among other findings reported the Lancet, children diagnosed after versus before the outbreak began had much higher rates of cardiac involvement and Kawasaki disease shock syndrome. Reports of a syndrome similar to Kawasaki disease in children are increasing around the world.
Researchers in the Bergamo province of Italy are reporting a 30-fold increased incidence of Kawasaki-like disease in children during the pandemic. Among other findings reported the Lancet, children diagnosed after versus before the outbreak began had much higher rates of cardiac involvement and Kawasaki disease shock syndrome. Reports of a syndrome similar to Kawasaki disease in children are increasing around the world.
The COVID-19 pandemic has disrupted the practice of cardiac surgery, a study in Circulation confirms. A questionnaire sent to centers participating in the ROMA trial showed “reduced cardiac surgery activity, redeployed personnel, and curtailed educational and research activities,” an interruption that “adds to the concerning observation that excess non-COVID-19 mortality may now surpass mortality directly related to COVID-19 infections,” the authors say.
The International Atomic Energy Agency (IAEA) is conducting a survey to evaluate the impact of COVID-19 on cardiac imaging practices and working conditions. The deadline to complete the INCAPS COVID survey, found here, is May 20. Only one survey should be completed for each laboratory/center.
Among patients with LV assist devices, the COVID-19 pandemic is complicating self-care such as maintaining the system and driveline, sticking to a healthy lifestyle, and remaining adherent prescribed medications, researchers say in a viewpoint in the European Journal of Heart Failure. They provide some tips for supporting patients, noting, “Healthcare providers need to be flexible and creative to support patients optimally and future educational programs should address these challenges that might become relevant more often.”
 More than one-quarter (27.5%) of the 69 most-watched videos about COVID-19 on YouTube contain misleading information, according to a study in BMJ Global Health. Those videos accounted for more than 62 million views. “As the current COVID-19 pandemic worsens, public health agencies must better use YouTube to deliver timely and accurate information and to minimize the spread of misinformation,” the authors conclude.
More than one-quarter (27.5%) of the 69 most-watched videos about COVID-19 on YouTube contain misleading information, according to a study in BMJ Global Health. Those videos accounted for more than 62 million views. “As the current COVID-19 pandemic worsens, public health agencies must better use YouTube to deliver timely and accurate information and to minimize the spread of misinformation,” the authors conclude.
The Stroke Council of the American Heart Association/American Stroke Association has issued guidance on the prehospital triage of patients with acute stroke during the ongoing crisis. “During the COVID-19 pandemic, it is more important than ever to ensure that stroke patients are taken to the right hospital that can meet their urgent needs at the outset,” lead author Mayank Goyal, MD, said in a press release.
It's time to move on from the small, uncontrolled trials that have dominated the search for COVID-19 treatments up to this point, according to a Nature editorial: “Some trials need to be small, initial explorations of potential treatments; but, after that, researchers must think big. It’s important to move quickly to larger, collaborative trials—ones that span borders and share expertise—that have a greater chance of showing what really works.”
There have been reports of fewer confirmed COVID-19 cases and reduced mortality in countries with versus without universal childhood bacille Calmette-Guerin (BCG) vaccination for tuberculosis. A research letter in JAMA does not support that idea, however. It shows that the BCG-vaccinated group was not less likely than the unvaccinated group to have a positive test result for SARS-CoV-2.
In a perspective in the New England Journal of Medicine, Victor Dzau, MD, and colleagues tackle the need to prevent the “parallel pandemic” of physical and emotional harm to healthcare workers during the COVID-19 crisis. “We have a brief window of opportunity to get ahead of two pandemics, the spread of the virus today and the harm to well-being tomorrow,” they write. “If we fail, we will pay the price for years to come. In the race to respond to the COVID-19 crisis, we must not neglect to care for those who care for us.”
Also in NEJM, an autopsy series of 27 patients shows that SARS-CoV-2 can be detected throughout the body, including in the lungs, pharynx, heart, liver, brain, and kidneys. The authors “speculate that organotropism influences the course of COVID-19 disease and, possibly, aggravates preexisting conditions.”
 Researchers have confirmed that SARS-CoV-2 can be transmitted between domestic cats. “Given the need to stop the . . . pandemic through various mechanisms, including breaking transmission chains, a better understanding of the role cats may play in the transmission of SARS-CoV-2 to humans is needed,” they write in a letter in NEJM.
Researchers have confirmed that SARS-CoV-2 can be transmitted between domestic cats. “Given the need to stop the . . . pandemic through various mechanisms, including breaking transmission chains, a better understanding of the role cats may play in the transmission of SARS-CoV-2 to humans is needed,” they write in a letter in NEJM.
May 13, 2020
 Hospitals are planning a cautious restart for elective procedures as COVID-19 wanes, as TCTMD’s Michael O’Riordan details in a feature story. Working off the backlog of elective CV cases put on hold for the last 8 weeks will be more of a marathon than a sprint, doctors say.
Hospitals are planning a cautious restart for elective procedures as COVID-19 wanes, as TCTMD’s Michael O’Riordan details in a feature story. Working off the backlog of elective CV cases put on hold for the last 8 weeks will be more of a marathon than a sprint, doctors say.
Researchers from Wuhan, China, report on the characteristics and clinical significance of myocardial injury in patients with severe COVID-19 in the European Heart Journal. Of hospitalized patients, those who died were much more likely to have myocardial injury (75.8% vs 9.7%). A separate group of researchers from China, reporting in the Journal of the American College of Cardiology, confirmed the association between acute myocardial injury at admission and a higher risk of all-cause mortality.
The role of cardiovascular imaging for myocardial injury in patients hospitalized with COVID-19 is discussed in a paper in the European Heart Journal – Cardiovascular Imaging. The authors aim to “provide guidance to clinicians regarding the appropriateness of cardiac imaging in the context of troponin elevation and myocardial injury, how best to decipher the mechanism of myocardial injury, and how to guide patient management.”
A review in the Journal of the American Heart Association tackles what is known about the impact of COVID-19 on the cardiovascular and cerebrovascular systems. “Based on our review of published studies, COVID-19 patients may be more likely to experience acute cardiac injury, arrhythmia, coagulation defects and acute stroke and are likely to have poorer outcomes as a result,” they write.
A clinical risk score may help predict the occurrence of critical illness in patients hospitalized with COVID-19, according to a study in JAMA Internal Medicine. The score, which incorporates 10 variables recorded at admission, predicted a composite of ICU admission, invasive ventilation, or death with an area under the curve of 0.88. An online calculator is available.
 A small study in JACC: Cardiovascular Imaging suggests that MRI-assessed cardiac involvement is detected in a substantial proportion of patients even after they recover from COVID-19. “MRI manifestation included myocardial edema, fibrosis, and impaired RV function,” the researchers report.
A small study in JACC: Cardiovascular Imaging suggests that MRI-assessed cardiac involvement is detected in a substantial proportion of patients even after they recover from COVID-19. “MRI manifestation included myocardial edema, fibrosis, and impaired RV function,” the researchers report.
The COVID-19 pandemic has highlighted pre-existing racial/ethnic disparities in health and presented an opportunity to address their causes, researchers argue in a JAMA viewpoint. “Understanding the reasons for the initial reports of excess mortality and economic disruption related to COVID-19 among health disparity populations may allow the scientific, public health, and clinical community to efficiently implement interventions to mitigate these outcomes, particularly if substantial disease emerges in the fall of 2020 or beyond,” they write.
The US Food and Drug Administration has expedited clearance of updated ultrasound software by Caption Health to make it available during the COVID-19 pandemic. Caption Guidance is “the first and only artificial intelligence-guided medical imaging acquisition system,” according to a company press release. The company said US physicians reached out to the FDA to explain how the system “could enable rapid assessment of cardiac function, reduce the risk of exposure for personnel, and stretch limited resources in hospital emergency rooms and ICUs.”
In Morbidity and Mortality Weekly Report, public health officials from Washington state describe a “superspreading” event in which 87% of choir members developed COVID-19 after spending a 2-and-a-half-hour practice with a single symptomatic person. “Transmission was likely facilitated by close proximity (within 6 feet) during practice and augmented by the act of singing,” the researchers say. “The potential for superspreader events underscores the importance of physical distancing, including avoiding gathering in large groups, to control spread of COVID-19.”

May 12, 2020
 Autopsy data from Germany on a dozen patients who died from COVID-19 confirm that thromboembolic events are common and may be unsuspected at the time of death, as TCTMD’s L.A. McKeown reports. The data support the idea that some patients may need anticoagulation to prevent pulmonary embolism.
Autopsy data from Germany on a dozen patients who died from COVID-19 confirm that thromboembolic events are common and may be unsuspected at the time of death, as TCTMD’s L.A. McKeown reports. The data support the idea that some patients may need anticoagulation to prevent pulmonary embolism.
An analysis of data from New York City, published in Morbidity and Mortality Weekly Report (MMWR), suggests that COVID-19-related mortality may be worse than currently estimated. Of deaths reported to city health authorities between March 11 and May 2 that were found to be in excess of the seasonal expected baseline, 57% were in patients with confirmed COVID-19 and 21% were probably associated with COVID-19. The remaining 22% did not fall in either category, but “might have been directly or indirectly attributable to the pandemic,” the researchers say.
Worldwide collaboration will be needed to develop enough vaccine to protect the global population from SARS-CoV-2, according to “policy forum” in Science written by Anthony Fauci, MD, director of the US National Institute of Allergy and Infectious Diseases, and Francis Collins, MD, PhD, director of the US National Institutes of Health. “To return to a semblance of previous normality, the development of SARS-CoV-2 vaccines is an absolute necessity,” they say. “To achieve this goal, all the resources in the public, private, and philanthropic sectors need to participate in a strategic manner.”
A systematic review in Heart Rhythm delves into the arrhythmogenic effects of short courses of chloroquine and hydroxychloroquine in COVID-19 patients; about 10% developed QT prolongation. “Daily ECG monitoring and other risk mitigation strategies should be considered in order to prevent possible harms from what is currently an unproven therapy,” the authors conclude.
Handheld echocardiography may be useful for screening COVID-19 patients for related cardiac conditions, according to a study in the Journal of the American Society of Echocardiography. The scans were found to provide sufficient information for the clinical care team and to reduce sonographer scan time. “The protocol performed with handheld tablet ultrasound provides adequate diagnostic information of major cardiac complications of COVID-19 infection while decreasing sonographer contact and simplifying decontamination,” the researchers say.
New data from Italy published in the European Heart Journal confirm that COVID-19 patients with versus without cardiac disease have a greater risk of dying. They also experience higher rates of thromboembolic events and septic shock during the hospitalization.
In the Journal of the American College of Cardiology, James Kirkpatrick, MD, and colleagues review the allocation of resources and triage of patients during the COVID-19 pandemic. “These decisions should be guided by ethical principles and values, should not be made before crisis standards have been declared by authorities, and, in most cases, will not be made by bedside clinicians,” they say.
The degree of immunity that occurs among people who have recovered from COVID-19 remains an open question, as discussed in a JAMA viewpoint. “Understanding whether and how recovery from COVID-19 confers immunity to, or decreased severity of, reinfection is needed to inform current efforts to safely scale back population-based interventions, such as physical distancing,” Robert Kirkcaldy, MD, and colleagues note.
 The US Food and Drug Administration (FDA) has updated the question-and-answer section of its guidance for conducting clinical trials in the COVID-19 era: it “includes new content with considerations for using alternate laboratories or imaging centers, holding trial participant visits via video conference, and conducting required postmarketing clinical trials. The guidance also includes updated information about managing protocol deviations and amendments to ongoing trials, and about consulting with the FDA regarding administering investigational product infusions at home rather than at the clinical trial site.”
The US Food and Drug Administration (FDA) has updated the question-and-answer section of its guidance for conducting clinical trials in the COVID-19 era: it “includes new content with considerations for using alternate laboratories or imaging centers, holding trial participant visits via video conference, and conducting required postmarketing clinical trials. The guidance also includes updated information about managing protocol deviations and amendments to ongoing trials, and about consulting with the FDA regarding administering investigational product infusions at home rather than at the clinical trial site.”
Patients with chronic obstructive pulmonary disease (COPD) and current smokers have elevated risks of more severe COVID-19 and mortality compared with others, researchers report in PLOS ONE.
 Efforts to screen arriving international travelers in California “did not effectively prevent introduction of COVID-19” in that state during the initial phase of the outbreak, according to data in Morbidity and Mortality Weekly Report. “Monitoring travelers was labor-intensive and limited by incomplete information, volume of travelers, and potential for asymptomatic transmission,” the authors write. “Health departments need to weigh the resources needed for monitoring against those needed for implementing mitigation activities during the COVID-19 pandemic.”
Efforts to screen arriving international travelers in California “did not effectively prevent introduction of COVID-19” in that state during the initial phase of the outbreak, according to data in Morbidity and Mortality Weekly Report. “Monitoring travelers was labor-intensive and limited by incomplete information, volume of travelers, and potential for asymptomatic transmission,” the authors write. “Health departments need to weigh the resources needed for monitoring against those needed for implementing mitigation activities during the COVID-19 pandemic.”
May 11, 2020
 There have been reports of an increase in large-vessel strokes among younger patients accompanying surges in COVID-19 cases, although the lack of firm numbers has created uncertainty about whether it’s a true trend. Read my feature story delving into the issue here.
There have been reports of an increase in large-vessel strokes among younger patients accompanying surges in COVID-19 cases, although the lack of firm numbers has created uncertainty about whether it’s a true trend. Read my feature story delving into the issue here.
The American College of Cardiology (ACC) said that it will begin collecting COVID-19 data through its National Cardiovascular Data Registry (NCDR) Chest Pain-MI and CathPCI registries. The registries will record COVID-19 status for all patients, “and among affected patients, also collect key biomarkers that may reflect cardiac damage in COVID-19 patients, hospital events that may reflect complications of COVID-19, and COVID-19 therapies that may have cardiac effects,” according to a press release.
A 5-year-old boy in New York became the first child in the United States to die from an inflammatory syndrome reported to be associated with COVID-19, according to a story from NBC News. Two more children in the state have since died, the New York Times reports. The syndrome, which shares features with Kawasaki disease and toxic shock syndrome, is being increasingly recognized around the world.
The Society for Cardiovascular Angiography and Interventions (SCAI) virtual conference kicks off later this week. In addition to regular interventional cardiology sessions, the meeting will include several specifically related to COVID-19, touching on mechanical circulatory support, hypercoagulability and antithrombotic therapy, and TAVR in the context of the pandemic. Registration is free.
An antiviral cocktail may be beneficial in patients with mild-to-moderate COVID-19, results of a phase II trial published in the Lancet show. At six Hong Kong hospitals, patients given interferon beta-1b, lopinavir-ritonavir, and ribavirin had a significantly shorter time from the start of study treatment to a negative nasopharyngeal swab compared with those treated with lopinavir-ritonavir alone (median 7 vs 12 days).
The US Food and Drug Administration (FDA) has issued the first emergency use authorization for a COVID-19 antigen test to rapidly detect SARS-CoV-2, the agency announced over the weekend. The move applies to Quidel Corporation’s Sofia 2 SARS Antigen FIA. “This is just the first antigen test to be authorized and we expect more to follow,” the FDA said in a press release.
Might COVID-19 be sexually transmitted? Researchers report in JAMA Network Open that SARS-CoV-2 can be found in the semen of patients with COVID-19. “If it could be proved that SARS-CoV-2 can be transmitted sexually in future studies, sexual transmission might be a critical part of the prevention of transmission, especially considering the fact that SARS-CoV-2 was detected in the semen of recovering patients,” the authors write.
Again: These researchers did NOT check to see if the virus could be grown or cultured and if it was infectious. Urine and feces also test positive for RNA fragments like this, but virus cannot be cultured & it is not infectious. Please report accurately @CNN https://t.co/9ixkt3Cmlw
— C. Michael Gibson MD (@CMichaelGibson) May 9, 2020
The pandemic is hitting immigrant communities in the Bronx, NY, particularly hard, according to a viewpoint in JAMA Internal Medicine. “To address the ongoing outbreak, COVID-19 testing and treatment should be accessible to all patients and targeted as needed toward populations, such as immigrant communities, with elevated risk,” the authors say.
A trial sponsored by the US National Institute of Allergy and Infectious Diseases (NIAID) will evaluate whether adding the anti-inflammatory drug baricitinib to the investigational antiviral remdesivir is effective in treating COVID-19. The study is now enrolling adults hospitalized with COVID-19 in the United States, with a planned enrollment of more than 1,000.
 Tips for having important conversations with CVD patients during the COVID-19 pandemic can be found in a paper in Circulation. “During this pandemic, we are charged with rapidly learning about a new disease and communicating clearly and compassionately with our patients with CVD,” the authors write. “Using these communication strategies to strengthen the therapeutic relationship and identify goals of care is a critical part of caring for our patients.” They note that a nonprofit organization called VitalTalk has created a COVID-19 communication guide, which is available for free.
Tips for having important conversations with CVD patients during the COVID-19 pandemic can be found in a paper in Circulation. “During this pandemic, we are charged with rapidly learning about a new disease and communicating clearly and compassionately with our patients with CVD,” the authors write. “Using these communication strategies to strengthen the therapeutic relationship and identify goals of care is a critical part of caring for our patients.” They note that a nonprofit organization called VitalTalk has created a COVID-19 communication guide, which is available for free.
May 8, 2020
The specific mechanism remains unclear and the scope of the problem is still unknown, but something about the COVID-19 pandemic seems to be causing an uptick in Takotsubo cardiomyopathy, as reported by TCTMD’s Yael Maxwell.
 In the European Heart Journal: Acute Cardiovascular Care, Kurt Huber, MD, and Patrick Goldstein, MD, discuss the impact of COVID-19 on the care of patients with ACS. “This paper describes, besides general measures in times of a pandemic, also the necessary changes in the invasive diagnosis and treatment of patients presenting with different entities of acute coronary syndromes including structural adaptations (networks, spokes-and-hub centers) and therapeutic adjustments,” they write.
In the European Heart Journal: Acute Cardiovascular Care, Kurt Huber, MD, and Patrick Goldstein, MD, discuss the impact of COVID-19 on the care of patients with ACS. “This paper describes, besides general measures in times of a pandemic, also the necessary changes in the invasive diagnosis and treatment of patients presenting with different entities of acute coronary syndromes including structural adaptations (networks, spokes-and-hub centers) and therapeutic adjustments,” they write.
The US Food and Drug Administration issued an emergency use authorization for the first COVID-19 diagnostic test that uses at-home collection of saliva samples, manufactured by Rutgers Clinical Genomics Laboratory. “This provides an additional option for the easy, safe, and convenient collection of samples required for testing without traveling to a doctor’s office, hospital, or testing site,” FDA Commissioner Stephen Hahn, MD, said in a press release.
 The agency also issued a warning to healthcare workers alerting them about concerns that “certain filtering facepiece respirators from China may not provide consistent and adequate respiratory protection” from COVID-19 exposure.
The agency also issued a warning to healthcare workers alerting them about concerns that “certain filtering facepiece respirators from China may not provide consistent and adequate respiratory protection” from COVID-19 exposure.
Use of hydroxychloroquine in patients with COVID-19 is not associated with risk of intubation or death, according to an observational study in the New England Journal of Medicine. There remains a need for randomized trials of the drug, the authors state, noting that “clinical guidance at our medical center has been updated to remove the suggestion that patients with COVID-19 be treated with hydroxychloroquine.”
In a letter in NEJM, researchers report that use of stroke imaging dropped in the early stages of the pandemic, which “suggests a decrease in the number of evaluations both in patients with severe strokes and in nonelderly patients who may have been at low risk for COVID-19 complications.” Any reduction in care of patients with conditions like acute stroke “may be consequential because timely treatment may decrease the incidence of disability,” the authors note.
A retrospective study in the Lancet Rheumatology hints at a potential benefit of high-dose anakinra, a recombinant interleukin-1 receptor antagonist, in patients with COVID-19, moderate-to-severe acute respiratory distress syndrome, and hyperinflammation when added to hydroxychloroquine and ritonavir. The drug was associated with clinical improvement in 72% of patients.
Researchers make a call for equitable distribution of COVID-19 therapeutics and vaccines that get developed in a JAMA viewpoint. “If nations pursue a competitive race to develop effective vaccines and therapeutics, there will be only be losers, no winners,” they argue. “The threat posed by the novel coronavirus knows no borders. Only a well-coordinated global plan that harnesses the best science and delivers it to everyone in need can effectively counteract the COVID-19 scourge and future pandemics.”
According to a study in CMAJ, the spread of COVID-19 is not strongly related to latitude or temperature and is only weakly associated with humidity. Use of various public health interventions like restrictions on mass gatherings, school closures, and social distancing were strongly tied to reduced epidemic growth.
The US National Institutes of Health (NIH) has launched an online survey to examine the impact of COVID-19 on the roughly 30 million people living with rare diseases in the United States, as well as their families and caregivers.
May 7, 2020
Anticoagulation may improve outcomes among certain patients with COVID-19, according to research out of New York City. As reported by TCTMD’s Caitlin Cox, anticoagulation was associated with a lower rate of in-hospital mortality among patients on mechanical ventilation (29.1% vs 62.7%). Investigator Valentin Fuster, MD, PhD, stressed that the observational study will be followed by larger, more rigorous analyses. Still, it’s an important step in an ongoing project, he added.
 Investigators are looking into a possible link between COVID-19 and Kawasaki disease in children, TCTMD Managing Editor Shelley Wood reports. The Royal College of Paediatrics and Child Health in the United Kingdom and New York City’s department of health have issued alerts. The American Heart Association (AHA) has also weighed in. “We want to reassure parents—this appears to be uncommon. While Kawasaki disease can damage the heart or blood vessels, the heart problems usually go away in 5 or 6 weeks, and most children fully recover,” said Jane Newburger, MD, a member of the AHA’s Young Hearts Council.
Investigators are looking into a possible link between COVID-19 and Kawasaki disease in children, TCTMD Managing Editor Shelley Wood reports. The Royal College of Paediatrics and Child Health in the United Kingdom and New York City’s department of health have issued alerts. The American Heart Association (AHA) has also weighed in. “We want to reassure parents—this appears to be uncommon. While Kawasaki disease can damage the heart or blood vessels, the heart problems usually go away in 5 or 6 weeks, and most children fully recover,” said Jane Newburger, MD, a member of the AHA’s Young Hearts Council.
In the European Heart Journal, researchers describe a case involving an 82-year-old man with acute respiratory distress syndrome due to SARS-CoV-2 infection that was complicated by STEMI and pulmonary embolism. “Treatment of COVID-19 requires multidisciplinary expertise to address the multifaceted clinical manifestations of this viral disease,” they write. “Moreover, careful attention to interactions between antiviral and other medications including oral and intravenous anticoagulants should be considered in COVID-19 patients with need for anticoagulation to minimize the risk of bleeding and thromboembolic complications.”
A review in the European Heart Journal: Acute Cardiovascular Care addresses the cardiac safety of off-label COVID-19 therapies, including chloroquine and hydroxychloroquine, antivirals, monoclonal antibodies, and common antibiotics. “The article focuses on practical points and offers a point-of-care protocol for providers who are taking care of patients with COVID-19 in an inpatient and outpatient setting,” the authors write. “The proposed protocol is taking into consideration that resources during the pandemic are limited.”
The Cardiovascular Research Foundation’s Interventional Complications conference, scheduled for August 7 to 8 in Seattle, WA, has been cancelled due to the continuing COVID-19 pandemic.
The COVID-19 era presents some tricky scenarios when it comes to performing CPR, according to a perspective in the New England Journal of Medicine. States and hospitals need to develop explicit and ethical crisis standards of care, which “will help clinicians define and understand when strict adherence to established resuscitation protocols may no longer be appropriate,” the authors say.
 In an NEJM correspondence, researchers state that “acute cor pulmonale causing obstructive shock should be included in the differential diagnosis in critically ill patients with COVID-19” after describing the course of five patients with confirmed infection who had “profound hemodynamic instability and cardiac arrest with acute right ventricular failure.”
In an NEJM correspondence, researchers state that “acute cor pulmonale causing obstructive shock should be included in the differential diagnosis in critically ill patients with COVID-19” after describing the course of five patients with confirmed infection who had “profound hemodynamic instability and cardiac arrest with acute right ventricular failure.”
How should patients who have recovered from COVID-19, as shown by positive antibody tests, be handled? Some countries are considering issuing immunity certifications or passports to such people, which would allow the holders additional freedoms to move around. Two viewpoints in JAMA—one by Govind Persad, JD, PhD, and Ezekiel Emanuel MD, PhD, and the one by Mark Hall, JD, and David Studdert, LLB, ScD—tackle the issues involved with such an approach. “Such policies raise important questions about fairness, stigma, and counterproductive incentives but could also further individual freedom and improve public health,” Persad and Emanuel write.
In another JAMA viewpoint, researchers describe how to interpret two commonly used tests for diagnosing SARS-CoV-2 infection—reverse transcriptase–polymerase chain reaction (RT-PCR) and IgM and IgG enzyme-linked immunosorbent assay (ELISA). They also include a figure illustrating how the test results vary over time relative to symptom onset.
Merlin Chowkwanyun, PhD, and Adolph Reed Jr, PhD, caution against examining racial health disparities during the COVID-19 pandemic without the appropriate context. “In sum, to mitigate myths of racial biology, behavioral explanations predicated on racial stereotypes, and territorial stigmatization, COVID-19 disparities should be situated in the context of material resource deprivation caused by low socioeconomic status, chronic stress brought on by racial discrimination, or place-based risk,” they write in a perspective in NEJM.
May 6, 2020
A case series out of the Lombardy region of Italy shows that many patients with STEMI and COVID-19—nearly 40%—do not have obstructive coronary disease on angiography. The finding supports anecdotal reports of STEMI mimics during the pandemic but not a role for fibrinolysis, according to investigator Giulio Stefanini, MD, PhD.
 The New England Journal of Medicine released a series of papers addressing the impact of ACE inhibitors and ARBs in COVID-19, and the findings are reassuring. As reported by TCTMD’s Michael O’Riordan, use of the drugs does not seem to increase susceptibility to developing COVID-19 or to having more severe forms of the disease if they get it.
The New England Journal of Medicine released a series of papers addressing the impact of ACE inhibitors and ARBs in COVID-19, and the findings are reassuring. As reported by TCTMD’s Michael O’Riordan, use of the drugs does not seem to increase susceptibility to developing COVID-19 or to having more severe forms of the disease if they get it.
In a related study published in JAMA Cardiology, researchers found that patients taking an ACE inhibitor or ARB were not more likely to test positive for COVID-19. “These clinical data support current professional society guidelines to not discontinue ACE inhibitors or ARBs in the setting of the COVID-19 pandemic,” they say. Secondary analyses in patients who tested positive hinted at the possibility that the severity of disease was greater in users of the drugs, but editorialists urged caution in interpreting those findings.
The 2020 European Society of Cardiology Congress, scheduled to take place in Amsterdam at the end of the summer, has officially been cancelled after the government of the Netherlands banned all public gatherings before September. There will be virtual offerings each day between August 29 and September 1.
A study released as a preprint on BioRxiv by researchers at the Los Alamos National Laboratory suggests that dominant strain of SARS-CoV-2 currently spreading across the United States is more transmissible than the strain that initially emerged in Wuhan, China.
In a letter to the editor of NEJM, researchers discuss lupus anticoagulant and abnormal coagulation tests in patients with COVID-19. The takeaway? “We suggest that a prolonged activated partial-thromboplastin time should not be a barrier to the use of anticoagulation therapies in the prevention and treatment of venous thrombosis in patients with COVID-19,” they advise.

An international panel of experts provides practical recommendations for the management of diabetes in patients with COVID-19 in the Lancet Diabetes & Endocrinology. Preliminary data collected during the pandemic indicate that risk of death is up to 50% higher in patients with diabetes.
In Heart & Lung, researchers delve into considerations for critical care nursing research and practice that are arising during the COVID-19 pandemic. “One thing is for certain: now more than ever, the holistic view and diverse expertise of critical care nurses are needed to provide a beacon of hope in this 2020 ‘Year of the Nurse,’” they write.
A new approach will be needed to deliver surgical services in Canada and deal with the backlog in the aftermath of the COVID-19 pandemic, researchers argue in CMAJ. They advocate a combination of single-entry models and team-based care, which is “an efficient, fair, and ethical approach to addressing the pent-up demand for surgery in the presence of constrained resources.”
In the BMJ, experts describe the best ways to reduce risks of SARS-CoV-2 transmission in the home. “Evidence from controlled experiments in animal models, viral genome studies, and other epidemics suggests the infecting viral load may be important,” they note. Efforts detailed on the Germ Defence website, including handwashing and cleaning, avoiding sharing rooms and surfaces, managing incoming deliveries, and ventilating rooms, could be key in controlling spread, they say.
May 5, 2020
A study out of Wuhan, China, has shown that evidence of right heart dysfunction, particularly RV longitudinal strain on two-dimensional speckle-tracking echocardiography, is strongly associated with increased mortality in patients with COVID-19, as reported by TCTMD’s Caitlin Cox.
 Though it’s been anticipated due to the French government’s prohibition on public gatherings of more than 5,000 people, EuroPCR has officially been cancelled. “We remain committed to working with our program committee to swiftly provide the community with a full update on late-breaking trials and other essential educational content,” the course directors said. “Details of the dates and platform upon which this independent medical education will be delivered shall be made known in the coming weeks.”
Though it’s been anticipated due to the French government’s prohibition on public gatherings of more than 5,000 people, EuroPCR has officially been cancelled. “We remain committed to working with our program committee to swiftly provide the community with a full update on late-breaking trials and other essential educational content,” the course directors said. “Details of the dates and platform upon which this independent medical education will be delivered shall be made known in the coming weeks.”
Likewise, the 2020 meeting of the Society of Cardiovascular Computed Tomography (SCCT), originally scheduled for the middle of July in Seattle, WA, will now be held virtually on July 17 and 18 due to COVID-19-related concerns.
The New York City Health Department has issued a health alert about a pediatric multisystem inflammatory syndrome potentially associated with COVID-19 after 15 cases were identified in city hospitals. The condition is characterized by persistent fever and features of Kawasaki disease and/or toxic shock syndrome. Similar reports have popped up around the world.
A perspective in Circulation addresses the racial/ethnic disparities in terms of hospitalizations, deaths, and infections related to COVID-19, with African Americans, Hispanics, and Native Americans feeling the effects of the pandemic more than other groups. The authors offer some solutions before concluding, “Our vulnerable interconnectedness highlighted by the COVID-19 pandemic should ignite meaningful solution-focused collaborations among community leaders, scholars and policymakers to orchestrate sustainable change aimed at addressing pervasive healthcare disparities.”
In the American Heart Journal, physicians from Duke University Medical Center released the care pathway they developed to deal with the cardiovascular complications of COVID-19. “The model presented can provide a framework for other institutions to organize their own approaches and can be adapted to local constraints, resource availability, and emerging knowledge,” they say.
That same journal also recently published a review of COVID-19 for the cardiovascular specialist and an editorial discussing how to anticipate and curtail the cardiometabolic toxicity of social isolation and emotional stress during the pandemic.
It’s possible that drones could be one solution to the problem of declining bystander CPR rates in patients with out-of-hospital cardiac arrest related to fear of contracting SARS-CoV-2, according to a letter to the editor of Resuscitation. “Aside from providing automated external defibrillator and CPR advice to bystanders, drones can deliver personal protective equipment and communicate safety instructions,” researchers say. “Although this seems a logistical challenge, it can be a crucial part of the strategy to encourage, instruct, and reassure bystanders to perform CPR even in times of epidemic.”
 What impact will the COVID-19 pandemic have on the financial health of US hospitals? Dhruv Khullar, MD, tackle that question in a JAMA viewpoint. “In the absence of robust and sustained governmental support, almost all hospitals will experience financial difficulties,” they predict. “But hospitals that are smaller, independent, rural, and have critical access status are particularly at risk. Policymakers should provide dedicated support to these hospitals to access CARES Act funds and consider allocating additional funding to them during the COVID-19 pandemic.”
What impact will the COVID-19 pandemic have on the financial health of US hospitals? Dhruv Khullar, MD, tackle that question in a JAMA viewpoint. “In the absence of robust and sustained governmental support, almost all hospitals will experience financial difficulties,” they predict. “But hospitals that are smaller, independent, rural, and have critical access status are particularly at risk. Policymakers should provide dedicated support to these hospitals to access CARES Act funds and consider allocating additional funding to them during the COVID-19 pandemic.”
In an editorial in JAMA, Howard Bauchner, MD, and Phil Fontanarosa, MD, discuss the challenges that will come from interpreting the results of clinical trials of COVID-19-related therapies. “Because much of the focus is now on preventing recurrence of the pandemic, it will be important for investigators, journals, and the media to accurately report the results of the studies responsibly and what they mean both for individuals and for population health,” they write.
Healthcare workers have a responsibility to address intimate partner violence (IPV), which has reportedly increased during the COVID-19 pandemic, researchers argue in CMAJ. “Healthcare providers, although facing the need to learn many new skills related to COVID-19, must also maintain awareness of IPV, seek opportunities for self-education, develop strategies for discussing IPV and become familiar with currently available local resources for patient referral,” they say.
May 4, 2020
 There was a “terrible” spike in cardiac arrest deaths during the COVID-19 surge in the Lombardy region of Italy, TCTMD Managing Editor Shelley Wood reports based on a research letter in the New England Journal of Medicine. The numbers appear to corroborate concerns that patients with STEMI symptoms—with or without COVID-19—are afraid to go to the hospital.
There was a “terrible” spike in cardiac arrest deaths during the COVID-19 surge in the Lombardy region of Italy, TCTMD Managing Editor Shelley Wood reports based on a research letter in the New England Journal of Medicine. The numbers appear to corroborate concerns that patients with STEMI symptoms—with or without COVID-19—are afraid to go to the hospital.
The NEJM also recently published a series of papers informing the investigation into the impact of renin-angiotensin-aldosterone system blockers on COVID-19 risk, one by Mandeep Mehra, MD, et al, one by Giuseppe Mancia, MD, et al, and one by Harmony Reynolds, MD, et al. “All are observational studies with the looming possibility of confounding, but each has unique strengths, and their message is consistent—none of the three studies showed evidence of harm with continued use of ACE inhibitors and ARBs,” John Jarcho, MD, et al, write in an accompanying editorial.
Multisociety guidance aims to provide a framework for the safe reintroduction of cardiovascular services that have been interrupted due to the COVID-19 pandemic. “As regions move along the journey of managing the COVID-19 pandemic, there is an opportunity to reintroduce regular cardiovascular care in a progressive manner with appropriate safeguards,” the authors write.
 The American Heart Association (AHA) has released temporary emergency guidance to STEMI systems of care during the COVID-19 pandemic. “Regionalization of STEMI care is perhaps more important than ever. Communication between hospitals and EMS and inter-facility transport providers in a region, sharing protocols and resources, data and experiences may prove critically important. Usual monthly review meetings should continue through the pandemic, in a virtual format, to review regional performance and opportunities for improvement,” the authors write.
The American Heart Association (AHA) has released temporary emergency guidance to STEMI systems of care during the COVID-19 pandemic. “Regionalization of STEMI care is perhaps more important than ever. Communication between hospitals and EMS and inter-facility transport providers in a region, sharing protocols and resources, data and experiences may prove critically important. Usual monthly review meetings should continue through the pandemic, in a virtual format, to review regional performance and opportunities for improvement,” the authors write.
On Friday, the US Food and Drug Administration (FDA) issued an emergency use authorization for the investigational antiviral remdesivir after a trial run by the US National Institute of Allergy and Infectious Diseases (NIAID) showed the drug shortened the time to recovery compared with placebo.
In Morbidity and Mortality Weekly Report, Anne Schuchat, MD, and the COVID-19 response team of the US Centers for Disease Control and Prevention (CDC) detail the public health response to the initiation and spread of SARS-CoV-2 in the United States through April 21. Multiple factors contributed to the spread, they say, “including continued travel-associated importations, large gatherings, introductions into high-risk workplaces and densely populated areas, and cryptic transmission resulting from limited testing and asymptomatic and presymptomatic spread.” Preventing future spread will require “sustained and concerted efforts.”
The European Medicines Agency (EMA) has published an overview of how it will be accelerating its regulatory procedures to speed the development of safe and effective medications for COVID-19.
 David Cutler, PhD, and colleagues discuss the business of medicine in the COVID-19 era in a viewpoint in JAMA. “It is possible, perhaps likely, that the painful process of reaching a new healthcare equilibrium will last well into 2021,” they say. “Ideally, this time will allow for thoughtful discussion of how the intertwined forces currently affecting clinicians and other healthcare personnel, as well as hospitals, healthcare centers, and practices, can lead to sustained improvement of the overall system for delivering care.”
David Cutler, PhD, and colleagues discuss the business of medicine in the COVID-19 era in a viewpoint in JAMA. “It is possible, perhaps likely, that the painful process of reaching a new healthcare equilibrium will last well into 2021,” they say. “Ideally, this time will allow for thoughtful discussion of how the intertwined forces currently affecting clinicians and other healthcare personnel, as well as hospitals, healthcare centers, and practices, can lead to sustained improvement of the overall system for delivering care.”
Unsure of how to lessen fear and suffering among COVID-19 patients isolated in the ICU and their families? Kathleen Akgün, MD, et al provide some communication strategies that might work in Heart & Lung.
May 1, 2020
 The American Society for Preventive Cardiology (ASPC) has released a scientific statement on continuity of care and outpatient management during the COVID-19 pandemic for patients who have or are at high risk for cardiovascular disease. “Several strategies are available to ensure ongoing care, including preventive measures, and we aim to highlight these strategies in this document,” ASPC President Amit Khera, MD, said in a press release.
The American Society for Preventive Cardiology (ASPC) has released a scientific statement on continuity of care and outpatient management during the COVID-19 pandemic for patients who have or are at high risk for cardiovascular disease. “Several strategies are available to ensure ongoing care, including preventive measures, and we aim to highlight these strategies in this document,” ASPC President Amit Khera, MD, said in a press release.
In a research letter in Circulation, investigators report on clinical and angiographic outcomes among STEMI patients with COVID-19 who were treated in the Lombardy region of Italy, one of the hardest hit parts of the world. For most patients (85.7%), STEMI was the first clinical manifestation of the viral infection. Angiography showed that a large minority (39.3%) had no culprit lesion.
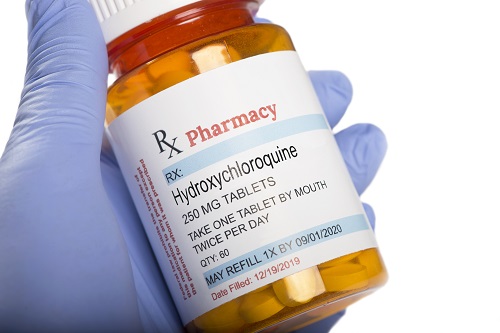 Two new reports in JAMA Cardiology—one out of Boston and one from France—assess the risk of QT interval prolongation associated with use of hydroxychloroquine with or without azithromycin to treat COVID-19. The findings, combined with some prior data, “underscore the potential risk associated with widespread use of hydroxychloroquine and the combination of hydroxychloroquine and azithromycin in ambulatory patients with known or suspected COVID-19,” Robert Bonow, MD, Adrian Hernandez, MD, and Mintu Turakhia, MD, write in an accompanying editorial. “Understanding whether this risk is worth taking in the absence of evidence of therapeutic efficacy creates a knowledge gap that needs to be addressed.”
Two new reports in JAMA Cardiology—one out of Boston and one from France—assess the risk of QT interval prolongation associated with use of hydroxychloroquine with or without azithromycin to treat COVID-19. The findings, combined with some prior data, “underscore the potential risk associated with widespread use of hydroxychloroquine and the combination of hydroxychloroquine and azithromycin in ambulatory patients with known or suspected COVID-19,” Robert Bonow, MD, Adrian Hernandez, MD, and Mintu Turakhia, MD, write in an accompanying editorial. “Understanding whether this risk is worth taking in the absence of evidence of therapeutic efficacy creates a knowledge gap that needs to be addressed.”
The American Heart Association (AHA) has distributed $1.2 million in grants to investigators at 12 US centers for fast-tracked studies of the cardiovascular and cerebrovascular effects of COVID-19. Among the projects: a team from Columbia University Irving Medical Center in New York City will examine arterial and venous thrombotic complications in patients with COVID-19, while a group from Kaiser Permanente Southern California will look into risks of severe morbidity and mortality related to COVID-19 in patients taking antihypertensive medications.
New data on adults hospitalized for COVID-19 in Georgia published in Morbidity and Mortality Weekly Report show that African-Americans were overrepresented—but had outcomes similar to those of other patients—and that roughly one-quarter of the overall cohort did not have any recognized risk factors for severe disease. “Prevention activities should prioritize communities and racial groups most affected by severe COVID-19,” the authors write. “Increased awareness of the risk for serious illness among all adults, regardless of underlying medical conditions or age, is needed.”
The National Aeronautics and Space Administration (NASA) is bringing its engineering expertise to the COVID-19 fight. It has developed a ventilator—called NASA VITAL—specifically for patients with COVID-19, and it is intended to last 3 to 4 months. The US Food and Drug Administration (FDA) has included the device under its ventilator emergency use authorization.
Convalescent plasma is an old solution for a new problem, as Rita Rubin, MA, describes in JAMA. Rubin takes readers through the history of its use and how its being applied and tested for the treatment of COVID-19.
 The European Medicines Agency (EMA) has initiated a rolling review of the investigational antiviral remdesivir for COVID-19 after the release of mixed clinical trial results. “The start of the rolling review only means that the evaluation of remdesivi r has started and does not imply that its benefits outweigh its risks,” the agency explained, noting that a rolling review can “speed up the assessment of a promising investigational medicine during a public health emergency, such as the ongoing pandemic.”
The European Medicines Agency (EMA) has initiated a rolling review of the investigational antiviral remdesivir for COVID-19 after the release of mixed clinical trial results. “The start of the rolling review only means that the evaluation of remdesivi r has started and does not imply that its benefits outweigh its risks,” the agency explained, noting that a rolling review can “speed up the assessment of a promising investigational medicine during a public health emergency, such as the ongoing pandemic.”
COVID-19: TCTMD's Daily Dispatch for September
COVID-19: TCTMD’s Daily Dispatch for August
COVID-19: TCTMD’s Daily Dispatch for July
COVID-19: TCTMD’s Daily Dispatch for June
COVID-19: TCTMD’s Daily Dispatch for April
COVID-19: TCTMD’s Daily Dispatch for March
Todd Neale is the Associate News Editor for TCTMD and a Senior Medical Journalist. He got his start in journalism at …
Read Full Bio

Comments